Abstract
Glucocorticoids remain widely used for many medical conditions, and fractures are the most serious common adverse event related to long-term glucocorticoid use. Glucocorticoid-induced osteoporosis (GIOP) develops in a time- and dose-dependent manner, but even at low doses, an increased risk of fragility fracture may be observed even within the first month of treatment. GIOP is mediated by multiple pathophysiologic mechanisms resulting in an inhibition of bone formation and an increase in bone resorption. The clinical assessment of GIOP has potential pitfalls since dual-energy X-ray absorptiometry (DXA) may underestimate the risk of fracture in patients treated with glucocorticoids. Many national organizations have developed guidelines for assessing fracture risk and treating patients with, or at risk for, GIOP. These groups advocate both antiresorptive agents and bone-forming agents based predominately on their efficacy in improving bone mineral density. Oral bisphosphonates are generally the first-line therapy for GIOP in most patients due to their proven efficacy, good safety, and low cost. For those patients at greater risk of fracture, teriparatide should be considered earlier, based on its ability to significantly reduce vertebral fractures when compared with alendronate. GIOP remains a major public health concern that is at least partially preventable with current and potential future therapeutic options.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiology and clinical burden of GIOP
Glucocorticoid-induced osteoporosis (GIOP) is the most common form of secondary osteoporosis. Glucocorticoids are used chronically by approximately 0.5–1% of the general population [1,2,3]. Glucocorticoids remain widely prescribed for many medical conditions by specialists and particularly by generalists [1,2,3]. Fractures are the most serious adverse event related to chronic glucocorticoid use [4]. Glucocorticoid use is associated with an increase of fragility fracture risk quickly following the first dose [5], leading to an “imminent risk of fracture,” [6]. However, the risk of fracture also increases depending on dosage and length of use; the longer and the more intense the treatment, the higher the risk [7,8,9,10]. Compared with shorter-course users, heavy users (daily dose ≥ 15 mg prednisone equivalent and/or cumulative dose ≥ 1 g) have the greatest risk of fractures [7]. The annual incidence of vertebral and non-vertebral fracture from the control arms of glucocorticoid-induced osteoporosis clinical trials was 5.1% among the patients chronically using glucocorticoids and 2.5% in those who were newly initiating glucocorticoids [5].
Burden of GIOP in specific glucocorticoid-requiring diseases
Glucocorticoids are prescribed for the treatment of many chronic diseases affecting patients of different ages, sexes, and ethnicities. Glucocorticoids lead to bone loss and eventually fragility fractures; however, they might also serve a protective role by reducing inflammation associated with an underlying disease. For this reason, it is important to consider the major glucocorticoid-requiring conditions separately. Rheumatoid arthritis appears to constitute the disease that is most often associated with chronic glucocorticoid use. The fracture incidence rate in persons affected by rheumatoid arthritis was higher in patients taking doses of glucocorticoids greater or equal than 15 mg/day prednisone equivalents (16.0 per 1000 person-year) compared with those who were taking doses less than 15 mg/day (5 to 9 per 1000 person-years). In rheumatoid arthritis patients, after discontinuation of glucocorticoids, the fracture incidence returned to baseline levels only after 12 months [8]. Patients with polymyalgia and giant cell arteritis (diseases primarily observed in older Caucasians) had incidence fracture rates approximately 14.5 per 1000 person-years, and the risk of fracture was increased by approximately 65% compared with the control populations, an effect largely attributable to the use of glucocorticoids [11]. In systemic lupus erythematosus (SLE) (a disease predominately affecting young women and more prevalent in non-Hispanic blacks), there was a 20% increased clinical fracture risk compared to controls [12]. This result was mainly ascribable to chronic glucocorticoids, based on an earlier evaluation of approximately 6000 person-years of follow-up [13]. More than 3% of diabetic patients reported chronic use of glucocorticoids with a corresponding fracture prevalence greater than 30% [14]. In patients with chronic obstructive pulmonary disease (COPD) and asthma, there was an increased risk of osteoporosis [15]. This observed increased risk was associated with several factors such as cigarette smoking, systemic inflammation, and less activity but also with the use of oral glucocorticoids [16]. The independent role of inhaled glucocorticoids is difficult to discern since most COPD and asthma patients receive periodic bursts of oral or parenteral glucocorticoids [17]. A Cochrane systematic review on the effect inhaled glucocorticoids have on bone metabolism showed neither evidence of increased risk of fracture nor loss of BMD with conventional doses of inhaled glucocorticoids given for 2 or 3 years [18]. However, a longer duration of treatment (> 8 years) and greater mean daily dose (> 600 μg/day of beclomethasone or equivalent) resulted in an increased risk of fragility fractures [19, 20].
Observations
The pathogenesis and molecular basis of GIOP
Glucocorticoids exert a direct toxic effect on bone cell–regulating genes (e.g., osteoblasts) by binding to the promoter region of glucocorticoid response elements, ultimately leading to altered protein synthesis and regulation. 11β-Hydroxysteroid dehydrogenase converts hormonally active glucocorticoids to inactive hormone forms; polymorphism of this enzyme may help explain altered susceptibility to glucocorticoid toxicity [21]. Glucocorticoids produce a direct deleterious effect on bone formation through two primary pathways: first, via enhancement of peroxisome proliferator-activated receptor gamma receptor 2 (PPARγ2) expression [22] and second, through inhibition of the canonical Wnt/β-catenin signaling pathway [23]. Glucocorticoids enhance expression of Wnt antagonists, sclerostin (SOST), and dickkopf-related protein 1 (Dkk1), resulting in decreased production of osteoblasts and ultimately less bone formation; thus, Wnt signaling plays a central role in the pathogenesis of GIOP [24]. There is augmented osteoblast death which appears to also depend on an increased release of reactive oxygen species (ROS) [25]. Moreover, glucocorticoids directly reduce the production of growth hormone (GH) and insulin-like growth factor (IGF1), both osteoblast stimulators [26]. In addition to their inhibitory effect on bone formation, glucocorticoids also affect bone resorption. Glucocorticoids increase the production of receptor activator of nuclear factor kappa-Β ligand (RANKL) and decrease the production of osteoprotegerin, resulting in enhanced bone resorption. RANKL expression is augmented directly not only by glucocorticoids but also by an increase in Dkk1 [27]. Glucocorticoids stimulate the secretion of interleukin-6 (IL-6), a cytokine that increases osteoclastogenesis and suppresses interferon-β an osteo-stimulating cytokine [28, 29]. The overall effect of glucocorticoids on bone resorption leads to bone loss, particularly early during the course of therapy. The effect of glucocorticoids on bone is not only driven by osteoclasts and osteoblasts but also by osteocytes [30]. Glucocorticoids impair the function of osteocytes and stimulate their apoptosis. The loss of osteocyte function leads to impaired bone architecture [31, 32] that could explain the bone mineral density (BMD)/fragility paradox; namely, that patients on glucocorticoid experience fracture at higher BMD compared with the general population [33]. Glucocorticoids induce hypogonadism through inhibition of estrogens and androgens, but without a clear bone effect. Glucocorticoids also have a deleterious effect on muscle strength resulting in increased risk of fall and subsequently, an increased risk of fracture [34]. Lastly, glucocorticoids might influence calcium homeostasis, but this effect remains controversial. There is some evidence that glucocorticoid inhibits calcium absorption in the intestinal tract, but other studies showed no decrement in calcium serum levels or a parathyroid hormone (PTH) increase [35]. These discordant reports may be related to the variability of vitamin D insufficiency prevalence in patients on glucocorticoids. Moreover, the renal handling of calcium and phosphate is also controversial due to the variable underlying conditions that can have independent effects on renal mineral excretion (e.g., sarcoidosis). In chronic glucocorticoid use, calcium net excretion increases due in part to mobilization of skeletal calcium. This perturbed mineral homeostasis may increase PTH secretion with the development of secondary hyperparathyroidism. Young healthy men who were administered 50 mg/day of prednisone for up to 6 months did not experience an increase in PTH nor a decrease in serum calcium [35]. Given the conflicting evidence to date, it is unlikely that changes in bone mineral homeostasis play a significant role in GIOP. In summary, GIOP differs substantially from postmenopausal osteoporosis in terms of pathophysiological mechanisms and time course. Patients on glucocorticoids have reduced bone formation, enhanced bone resorption, impaired bone architecture and experience fractures earlier than postmenopausal osteoporosis.
Non-pharmacologic treatment options for GIOP: calcium and vitamin D
Sufficient calcium and vitamin D are critical for the prevention and treatment of GIOP, particularly in light of the calciuria that may occur early with glucocorticoid use. Meta-analyses showed a reduction of fracture rate in patients treated with alfacalcidol and calcitriol compared with a placebo [36, 37]. Despite these results, the use of calcium and vitamin D supplements alone for fracture preventions is controversial in osteoporosis overall and inferior to bisphosphonate treatment for GIOP [37].
Pharmacologic treatment options for GIOP
To date, six large randomized clinical trials on pharmacologic or biologic therapies for GIOP have been conducted. These clinical trials provide key information about GIOP therapy, but comparisons within and between studies are limited due to study design heterogeneity including variability in study subject age, menopausal status, underlying conditions, comorbidities, cotherapies, and baseline bone mass status and previous history of fractures. Another important difference between and within studies resides in a “prevention” vs “treatment” designation, referring to whether the study subject is a new or prevalent user of glucocorticoids, respectively. For example, a clinical trial of alendronate compared with placebo [38] had 53% post-menopausal women compared with a clinical trial evaluating teriparatide vs alendronate where 83% of women were post-menopausal [39]. Furthermore, the underlying condition that required glucocorticoids differed in the alendronate trial, 19% of the patients were affected by SLE and 30% by rheumatoid arthritis [38] compared with 8% and 40%, respectively, in a risedronate trial [40]. Baseline prevalence of vertebral fracture also differed 15% fracture rate in the treatment arm of the alendronate trial [38] compared with a 30% fracture rate in the risedronate trial [41].
Bisphosphonates
Similar to post-menopausal osteoporosis, bisphosphonates are the most widely used therapy in GIOP, and a number of studies have assessed their efficacy (Table 1). Oral alendronate (5/10 mg once a day or 70 mg once weekly) [38, 42, 43], risedronate (5 mg once a day or 35 mg once weekly) [40, 41, 44, 45], ibandronate (150 mg PO monthly or 2–3 mg IV every 3 months) [46,47,48], and zoledronic acid (5 mg IV once every year) [49] are all efficacious for treating GIOP. All four bisphosphonates increased lumbar spine and hip BMD more than placebo, or for zoledronic acid compared with risedronate and for ibandronate compared with alfacalcidol.
Alendronate
In the pivotal clinical trial comparing daily oral alendronate to placebo [38] after 48 weeks, alendronate improved lumbar spine BMD by 2.9% compared with the baseline while with placebo BMD was reduced by 0.4%. In a 12-month randomized, placebo-controlled clinical trial, weekly alendronate appeared largely similar in effects on BMD to daily in GIOP [43]. Alendronate, risedronate, and ibandronate have all shown at least preliminary evidence for vertebral fracture prevention [38, 41, 44,45,46]. There was a trend towards vertebral fracture risk reduction in the first year of the pivotal alendronate study and 90% significant reduction of vertebral fracture risk in the open-label extension study at 2 years [42]. While non-vertebral fractures were far too few in number to draw conclusions from GIOP-randomized clinical trials, observational data from a Swedish national database demonstrated that alendronate significantly reduced the risk of hip fracture (HR 0.35, 95% CI, 0.22–0.54) [50].
Risedronate
Risedronate increased the lumbar spine BMD by 3.4% compared with placebo but only by 0.6% compared with baseline [41]. Another study evaluating risedronate in GIOP patients with lower baseline BMD showed an improvement of 2.9% on lumbar spine BMD within 1 year compared with baseline [44]. These clinical trials were conducted in parallel, under similar protocols but were then combined for aggregate analysis [45]. In the combined analysis, the overall vertebral fracture risk reduction with risedronate was 70% versus placebo (p = 0.01).
Ibandronate
Ibandronate prevented bone loss associated with glucocorticoid use [46,47,48], and in a high-risk cohort of cardiac transplanted patients treated with 15 mg/day of prednisone equivalent, ibandronate reduced fracture risk by 75% after 12 months compared with placebo [48].
Zoledronic acid
Zoledronic acid improved BMD to a greater extent than risedronate but failed to achieve direct evidence of fracture prevention, possibly due to a low fracture rate in the population under analysis in an active comparator study that did not require a BMD inclusion criteria [49].
A 2016 meta-analysis on bisphosphonates for GIOP included 27 randomized controlled trials containing 3075 patients [51]. In this analysis, 7.7% of people experienced a new vertebral fracture in the control arm compared with 4.4% in the bisphosphonate arm; overall fracture risk reduction was 43% with bisphosphonates (95% CI, 9.0 to 65.0%).
Bisphosphonates are relatively safe, well-tolerated drugs. The risk of osteonecrosis of the jaw and atypical femur fractures remains exceedingly low; however, there are anecdotal reports of these rare events and a theoretical concern that in a low turnover state such as GIOP these problems might be accentuated [52,53,54]. Indeed, glucocorticoid use has been associated with an increased risk of osteonecrosis of the jaw [55]. Compelling data on these safety signals are lacking from GIOP clinical trials due to the comparatively small number of patients included in these studies.
Denosumab
A randomized double-blind, double-dummy, active-controlled study on the use of denosumab versus risedronate in GIOP [56] showed greater BMD at lumbar spine compared to risedronate in both glucocorticoid-continuing (4.4% vs 2.3%) and glucocorticoid-initiating (3.8% vs 0.8%) subpopulations. Serious infections were similar in the two groups, although the study was underpowered for this safety outcome. Of the 17 patients in the denosumab group who were also taking concomitant biologic medications for inflammatory diseases, none experienced serious infection compared with two (7%) in the risedronate group. There was no difference between treatment arms in fracture outcomes. One concern of particular special relevance to GIOP is the possible increase in vertebral fracture after stopping denosumab [57, 58], particularly since these patients are younger and may discontinue glucocorticoid at some point. Thus, how to prescribe and manage denosumab (when to stop and what to follow it with) in those who stop glucocorticoids requires pre-planning, and further studies are needed to evaluate the efficacy of possible discontinuation strategies.
Teriparatide
Teriparatide is an attractive therapeutic option for patients affected by GIOP due to its anabolic mechanism of action and the pathophysiologic considerations in GIOP discussed above. Rats treated with both PTH and glucocorticoids had only a partial inhibition of the bone formation than seen with glucocorticoids alone, and the strength of the bone was the same after combined treatment [59]. However, the response to teriparatide was somewhat attenuated by glucocorticoids doses greater than 15 mg/day of prednisone equivalent. This partial inhibition of the response at higher doses of glucocorticoids was not seen for alendronate [60]. Human clinical trials have not only demonstrated teriparatide as efficacious for GIOP [39, 61,62,63,64,65], but that it was superior to alendronate in prevention of a small number of vertebral fracture at 24 and 36 months (0.6% vs 6.1% and 1.7% vs 7.7% respectively) [39, 64]. Teriparatide is used for 24 months of treatment in patients with GIOP. Providers should consider teriparatide in selected, high-risk patients (i.e., older adults starting higher dose steroids, multiple prior fractures, and very low initial bone mass), potentially even as an initial GIOP drug. However, due to teriparatide’s significantly higher cost than generic therapies and the inconvenience of a once-daily subcutaneous administration, its use in GIOP is limited.
Hormone replacement therapy (HRT), selective estrogen receptor modulators (SERMs), and testosterone
The efficacy of sex steroid as therapeutic agents in GIOP had been seen in small clinical trials without drug registration indications [66,67,68,69]. However, a large randomized controlled trial from the Women’s Health Initiative provided evidence of increased risk of coronary heart disease, stroke, pulmonary embolism, and breast cancer in older women treated with estrogens who were not on glucocorticoids [70]. Nevertheless, short-term HRT and SERMs may be considered, respectively, in symptomatic women with postmenopausal symptoms and young women with contraindications to more extensively tested GIOP therapies, who do not have contraindications to estrogen or estrogen-like moiety. This may be problematic in patients with connective tissue diseases taking glucocorticoids who, not uncommonly, are at higher risk of thromboembolic diatheses. Data from three clinical trials evaluating testosterone in GIOP patients demonstrated efficacy in increasing BMD, particularly of note was a moderate increase in lumbar spine BMD [71,72,73,74]. Similar to HRT and SERMs, testosterone should be considered in selected patients (i.e., men suffering from symptomatic hypogonadism) taking chronic glucocorticoids and may be contraindicated due to possibly short- and long-term safety concerns when other better-tested and more bone-specific therapies.
Cost-effectiveness of treatment and long-term compliance
GIOP treatment should take into account efficacy, safety, adherence, and at a societal level, cost-effectiveness. With the lengthening of life expectancy and the surprising growing worldwide usage of glucocorticoids, GIOP is both an economic and clinical problem. Despite the overwhelming clinical evidence available, only approximately 1 out of 5 US patients on glucocorticoids is taking an osteoporosis medication [75, 76]. Bisphosphonates are now all available as generic drugs and represent the least expensive medication option for GIOP. A Markov microsimulation model determined the cost-effectiveness of using bisphosphonates for patients with GIOP [77]. Assumptions included that the intervention had no incremental cost, and under these circumstances, the resultant incremental cost-effectiveness ratios (ICERs) were $188,000 per hip fracture averted and $273,000 per quality adjusted life years (QALY). The same analysis revealed that when a generic antiosteoporotic drug is used in a high-risk cohort of patient with optimal treatment adherence; the ICERs improved significantly to $84,000 per QALY and $57,900 per fracture averted [77]. In another analysis of the use of bisphosphonates in patients taking 5 mg of prednisone equivalent daily, the cost per one QALY gained with bisphosphonates varied from approximately $53,300 in women aged < 60 years, $22,100 in women aged 60–79 years, and $6500 in women aged ≥ 80 years. With 15 mg of prednisone equivalent, the same set of women varied from $22,100, $16,900, and $19,500 respectively [78]. Another analysis showed that the ICER of 5-year alendronate therapy ranged from $10,958 in the best-case scenario (45-year-old women with prevalent fracture treated with 10 mg/day of prednisone equivalent) to $66,791 in the worst-case scenario (65-year-old woman without previous fractures treated with 2.5 mg/day of prednisone equivalent) [79]. Teriparatide may be one of the most effective treatments for GIOP having shown superior fracture prevention to alendronate [39]; however, it is currently the most expensive drug available to treat GIOP. A computer simulation model among higher risk patients (women aged more than 69 years with T-score ≤ 2.5) showed that teriparatide is justifiable as first-line treatment at a cost per QALY (quality-adjusted life year) threshold of $50,000.
GIOP monitoring
Dual-energy X-ray absorptiometry, FRAX, and trabecular bone score
Algorithms had been developed to better quantify the fracture risk in GIOP patients most incorporating use of FRAX to help risk stratify [80, 81]; however, the FRAX algorithm instrument includes only a dichotomous variable for glucocorticoids, an assumption that does not consider treatment duration and dosage concurrently. FRAX can be adjusted to account for daily dosage but not for the cumulative dosage or length of use [82]. The FRAX and a number of other algorithms lack the ability to provide estimates for young patients, many of whom use glucocorticoids. The current American College of Rheumatology (ACR) guidelines on prevention and treatment of GIOP advise a baseline DXA evaluation to better discriminate the high-risk patients from lower-risk patients and where appropriate to consider serial DXA after treatment [83]. The trabecular bone score may preferentially capture differences between drugs in therapeutic response in women treated with glucocorticoids relative to routine DXA [61].
High-resolution peripheral computed tomography (HRpQCT) with finite element analysis
Comparing postmenopausal women treated with glucocorticoids and controls, women treated with glucocorticoids had lower cortical and trabecular volumetric BMD, with fewer trabecular plates, abnormality in the alignment of trabeculae, and less connectivity between trabeculae, all resulting in altered microarchitecture relative to controls [84]. Average volumetric BMD (vBMD) and cortical vBMD were significantly reduced in systemic lupus erythematosus patients treated with glucocorticoids. In these patients, the cortical microarchitecture was mainly affected with a 6.3% reduction in cortical thickness and higher cortical porosity [85]. HRpQCT using finite element analysis may also be useful in comparing therapeutic efficacy. For example, teriparatide appeared significantly more effective than risedronate in improving finite element analysis measures that assessed anterior bending, axial compression, and axial torsion [65].
Microindentation
A small pilot study of microindentation in GIOP patients showed that the bone material strength index, a qualitative measurement of bone strength, significantly decreased in patients using glucocorticoids in combination with calcium and vitamin D after 7 weeks of therapy, remained stable in patients using a glucocorticoid in combination with risedronate, and increased in patients taking a glucocorticoid in combination with denosumab or teriparatide [86].
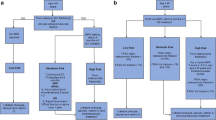
International guidelines on GIOP treatment
Numerous groups have developed societal and national guidelines for GIOP. Some differences and similarities exist between the more recent national and international guideline on the treatment of GIOP patients (Table 2). Most of the guidelines advocate that patients should receive at least 400 UI/day of cholecalciferol or equivalent and at least 1200 mg/day of elemental calcium intake [35,36,37]. The BMD threshold for pharmacological intervention in GIOP patients is generally a T-score between − 1.5 and − 1.0. Most guidelines recommend evaluating fracture risk with FRAX [87,88,89]. The ACR 2017 guidelines recommend pharmacologic intervention in patients with a 10-year risk of major osteoporotic fracture > 10% or with a history of previous osteoporotic fracture or with T-score less than − 2.5 or those treated with very high dose of glucocorticoids [83]. ACR guidelines recommend oral bisphosphonates as the first line of treatment in all GIOP patients not of childbearing potential [83]. Furthermore, 2017 ACR guidelines suggested zoledronic acid, teriparatide, denosumab, and raloxifene as the second, third, fourth, and fifth lines of treatment, respectively, for patients who do not tolerate oral bisphosphonates. This conditional recommendation about treatment order preference was determined based on efficacy, toxicity, and the cost of treatments. It is notable that this treatment order preference was formulated prior to the denosumab clinical trial in GIOP [56]. Other society guidelines do not incorporate the FRAX and set the threshold for intervention at ≥ 7.5 mg of prednisone equivalent [90, 91]. The UK National Osteoporosis Guideline Group (NOGG) on GIOP suggests antiosteoporotic therapies for women and men age ≥ 70 years, with a previous fragility fracture, or who are taking high doses of glucocorticoids (≥ 7.5 mg/day prednisone equivalent). They recommend that in all other individuals, the risk should be assessed with the 2011 updated FRAX. These strategies might underestimate the risk in patients chronically treated with a lower dosage of glucocorticoids. Another example of prevention and treatment strategy comes from 2016 Italian guidelines and reimbursability criteria for treatment of GIOP [92]. In this guideline, postmenopausal women and men > 50 years without history of fragility fracture, with an expected treatment of > 3 months, and with ≥ 5 mg/day of prednisone equivalent should be treated with oral or IV bisphosphonates as the first line and with denosumab as the second line of treatment. Within this same guideline, patients with a vertebral or hip fracture treated with ≥ 5 mg/day of prednisone equivalent should be treated with teriparatide as the first line of treatment.
Conclusions
GIOP is a well-recognized public health problem that causes disability and mortality. The key points to be aware in the treatment of GIOP are as follows: (1) GIOP is a problem not only in the elderly; (2) imminent fracture risk in GIOP rises quickly after the initiation of glucocorticoids but is also related to time and dosage of glucocorticoids (i.e., the higher the dosage and the longer the treatment, the greater the risk); (3) the pathogenesis of GIOP is complex, including reduced bone formation and increased bone resorption; (4) the assessment of fracture risk in GIOP patients can be difficult, but guidelines suggest tools to better estimate the risk and to guide the treatment selection; and (5) clinicians have GIOP medications in their armamentarium, all with demonstrated efficacy for improving bone mineral density and several with suggested efficacy in reducing fracture, in particular reducing vertebral fracture risk.
Learning objectives
-
1.
To understand pathogenesis, epidemiology, and clinical and societal burden of GIOP.
-
2.
To understand the risk of glucocorticoid depending on duration and dose of treatment.
-
3.
To acknowledge all the possible therapeutic options and international society guidelines differences.
References
Overman RA, Yeh J-Y, Deal CL (2013) Prevalence of oral glucocorticoid usage in the United States: a general population perspective. Arthritis Care Res (Hoboken) 65:294–298. https://doi.org/10.1002/acr.21796
Walsh LJ, Wong CA, Pringle M, Tattersfield AE (1996) Use of oral corticosteroids in the community and the prevention of secondary osteoporosis: a cross sectional study. BMJ 313:344–346. https://doi.org/10.1136/bmj.313.7053.344
Mudano A, Allison J, Hill J et al (2001) Variations in glucocorticoid induced osteoporosis prevention in a managed care cohort. J Rheumatol 28:1298–1305
Saag KG, Koehnke R, Caldwell JR, Brasington R, Burmeister LF, Zimmerman B, Kohler JA, Furst DE (1994) Low dose long-term corticosteroid therapy in rheumatoid arthritis: an analysis of serious adverse events. Am J Med 96:115–123. https://doi.org/10.1016/0002-9343(94)90131-7
Amiche MA, Albaum JM, Tadrous M, Pechlivanoglou P, Lévesque LE, Adachi JD, Cadarette SM (2016) Fracture risk in oral glucocorticoid users: a Bayesian meta-regression leveraging control arms of osteoporosis clinical trials. Osteoporos Int 27:1709–1718. https://doi.org/10.1007/s00198-015-3455-9
Roux C, Briot K (2017) Imminent fracture risk. Osteoporos Int 28:1765–1769. https://doi.org/10.1007/s00198-017-3976-5
Amiche MA, Abtahi S, Driessen JHM, Vestergaard P, de Vries F, Cadarette SM, Burden AM (2018) Impact of cumulative exposure to high-dose oral glucocorticoids on fracture risk in Denmark: a population-based case-control study. Arch Osteoporos 13:30. https://doi.org/10.1007/s11657-018-0424-x
Balasubramanian A, Wade SW, Adler RA, Lin CJF, Maricic M, O’Malley CD, Saag K, Curtis JR (2016) Glucocorticoid exposure and fracture risk in patients with new-onset rheumatoid arthritis. Osteoporos Int 27:3239–3249. https://doi.org/10.1007/s00198-016-3646-z
van Staa TP, Leufkens HG, Abenhaim L et al (2000) Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology (Oxford) 39:1383–1389. https://doi.org/10.1093/rheumatology/39.12.1383
Van Staa TP, Leufkens HG, Abenhaim L et al (2000) Use of oral corticosteroids and risk of fractures. J Bone Miner Res 15:993–1000. https://doi.org/10.1359/jbmr.2000.15.6.993
Paskins Z, Whittle R, Sultan AA, Muller S, Blagojevic-Bucknall M, Helliwell T, Hider S, Roddy E, Mallen C (2018) Risk of fracture among patients with polymyalgia rheumatica and giant cell arteritis: a population-based study. BMC Med 16:4. https://doi.org/10.1186/s12916-017-0987-1
Bultink IEM, Harvey NC, Lalmohamed A, Cooper C, Lems WF, van Staa TP, de Vries F (2014) Elevated risk of clinical fractures and associated risk factors in patients with systemic lupus erythematosus versus matched controls: a population-based study in the United Kingdom. Osteoporos Int 25:1275–1283. https://doi.org/10.1007/s00198-013-2587-z
Ramsey-Goldman R, Dunn JE, Huang CF, Dunlop D, Rairie JE, Fitzgerald S, Manzi S (1999) Frequency of fractures in women with systemic lupus erythematosus: comparison with United States population data. Arthritis Rheum 42:882–890. https://doi.org/10.1002/1529-0131(199905)42:5<882::AID-ANR6>3.0.CO;2-C
Casagrande SS, Cowie CC, Malozowski S (2017) Glucocorticoid use and its association with skeletal health among U.S. adults with diabetes. J Diabetes Complicat 31:353–357. https://doi.org/10.1016/j.jdiacomp.2016.06.021
Graat-Verboom L, van den Borne BEEM, Smeenk FWJM, Spruit MA, Wouters EFM (2011) Osteoporosis in COPD outpatients based on bone mineral density and vertebral fractures. J Bone Miner Res 26:561–568. https://doi.org/10.1002/jbmr.257
Lu P-C, Yang Y-H, Guo S-E, Yang T-M (2017) Factors associated with osteoporosis in patients with chronic obstructive pulmonary disease-a nationwide retrospective study. Osteoporos Int 28:359–367. https://doi.org/10.1007/s00198-016-3732-2
Okazaki R, Watanabe R, Inoue D (2016) Osteoporosis associated with chronic obstructive pulmonary disease. J Bone Metab 23:111–120. https://doi.org/10.11005/jbm.2016.23.3.111
Jones A, Fay JK, Burr ML, Stone M, Hood K, Roberts G, Cochrane Airways Group (2002) Inhaled corticosteroid effects on bone metabolism in asthma and mild chronic obstructive pulmonary disease. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003537
Suissa S, Baltzan M, Kremer R, Ernst P (2004) Inhaled and nasal corticosteroid use and the risk of fracture. Am J Respir Crit Care Med 169:83–88. https://doi.org/10.1164/rccm.200305-640OC
Hubbard R, Tattersfield A, Smith C, West J, Smeeth L, Fletcher A (2006) Use of inhaled corticosteroids and the risk of fracture. Chest 130:1082–1088. https://doi.org/10.1378/chest.130.4.1082
Diederich S, Eigendorff E, Burkhardt P, Quinkler M, Bumke-Vogt C, Rochel M, Seidelmann D, Esperling P, Oelkers W, Bähr V (2002) 11beta-hydroxysteroid dehydrogenase types 1 and 2: an important pharmacokinetic determinant for the activity of synthetic mineralo- and glucocorticoids. J Clin Endocrinol Metab 87:5695–5701. https://doi.org/10.1210/jc.2002-020970
Wu Z, Bucher NL, Farmer SR (1996) Induction of peroxisome proliferator-activated receptor gamma during the conversion of 3T3 fibroblasts into adipocytes is mediated by C/EBPbeta, C/EBPdelta, and glucocorticoids. Mol Cell Biol 16:4128–4136. https://doi.org/10.1128/MCB.16.8.4128
Ohnaka K, Tanabe M, Kawate H, Nawata H, Takayanagi R (2005) Glucocorticoid suppresses the canonical Wnt signal in cultured human osteoblasts. Biochem Biophys Res Commun 329:177–181. https://doi.org/10.1016/j.bbrc.2005.01.117
Hayashi K, Yamaguchi T, Yano S, Kanazawa I, Yamauchi M, Yamamoto M, Sugimoto T (2009) BMP/Wnt antagonists are upregulated by dexamethasone in osteoblasts and reversed by alendronate and PTH: potential therapeutic targets for glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun 379:261–266. https://doi.org/10.1016/j.bbrc.2008.12.035
Almeida M, Han L, Ambrogini E, Weinstein RS, Manolagas SC (2011) Glucocorticoids and tumor necrosis factor α increase oxidative stress and suppress Wnt protein signaling in osteoblasts. J Biol Chem 286:44326–44335. https://doi.org/10.1074/jbc.M111.283481
Mazziotti G, Formenti AM, Adler RA, Bilezikian JP, Grossman A, Sbardella E, Minisola S, Giustina A (2016) Glucocorticoid-induced osteoporosis: pathophysiological role of GH/IGF-I and PTH/VITAMIN D axes, treatment options and guidelines. Endocrine 54:603–611. https://doi.org/10.1007/s12020-016-1146-8
Ritchlin CT, Haas-Smith SA, Li P, Hicks DG, Schwarz EM (2003) Mechanisms of TNF-α– and RANKL-mediated osteoclastogenesis and bone resorption in psoriatic arthritis. J Clin Investig 111:821–831. https://doi.org/10.1172/JCI16069
Dovio A, Perazzolo L, Saba L, Termine A, Capobianco M, Bertolotto A, Angeli A (2006) High-dose glucocorticoids increase serum levels of soluble IL-6 receptor alpha and its ratio to soluble gp130: an additional mechanism for early increased bone resorption. Eur J Endocrinol 154:745–751. https://doi.org/10.1530/eje.1.02147
Takuma A, Kaneda T, Sato T, Ninomiya S, Kumegawa M, Hakeda Y (2003) Dexamethasone enhances osteoclast formation synergistically with transforming growth factor-beta by stimulating the priming of osteoclast progenitors for differentiation into osteoclasts. J Biol Chem 278:44667–44674. https://doi.org/10.1074/jbc.M300213200
Weinstein RS, Wan C, Liu Q, Wang Y, Almeida M, O’Brien CA, Thostenson J, Roberson PK, Boskey AL, Clemens TL, Manolagas SC (2010) Endogenous glucocorticoids decrease skeletal angiogenesis, vascularity, hydration, and strength in aged mice. Aging Cell 9:147–161. https://doi.org/10.1111/j.1474-9726.2009.00545.x
Chappard D, Legrand E, Basle MF et al (1996) Altered trabecular architecture induced by corticosteroids: a bone histomorphometric study. J Bone Miner Res 11:676–685. https://doi.org/10.1002/jbmr.5650110516
Dalle Carbonare L, Arlot ME, Chavassieux PM et al (2001) Comparison of trabecular bone microarchitecture and remodeling in glucocorticoid-induced and postmenopausal osteoporosis. J Bone Miner Res 16:97–103. https://doi.org/10.1359/jbmr.2001.16.1.97
Van Staa TP, Laan RF, Barton IP et al (2003) Bone density threshold and other predictors of vertebral fracture in patients receiving oral glucocorticoid therapy. Arthritis Rheum 48:3224–3229. https://doi.org/10.1002/art.11283
Sato AY, Richardson D, Cregor M, Davis HM, Au ED, McAndrews K, Zimmers TA, Organ JM, Peacock M, Plotkin LI, Bellido T (2017) Glucocorticoids induce bone and muscle atrophy by tissue-specific mechanisms upstream of E3 ubiquitin ligases. Endocrinology 158:664–677. https://doi.org/10.1210/en.2016-1779
Pearce G, Tabensky DA, Delmas PD, Baker HWG, Seeman E (1998) Corticosteroid-induced bone loss in men. J Clin Endocrinol Metab 83:801–806. https://doi.org/10.1210/jcem.83.3.4621
Richy F, Ethgen O, Bruyere O, Reginster J-Y (2004) Efficacy of alphacalcidol and calcitriol in primary and corticosteroid-induced osteoporosis: a meta-analysis of their effects on bone mineral density and fracture rate. Osteoporos Int 15:301–310. https://doi.org/10.1007/s00198-003-1570-5
de Nijs RNJ, Jacobs JWG, Algra A, Lems WF, Bijlsma JWJ (2004) Prevention and treatment of glucocorticoid-induced osteoporosis with active vitamin D3 analogues: a review with meta-analysis of randomized controlled trials including organ transplantation studies. Osteoporos Int 15:589–602. https://doi.org/10.1007/s00198-004-1614-5
Saag KG, Emkey R, Schnitzer TJ, Brown JP, Hawkins F, Goemaere S, Thamsborg G, Liberman UA, Delmas PD, Malice MP, Czachur M, Daifotis AG, Lane N, Correa-Rotter R, Yanover M, Westhovens R, Epstein S, Adachi JD, Poubelle P, Melo-Gomes J, Rodriguez-Portales JA (1998) Alendronate for the prevention and treatment of glucocorticoid-induced osteoporosis. Glucocorticoid-induced osteoporosis intervention study group. N Engl J Med 339:292–299. https://doi.org/10.1056/NEJM199807303390502
Saag KG, Shane E, Boonen S, Marín F, Donley DW, Taylor KA, Dalsky GP, Marcus R (2007) Teriparatide or alendronate in glucocorticoid-induced osteoporosis. N Engl J Med 357:2028–2039. https://doi.org/10.1056/NEJMoa071408
Reid DM, Hughes RA, Laan RF, Sacco-Gibson NA, Wenderoth DH, Adami S, Eusebio RA, Devogelaer JP (2000) Efficacy and safety of daily risedronate in the treatment of corticosteroid-induced osteoporosis in men and women: a randomized trial. European Corticosteroid-Induced Osteoporosis Treatment Study. J Bone Miner Res 15:1006–1013. https://doi.org/10.1359/jbmr.2000.15.6.1006
Cohen S, Levy RM, Keller M, Boling E, Emkey RD, Greenwald M, Zizic TM, Wallach S, Sewell KL, Lukert BP, Axelrod DW, Chines AA (1999) Risedronate therapy prevents corticosteroid-induced bone loss: a twelve-month, multicenter, randomized, double-blind, placebo-controlled, parallel-group study. Arthritis Rheum 42:2309–2318. https://doi.org/10.1002/1529-0131(199911)42:11<2309::AID-ANR8>3.0.CO;2-K
Adachi JD, Saag KG, Delmas PD, Liberman UA, Emkey RD, Seeman E, Lane NE, Kaufman JM, Poubelle PEE, Hawkins F, Correa-Rotter R, Menkes CJ, Rodriguez-Portales JA, Schnitzer TJ, Block JA, Wing J, McIlwain HH, Westhovens R, Brown J, Melo-Gomes JA, Gruber BL, Yanover MJ, Leite MOR, Siminoski KG, Nevitt MC, Sharp JT, Malice MP, Dumortier T, Czachur M, Carofano W, Daifotis A (2001) Two-year effects of alendronate on bone mineral density and vertebral fracture in patients receiving glucocorticoids: a randomized, double-blind, placebo-controlled extension trial. Arthritis Rheum 44:202–211. https://doi.org/10.1002/1529-0131(200101)44:1<202::AID-ANR27>3.0.CO;2-W
Stoch SA, Saag KG, Greenwald M et al (2009) Once-weekly oral alendronate 70 mg in patients with glucocorticoid-induced bone loss: a 12-month randomized, placebo-controlled clinical trial. J Rheumatol 36:1705–1714. https://doi.org/10.3899/jrheum.081207
Reid DM, Adami S, Devogelaer JP, Chines AA (2001) Risedronate increases bone density and reduces vertebral fracture risk within one year in men on corticosteroid therapy. Calcif Tissue Int 69:242–247. https://doi.org/10.1007/s00223-001-1060-8
Wallach S, Cohen S, Reid DM, Hughes RA, Hosking DJ, Laan RF, Doherty SM, Maricic M, Rosen C, Brown J, Barton I, Chines AA (2000) Effects of risedronate treatment on bone density and vertebral fracture in patients on corticosteroid therapy. Calcif Tissue Int 67:277–285. https://doi.org/10.1007/s002230001146
Ringe JD, Dorst A, Faber H, Ibach K, Sorenson F (2003) Intermittent intravenous ibandronate injections reduce vertebral fracture risk in corticosteroid-induced osteoporosis: results from a long-term comparative study. Osteoporos Int 14:801–807. https://doi.org/10.1007/s00198-003-1425-0
Shin K, Park S-H, Park W et al (2017) Monthly oral ibandronate reduces bone loss in Korean women with rheumatoid arthritis and osteopenia receiving long-term glucocorticoids: a 48-week double-blinded randomized placebo-controlled investigator-initiated trial. Clin Ther 39:268–278.e2. https://doi.org/10.1016/j.clinthera.2017.01.008
Fahrleitner-Pammer A, Piswanger-Soelkner JC, Pieber TR, Obermayer-Pietsch BM, Pilz S, Dimai HP, Prenner G, Tscheliessnigg KH, Hauge E, Portugaller RH, Dobnig H (2009) Ibandronate prevents bone loss and reduces vertebral fracture risk in male cardiac transplant patients: a randomized double-blind, placebo-controlled trial. J Bone Miner Res 24:1335–1344. https://doi.org/10.1359/jbmr.090216
Reid DM, Devogelaer J-P, Saag K, Roux C, Lau CS, Reginster JY, Papanastasiou P, Ferreira A, Hartl F, Fashola T, Mesenbrink P, Sambrook PN (2009) Zoledronic acid and risedronate in the prevention and treatment of glucocorticoid-induced osteoporosis (HORIZON): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 373:1253–1263. https://doi.org/10.1016/S0140-6736(09)60250-6
Axelsson KF, Nilsson AG, Wedel H, Lundh D, Lorentzon M (2017) Association between alendronate use and hip fracture risk in older patients using oral prednisolone. JAMA 318:146–155. https://doi.org/10.1001/jama.2017.8040
Allen CS, Yeung JH, Vandermeer B, Homik J (2016) Bisphosphonates for steroid-induced osteoporosis. Cochrane Database Syst Rev 10:CD001347. https://doi.org/10.1002/14651858.CD001347.pub2
Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O'Ryan F, Reid IR, Ruggiero SL, Taguchi A, Tetradis S, Watts NB, Brandi ML, Peters E, Guise T, Eastell R, Cheung AM, Morin SN, Masri B, Cooper C, Morgan SL, Obermayer-Pietsch B, Langdahl BL, al Dabagh R, Davison KS, Kendler DL, Sándor GK, Josse RG, Bhandari M, el Rabbany M, Pierroz DD, Sulimani R, Saunders DP, Brown JP, Compston J, on behalf of the International Task Force on Osteonecrosis of the Jaw (2015) Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res 30:3–23. https://doi.org/10.1002/jbmr.2405
Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O'Keefe R, Papapoulos S, Howe TS, van der Meulen MCH, Weinstein RS, Whyte MP (2014) Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 29:1–23. https://doi.org/10.1002/jbmr.1998
Koh JH, Myong JP, Yoo J, Lim YW, Lee J, Kwok SK, Park SH, Ju JH (2017) Predisposing factors associated with atypical femur fracture among postmenopausal Korean women receiving bisphosphonate therapy: 8 years’ experience in a single center. Osteoporos Int 28:3251–3259. https://doi.org/10.1007/s00198-017-4169-y
Horton DB, Haynes K, Denburg MR, Thacker MM, Rose CD, Putt ME, Leonard MB, Strom BL (2017) Oral glucocorticoid use and osteonecrosis in children and adults with chronic inflammatory diseases: a population-based cohort study. BMJ Open 7:e016788. https://doi.org/10.1136/bmjopen-2017-016788
Saag KG, Wagman RB, Geusens P, Adachi JD, Messina OD, Emkey R, Chapurlat R, Wang A, Pannacciulli N, Lems WF (2018) Denosumab versus risedronate in glucocorticoid-induced osteoporosis: a multicentre, randomised, double-blind, active-controlled, double-dummy, non-inferiority study. Lancet Diabetes Endocrinol 6:445–454. https://doi.org/10.1016/S2213-8587(18)30075-5
Anastasilakis AD, Polyzos SA, Makras P, Aubry-Rozier B, Kaouri S, Lamy O (2017) Clinical features of 24 patients with rebound-associated vertebral fractures after denosumab discontinuation: systematic review and additional cases. J Bone Miner Res 32:1291–1296. https://doi.org/10.1002/jbmr.3110
Tsourdi E, Langdahl B, Cohen-Solal M, Aubry-Rozier B, Eriksen EF, Guañabens N, Obermayer-Pietsch B, Ralston SH, Eastell R, Zillikens MC (2017) Discontinuation of denosumab therapy for osteoporosis: a systematic review and position statement by ECTS. Bone 105:11–17. https://doi.org/10.1016/j.bone.2017.08.003
Oxlund H, Ortoft G, Thomsen JS et al (2006) The anabolic effect of PTH on bone is attenuated by simultaneous glucocorticoid treatment. Bone 39:244–252. https://doi.org/10.1016/j.bone.2006.01.142
Devogelaer J-P, Adler RA, Recknor C et al (2010) Baseline glucocorticoid dose and bone mineral density response with teriparatide or alendronate therapy in patients with glucocorticoid-induced osteoporosis. J Rheumatol 37:141–148. https://doi.org/10.3899/jrheum.090411
Saag KG, Agnusdei D, Hans D et al (2016) Trabecular bone score in patients with chronic glucocorticoid therapy-induced osteoporosis treated with alendronate or teriparatide. Arthritis Rheumatol 68:2122–2128. https://doi.org/10.1002/art.39726
Langdahl BL, Marin F, Shane E, Dobnig H, Zanchetta JR, Maricic M, Krohn K, See K, Warner MR (2009) Teriparatide versus alendronate for treating glucocorticoid-induced osteoporosis: an analysis by gender and menopausal status. Osteoporos Int 20:2095–2104. https://doi.org/10.1007/s00198-009-0917-y
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mellström D, Oefjord ES, Marcinowska-Suchowierska E, Salmi J, Mulder H, Halse J, Sawicki AZ, Mitlak BH (2001) Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441. https://doi.org/10.1056/NEJM200105103441904
Saag KG, Zanchetta JR, Devogelaer J-P, Adler RA, Eastell R, See K, Krege JH, Krohn K, Warner MR (2009) Effects of teriparatide versus alendronate for treating glucocorticoid-induced osteoporosis: thirty-six-month results of a randomized, double-blind, controlled trial. Arthritis Rheum 60:3346–3355. https://doi.org/10.1002/art.24879
Glüer C-C, Marin F, Ringe JD, Hawkins F, Möricke R, Papaioannu N, Farahmand P, Minisola S, Martínez G, Nolla JM, Niedhart C, Guañabens N, Nuti R, Martín-Mola E, Thomasius F, Kapetanos G, Peña J, Graeff C, Petto H, Sanz B, Reisinger A, Zysset PK (2013) Comparative effects of teriparatide and risedronate in glucocorticoid-induced osteoporosis in men: 18-month results of the EuroGIOPs trial. J Bone Miner Res 28:1355–1368. https://doi.org/10.1002/jbmr.1870
Mok CC, Ying KY, To CH et al (2011) Raloxifene for prevention of glucocorticoid-induced bone loss: a 12-month randomised double-blinded placebo-controlled trial. Ann Rheum Dis 70:778–784. https://doi.org/10.1136/ard.2010.143453
Kung AW, Chan TM, Lau CS et al (1999) Osteopenia in young hypogonadal women with systemic lupus erythematosus receiving chronic steroid therapy: a randomized controlled trial comparing calcitriol and hormonal replacement therapy. Rheumatology (Oxford) 38:1239–1244. https://doi.org/10.1093/rheumatology/38.12.1239
Hall GM, Daniels M, Doyle DV, Spector TD (1994) Effect of hormone replacement therapy on bone mass in rheumatoid arthritis patients treated with and without steroids. Arthritis Rheum 37:1499–1505. https://doi.org/10.1002/art.1780371014
Lane NE, Sanchez S, Modin GW, Genant HK, Pierini E, Arnaud CD (1998) Parathyroid hormone treatment can reverse corticosteroid-induced osteoporosis. Results of a randomized controlled clinical. trial J Clin Invest 102:1627–1633. https://doi.org/10.1172/JCI3914
Rossouw JE, Anderson GL, Prentice RL et al (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 288:321–333. https://doi.org/10.1001/jama.288.3.321
Hall GM, Larbre JP, Spector TD et al (1996) A randomized trial of testosterone therapy in males with rheumatoid arthritis. Br J Rheumatol 35:568–573. https://doi.org/10.1093/rheumatology/35.6.568
Reid IR, Wattie DJ, Evans MC, Stapleton JP (1996) Testosterone therapy in glucocorticoid-treated men. Arch Intern Med 156:1173–1177. https://doi.org/10.1001/archinte.156.11.1173
Crawford BAL, Liu PY, Kean MT, Bleasel JF, Handelsman DJ (2003) Randomized placebo-controlled trial of androgen effects on muscle and bone in men requiring long-term systemic glucocorticoid treatment. J Clin Endocrinol Metab 88:3167–3176. https://doi.org/10.1210/jc.2002-021827
Snyder PJ, Peachey H, Berlin JA, Hannoush P, Haddad G, Dlewati A, Santanna J, Loh L, Lenrow DA, Holmes JH, Kapoor SC, Atkinson LE, Strom BL (2000) Effects of testosterone replacement in hypogonadal men. J Clin Endocrinol Metab 85:2670–2677. https://doi.org/10.1210/jcem.85.8.6731
Albaum JM, Lévesque LE, Gershon AS, Liu G, Cadarette SM (2015) Glucocorticoid-induced osteoporosis management among seniors, by year, sex, and indication, 1996-2012. Osteoporos Int 26:2845–2852. https://doi.org/10.1007/s00198-015-3200-4
McKeown E, Bykerk VP, De Leon F et al (2012) Quality assurance study of the use of preventative therapies in glucocorticoid-induced osteoporosis in early inflammatory arthritis: results from the CATCH cohort. Rheumatology (Oxford) 51:1662–1669. https://doi.org/10.1093/rheumatology/kes079
Beukelman T, Saag KG, Curtis JR, Kilgore ML, Pisu M (2010) Cost-effectiveness of multifaceted evidence implementation programs for the prevention of glucocorticoid-induced osteoporosis. Osteoporos Int 21:1573–1584. https://doi.org/10.1007/s00198-009-1114-8
van Staa TP, Geusens P, Zhang B, Leufkens HGM, Boonen A, Cooper C (2007) Individual fracture risk and the cost-effectiveness of bisphosphonates in patients using oral glucocorticoids. Rheumatology (Oxford) 46:460–466. https://doi.org/10.1093/rheumatology/kel249
Moriwaki K, Fukuda H (2019) Cost-effectiveness of implementing guidelines for the treatment of glucocorticoid-induced osteoporosis in Japan. Osteoporos Int. https://doi.org/10.1007/s00198-018-4798-9
Adami S, Bianchi G, Brandi ML et al (2010) Validation and further development of the WHO 10-year fracture risk assessment tool in Italian postmenopausal women: project rationale and description. Clin Exp Rheumatol 28:561–570
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397. https://doi.org/10.1007/s00198-007-0543-5
Kanis JA, Johansson H, Oden A, McCloskey EV (2011) Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int 22:809–816. https://doi.org/10.1007/s00198-010-1524-7
Buckley L, Guyatt G, Fink HA et al (2017) 2017 American College of Rheumatology guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Rheumat 69:1521–1537. https://doi.org/10.1002/art.40137
Sutter S, Nishiyama KK, Kepley A, Zhou B, Wang J, McMahon DJ, Guo XE, Stein EM (2014) Abnormalities in cortical bone, trabecular plates, and stiffness in postmenopausal women treated with glucocorticoids. J Clin Endocrinol Metab 99:4231–4240. https://doi.org/10.1210/jc.2014-2177
Tang XL, Qin L, Kwok AW, Zhu TY, Kun EW, Hung VW, Griffith JF, Leung PC, Li EK, Tam LS (2013) Alterations of bone geometry, density, microarchitecture, and biomechanical properties in systemic lupus erythematosus on long-term glucocorticoid: a case-control study using HR-pQCT. Osteoporos Int 24:1817–1826. https://doi.org/10.1007/s00198-012-2177-5
Mellibovsky L, Prieto-Alhambra D, Mellibovsky F, Güerri-Fernández R, Nogués X, Randall C, Hansma PK, Díez-Perez A (2015) Bone tissue properties measurement by reference point indentation in glucocorticoid-induced osteoporosis. J Bone Miner Res 30:1651–1656. https://doi.org/10.1002/jbmr.2497
Compston J, Cooper A, Cooper C et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12:43. https://doi.org/10.1007/s11657-017-0324-5
Geusens PP, de Nijs RNJ, Lems WF et al (2004) Prevention of glucocorticoid osteoporosis: a consensus document of the Dutch Society for Rheumatology. Ann Rheum Dis 63:324–325. https://doi.org/10.1136/ard.2003.008060
Briot K, Cortet B, Roux C, Fardet L, Abitbol V, Bacchetta J, Buchon D, Debiais F, Guggenbuhl P, Laroche M, Legrand E, Lespessailles E, Marcelli C, Weryha G, Thomas T, Bone Section of the French Society for Rheumatology (SFR) and Osteoporosis Research and Information Group (GRIO) (2014) 2014 update of recommendations on the prevention and treatment of glucocorticoid-induced osteoporosis. Joint Bone Spine 81:493–501. https://doi.org/10.1016/j.jbspin.2014.10.001
Devogelaer J-P, Goemaere S, Boonen S, Body JJ, Kaufman JM, Reginster JY, Rozenberg S, Boutsen Y (2006) Evidence-based guidelines for the prevention and treatment of glucocorticoid-induced osteoporosis: a consensus document of the Belgian Bone Club. Osteoporos Int 17:8–19. https://doi.org/10.1007/s00198-005-2032-z
Suzuki Y, Nawata H, Soen S, Fujiwara S, Nakayama H, Tanaka I, Ozono K, Sagawa A, Takayanagi R, Tanaka H, Miki T, Masunari N, Tanaka Y (2014) Guidelines on the management and treatment of glucocorticoid-induced osteoporosis of the Japanese Society for Bone and Mineral Research: 2014 update. J Bone Miner Metab 32:337–350. https://doi.org/10.1007/s00774-014-0586-6
Rossini M, Adami S, Bertoldo F, Diacinti D, Gatti D, Giannini S, Giusti A, Malavolta N, Minisola S, Osella G, Pedrazzoni M, Sinigaglia L, Viapiana O, Isaia GC (2016) Guidelines for the diagnosis, prevention and management of osteoporosis. Reumatismo 68:1–39. https://doi.org/10.4081/reumatismo.2016.870
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Giovanni Adami declares that he has no conflict of interest. Kenneth G Saag declares research grant from Amgen and Merck and consultant fee from Amgen, Lilly, Merck, and Radius.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adami, G., Saag, K. Glucocorticoid-induced osteoporosis: 2019 concise clinical review. Osteoporos Int 30, 1145–1156 (2019). https://doi.org/10.1007/s00198-019-04906-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04906-x