Abstract
Summary
This study examined trends in osteoporosis and low bone mass in older US adults between 2005 and 2014 using bone mineral density (BMD) data from the National Health and Nutrition Examination Survey (NHANES). Osteoporosis and low bone mass appear to have increased at the femur neck but not at the lumbar spine during this period.
Introduction
Recent preliminary data from Medicare suggest that the decline in hip fracture incidence among older US adults may have plateaued in 2013–2014, but comparable data on BMD trends for this time period are currently lacking. This study examined trends in the prevalence of osteoporosis and low bone mass since 2005 using BMD data from NHANES. The present study also updated prevalence estimates to 2013–2014 and included estimates for non-Hispanic Asians.
Methods
Femur neck and lumbar spine BMD by DXA were available for 7954 adults aged 50 years and older from four NHANES survey cycles between 2005–2006 and 2013–2014.
Results
Significant trends (quadratic or linear) were observed for the femur neck (mean T-score and osteoporosis in both sexes; low bone mass in women) but not for the lumbar spine. The trend in femur neck status was somewhat U-shaped, with prevalences being most consistently significantly higher (by 1.1–6.6 percentage points) in 2013–2014 than 2007–2008. Adjusting for changes in body mass index, smoking, milk intake, and physician’s diagnosis of osteoporosis between surveys did not change femur neck trends. In 2013–2014, the percent of older adults with osteoporosis was 6% at the femur neck, 8% at the lumbar spine, and 11% at either site.
Conclusions
There was some evidence of a decline in femur neck BMD between 2005–2006 and 2013–2014, but not in lumbar spine BMD. Changes in the risk factors that could be examined did not explain the femur neck BMD trends.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
National data on bone density and hip fracture incidence showed improvements among older adults in the US between the mid-1980s and the end of the past decade. For example, data from the National Health and Nutrition Examination Survey (NHANES) showed a decline in the prevalence of femoral neck osteoporosis between 1988–1994 and 2005–2006 [1], and data from Medicare indicated a decline in hip fracture incidence between 1985 and 2012, at least in some race/ethnic groups [2, 3].
However, a more recent, preliminary analysis of Medicare data suggests that, as of 2013–2014, the decline in hip fracture incidence may have ended [4]. Whether similar changes in bone density have occurred during this same time period is not known. To address this question, the present study uses bone mineral density (BMD) of the proximal femur and lumbar spine of adults aged 50 years and older from four NHANES survey cycles (2005–2006, 2007–2008, 2009–2010, and 2013–2014) to examine trends in osteoporosis and low bone mass between through 2014.
The present study also updates and expands previously published estimates of osteoporosis and low bone mass for older US adults from NHANES [5, 6] in several ways. For example, it provides the first nationally representative estimates of osteoporosis and low bone mass among non-Hispanic Asians, which only became possible after 2010 because NHANES began oversampling this race/ethnic group in 2011 [7]. It also updates estimates to reflect status as of 2013–2014 (previous estimates reflected status either at the midpoint [5] or at the end [6] of the past decade), and provides estimates for the femur neck and lumbar spine separately, as well as in combination.
Methods
Sample
The present study used data collected in the NHANES, which is conducted by the National Center for Health Statistics (NCHS) to assess the health and nutritional status of a representative sample of the non-institutionalized, civilian US population. A complex, multistage probability sample design was used to select the sample [7, 8]. The present study examines data from four NHANES survey cycles covering the periods 2005–2010 and 2013–2014 because these are the survey cycles completed to date in which BMD of the proximal femur and lumbar spine have been measured with fan-beam DXA.Footnote 1 NHANES collects data via household interviews and direct standardized physical examinations conducted in specially equipped mobile examination centers [8]. All procedures in the NHANES survey cycles used in this study were approved by the NCHS Research Ethics Review Board, and written informed consent was obtained from all subjects. The overall unweighted examination response rate for adults aged 50 years and older in the four NHANES survey cycles were 67.1% in 2005–2006 and 2007–2008, 67.2% in 2009–2010, and 59.8% in 2013–2014.
Estimates from NHANES 2013–2014 by race and Hispanic origin are presented separately for non-Hispanic whites, non-Hispanic blacks, Hispanics (including Mexican Americans), and non-Hispanic Asians because NHANES 2013–2014 provides reliable estimates for these groups. Race and ethnicity were self-reported by the participants.
The analytic sample was derived from the 10,695 adults aged 50 years and older in NHANES 2005–2010 and 2013–2014 who received physical examinations. Of these, 2741 (23.5%) were excluded because they lacked valid BMD data for the proximal femur or did not have data for at least two lumbar vertebrae, as recommended by the International Society for Clinical Densitometry (ISCD) for calculation of lumbar spine T-scores [9]. The proportion of the total number of excluded respondents contributed by each survey cycle did not differ (p = 0.10), being approximately 21–22% in NHANES 2005–2006 and 2007–2008, and 25% in NHANES 2009–2010 and NHANES 2013–2014. In all survey periods, excluded respondents were more likely to be female, older, non-Hispanic black, and shorter and self-reported their health status as fair or poor than respondents in the analytic sample. The final main analytic sample consisted of 7954 respondents. Sample sizes for the individual survey cycles are shown in Fig. 1.
Bone density
Proximal femur and posterior-anterior lumbar spine scans were obtained with Hologic QDR 4500A fan-beam densitometers in NHANES 2005–2010 and with Hologic Discovery® A densitometers in NHANES 2013–2014 (Hologic Inc., Marlborough, MA). Details of the dual-energy x-ray absorptiometry (DXA) examination protocol have been published elsewhere [10]. Scanning was done in the fast array mode. Rigorous quality control (QC) programs were employed to monitor DXA scanners. All QC and respondent scans were analyzed at a central site (Department of Radiology of the University of California, San Francisco) using standard radiologic techniques and study-specific protocols developed for the NHANES [10]. All respondent scans were also reviewed by an expert at the central site. Survey respondents were not eligible for DXA scans if they were pregnant, self-reported an imaging procedure using contrast material in the previous 7 days, or weighed more than the DXA table weight limit (>300 lb in 2005–2010, >450 lb in 2013–2014).
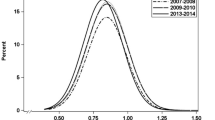
Spine scans obtained in NHANES 2005–2010 were analyzed using Apex version 3.0 software, while femur scans were analyzed using Discovery 12.4 software. APEX™ version 4.0 was used to analyze femur and spine scans in NHANES 2013–2014. Differences in DXA scan results for the same individuals have been noted previously when different DXA scan analysis software versions were used [11], so a study using a subsample of 600 adults from NHANES 2005–2010 was performed to compare femur results analyzed by the two software versions; study details and results are described in Supplementary Appendix 1. Results showed differences in mean BMD at four of the five regions of interest (ROI) (Supplementary Table 1). The exception occurred at the femur neck. However, software version had little effect on prevalence of low values at the four femur ROI that were examined (Supplementary Table 2), likely due to the fact that software differences were either small overall or were minimal in the lower end of the BMD distributions (Supplementary Figs. 1, 2, 3).
Skeletal status of adults aged 50 years and older was categorized using criteria recommended by the World Health Organization (WHO) [12]. T-scores were calculated as (BMDrespondent − mean BMDreference group)/standard deviationreference group. Low bone mass was defined as a T-score between −1.0 and −2.5, while osteoporosis was defined as a T-score ≤ −2.5. As recommended by the ISCD, the reference group for calculation of T-scores at the lumbar spine consisted of 30-year-old white females from the DXA manufacturer reference database, while the reference group for calculation of these scores for the femur neck consisted of 20–29 year-old non-Hispanic white females from NHANES III [13]. Prevalence of osteoporosis and low bone mass were calculated for the femur neck only, lumbar spine only, and for either the femur neck or the lumbar spine. The total femur ROI is also used clinically to define osteoporosis [9], but it was not included in the present study because previous analyses revealed that prevalence estimates based on either femur neck, lumbar spine, or total femur differed by less than 1 percentage point from those based on either femur neck or lumbar spine only [6].
Other variables
Trends in osteoporosis or low bone mass by survey period were assessed before and after controlling for changes in selected bone-related variables that might have contributed to changes in bone density over time. The following bone-related variables were selected on the basis of being available for all four survey cycles at the time of the study, and also being measured in a comparable manner in all periods:
Body mass index
Body mass index (BMI) is calculated as body weight (kilograms) divided by height (meters squared). Body weight was measured using an electronic load cell scale, and standing height was measured with a fixed stadiometer.
Cigarette smoking
Smokers were defined as respondents who self-reported that they currently or formerly smoked.
Milk use
Milk users were defined as respondents who reported drinking milk alone or on cereal one or more times per week during the past 30 days.
Osteoporosis diagnosis
Respondents who self-reported that their doctor had told them they had osteoporosis were defined as having an osteoporosis diagnosis.
Statistical analyses
Analyses were conducted with PC-SAS (Version 9.3, SAS Institute, Cary NC) and SUDAAN (Version 11.0.1, Research Triangle Institute, NC). All analyses used the examination sample weights and accounted for the complex survey design when calculating statistical tests. Prevalence estimates for NHANES 2013–2014 by race/Hispanic origin were age-adjusted to the 2000 Census using the direct method and the following age groups: 50–59, 60–69, 70–79, and 80+ years. The 2000 Census is currently the standard population recommended by the Department of Health and Human Services to use when calculating age-adjusted results [14, 15]. Tests of statistical significance were performed using t tests or chi-square analyses (for unadjusted results) and linear or logistic regression (for multivariate adjusted results). Linear and quadratic trends across survey periods by sex were tested by including single degree-of-freedom contrast terms in logistic regression models in which survey period was treated as a categorical variable. When quadratic or linear trends were statistically significant, pairwise comparison of means and prevalence estimates between individual survey periods were performed because there were too few survey cycles to permit use of joinpoint regression models to assess the shape of the trend.
Sensitivity analyses
A sensitivity analysis was performed to assess the impact of the addition of the non-Hispanic Asian oversample to NHANES 2013–2014 on observed trends in skeletal status between 2005 and 2014. Specifically, trends in the prevalence of osteoporosis and low bone mass by survey period were re-examined after limiting the analytic sample to non-Hispanic whites only. Results and conclusions were similar to those observed without restricting the sample to non-Hispanic whites, so results for trends are shown for the full analytic sample. Another sensitivity analysis was performed to assess the impact of the change in software used to process femur scans between NHANES 2005–2010 (Discovery 12.4 software) and 2013–2014 (Apex 4.0 software). Prediction equations derived from the NHANES 2005–2010 Hip Re-analysis Study (Supplementary Table 3) were used to calculate predicted “Apex 4.0” femur neck BMD values for NHANES 2005–2010. The predicted femur neck BMD values for NHANES 2005–2010 were then used to re-examine linear and quadratic trends in femur neck osteoporosis and low bone mass between all four survey periods. Conclusions regarding trends based on predicted Apex 4.0 femur neck BMD values for NHANES 2005–2010 were the same as when based on femur neck BMD values produced by the Discovery software in NHANES 2005–2010.
A sensitivity analysis was also performed to assess potential non-response bias in the analytic sample, since 24% of the examined sample of adults aged 50 years and older had been excluded from the main analytic sample due to missing femur neck or lumbar spine BMD. In this analysis, the publicly released examination sample weights were adjusted for item non-response using the PROC WTADJUST procedure in SUDAAN. We used this model-based calibration procedure to reweight the data by computing non-response and post-stratification weight adjustments by age, sex, and race/Hispanic origin in order to adjust for biases associated with these variables. The adjusted sample weights resulted in similar conclusions to those seen when the publicly released examination sample weights were used, so only the latter results are shown.
Finally, a sensitivity analysis was performed to assess the effect of using the 2010 Census population on age-adjusted results rather than the 2000 Census population. Results differed by less than 1 percentage point.
Results
The observed, or unadjusted, prevalence of osteoporosis and low bone mass at the femur neck, lumbar spine, and either the femur neck or lumbar spine among older adults in 2013–2014 is shown in Table 1. Overall, the observed prevalence of osteoporosis ranged from 6 to 11% (roughly 7–12 million adults), while the prevalence of low bone mass ranged from 28 to 45% (approximately 29–47 million adults), depending on the skeletal variable considered. The prevalence of both conditions was significantly higher in women (10–17% with osteoporosis; 36–53% with low bone mass) than in men (3–5% with osteoporosis; 19–36% with low bone mass) for all three skeletal variables. Age-adjusted prevalences using the direct method to either the 2000 or 2010 Census were roughly one percentage unit higher than the observed prevalences (data not shown).
The prevalence of osteoporosis and low bone mass at either the femur neck or lumbar spine in 2013–2014 are summarized by race/Hispanic origin and sex in Table 2. Differences in osteoporosis and low bone mass by race and Hispanic origin are illustrated for the combination of the femur neck and lumbar spine rather than for each skeletal site separately because the combined skeletal variable had statistically reliable estimates for the largest number of demographic subgroups. In women, the age-adjusted prevalence of osteoporosis at the femur neck or lumbar spine was highest in non-Hispanic Asians, intermediate in non-Hispanic whites and Hispanics, and lowest in non-Hispanic blacks (Table 2). After adjusting for age, non-Hispanic white and Hispanic women had a significantly higher prevalence of low bone mass at either site than non-Hispanic black women, but the age-adjusted low bone mass prevalence did not differ significantly between women in the other race/Hispanic groups. In men, the age-adjusted prevalence of osteoporosis at the femur neck or lumbar spine was significantly lower in non-Hispanic blacks than in non-Hispanic whites or non-Hispanic Asians. Low bone mass at either skeletal site was significantly higher in non-Hispanic white, Hispanic, and non-Hispanic Asian men than in non-Hispanic black men after adjusting for age. Non-Hispanic Asian men also had a significantly higher prevalence of low bone mass at either skeletal site than non-Hispanic white men.
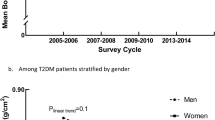
Unadjusted trends in mean femur neck and lumbar spine T-scores between 2005–2006 and 2013–2014 are shown in Fig. 2 by sex and survey period. There was a significant quadratic trend in mean femur neck T-score across the survey periods in both men and women. The pattern was roughly an inverted U shape in both sexes, with the mean negative T-score being closer to zero, and thus indicating better skeletal status, in the middle two survey periods than in the first or last survey period. Pairwise comparisons revealed the negative femur neck T-score was significantly further from zero in 2013–2014 than in 2007–2008 (by 0.20–0.21 units) or 2009–2010 (by 0.13–0.15 units) in both sexes (data not shown). There was no significant linear or quadratic trend in mean lumbar spine T-score during the same time period in either sex, however. Adjusting for age, race/Hispanic origin, and the selected bone-related lifestyle factors did not alter conclusions regarding trends in mean T-score at either skeletal site (data not shown).
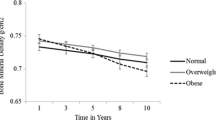
Trends in osteoporosis and low bone mass by survey period are shown separately by sex for the femur neck and lumbar spine before and after adjusting for selected risk factors in Table 3. Consistent with findings for mean T-scores, significant trends in poor skeletal status were confined to the femur neck. There were significant quadratic trends in the unadjusted prevalence of femur neck osteoporosis in both sexes. However, pairwise differences in femur neck osteoporosis between individual survey periods were confined to women, in whom prevalence in 2007–2008 was significantly lower than in 2005–2006 or 2013–2014. Adjusting for selected risk factors did not alter conclusions regarding femur neck osteoporosis trends in men, but in women, the quadratic trend was no longer statistically significant (p < 0.06).
There was also a significant quadratic trend in the unadjusted prevalence of low femur neck bone mass in women (Table 3), with low bone mass at the femur neck being significantly lower in 2007–2008 than in 2013–2014. After adjusting for selected risk factors, the trend in women became linear in shape and more pairwise comparisons became statistically significant. Specifically, adjusted femur neck low bone mass in women was significantly lower in both 2007–2008 and 2009–2010 when compared to 2013–2014.
Trends in the selected risk factors used in the multivariate models were examined in order to explore possible reasons for the observed trends in skeletal status. Mean age did not differ significantly between survey periods in either sex (data not shown). Figure 3 illustrates age-adjusted trends in other risk factors that were examined in the present study. There was no significant trend in the prevalence of self-reported physician’s diagnosis of osteoporosis in either sex. Trends in the other risk factors differed by sex. Smoking declined significantly between 2005–2006 and 2013–2014 in men, but not in women. In contrast, among men, there were no trends in the proportion who drank milk or who had BMI ≥ 25, but in women, milk intake declined significantly over the relevant time period, while the proportion with BMI ≥ 25 increased significantly.
Discussion
We found evidence of a shift towards a higher prevalence of osteoporosis and low bone mass at the femur neck in older US adults since 2005. Specifically, the prevalence of low bone mass or osteoporosis at the femur neck was significantly higher in 2013–2014 than in 2007–2008 (by 1.1–6.6 percentage points) and, while not statistically different, somewhat higher (by 0.3–3.7 percentage points) than in 2005–2006 and 2009–2010 as well. These findings are consistent with results of a recent, preliminary analysis of Medicare data indicating that the decline in hip fracture incidence among older US adults seen through 2012 plateaued in 2013–2014 [4]. However, there was no evidence of a change in lumbar spine bone density during the same time frame in the present study.
The reason for the lack of consistent trends in bone density at the two skeletal sites is not clear. Bone loss patterns may differ between these two skeletal sites [16], which can lead to discrepancies in skeletal status [17]. Lumbar spine bone density measurements by DXA may also be more affected by artifacts such as aortic calcification and osteophytes, than the femur neck. Another possible factor for the inconsistent trends observed between femur neck and spine specific to the present study, namely a change in software to process femur scans but not spine scans between survey periods, seems unlikely to have played a role, since conclusions regarding femur neck trends were similar after adjusting for the software change.
To identify possible reasons for the observed femur neck BMD trends, we examined changes in demographic variables and a small number of bone-related risk factors (BMI, smoking, milk intake, self-reported physician’s diagnosis of osteoporosis) between survey periods. These variables had to be limited to variables for which data were available at the time of the present study as well as ones that had been measured comparably in all four survey cycles. Adjusting for changes in these variables did not appreciably alter conclusions regarding trends, as would be expected if these factors played a major role in the observed changes in skeletal status. This is perhaps not surprising, given that, of the trends in confounding variables considered, only the trend in milk intake among women changed in a manner consistent with reduced bone density (e.g., milk intake declined in women during the time period between 2005 and 2014).
Concerns have been raised recently regarding recent trends in medical care for osteoporosis in the USA due to changes in Medicare reimbursement for DXA that were implemented in 2007 [18–24]. Additionally, others have noted a decline in bisphosphonate prescriptions between 2007–2008 and 2012 in the USA [25], which coincided temporally with increases in media reports and Internet searches about safety concerns associated with these drugs in an ecological analysis [26]. Trends in medical care for osteoporosis could potentially underlie the trend in femur neck osteoporosis observed in the present study. However, our ability to examine this possibility was limited to trends in self-reported physician’s diagnosis of osteoporosis, which did not change between survey periods. However, it is important to note that agreement between osteoporosis diagnosis data between self-report and medical records is moderate at best [27, 28]. Other variables related to medical care of osteoporosis that would allow a more detailed examination of this possibility were either not collected (e.g., medical records) or not available for the NHANES 2013–2014 survey cycle at the time of analysis (e.g., prescription medication use).
Introduction of oversampling of non-Hispanic Asians in NHANES 2013–2014 could theoretically have an impact on observed trends, since Asians generally have lower BMD than non-Asians [29, 30]. However use of sample weights in analyses ensured that trend results reflected the proportion of non-Hispanic Asians in the total population, which was estimated as 4.9% in 2012, and this small proportion is unlikely to be able to shift the BMD distribution of the overall population. In addition, similar trends were observed in secondary analysis which focused on non-Hispanic whites only, which further suggests that the introduction of oversampling of Asians in 2013–2014 did not account for the observed trends.
In addition to examining trends in bone density since 2005, the present study also provided more recent estimates of osteoporosis and low bone mass at the femur neck and lumbar spine (both separately and in combination) than previously available. The observed, or unadjusted, prevalence estimates varied depending on the skeletal site considered and was higher when based on BMD at the two skeletal sites in combination. For example, the observed, or unadjusted, prevalence of osteoporosis for adults aged 50+ was 6% for the femur neck alone, 8% for the lumbar spine alone, and 11% for either the femur neck or lumbar spine. The age-adjusted prevalence of osteoporosis (12%) and low bone mass (45%) at either the femur neck or lumbar spine in 2013–14 observed in the present study were slightly higher than the age-, sex-, and race/ethnic-adjusted prevalences of osteoporosis (10%) and low bone mass (44%) reported by Wright et al. for NHANES 2005–2010 [6]. However, it is important to note that results for the combination of femur neck and spine in the present study are not directly comparable with those published by Wright et al. [6] due to differences in the analytic approach between the studies. For example, Wright et al. [6] provided an estimate that was adjusted to 2010 using data collected in 2005–2010, whereas the present study examined prevalence in each survey cycle separately. The estimates in Wright et al. [6] were also adjusted to the age, sex, and race/ethnic composition of the total US population in 2010, while estimates in the present study were adjusted to the age composition of the non-institutionalized US civilian population, which corresponds more strictly to the population that NHANES is designed to represent.
This study also provides the first nationally representative estimates of osteoporosis and low bone mass at either the femur neck or lumbar spine in non-Hispanic Asians. We found that the age-adjusted prevalence of osteoporosis at either skeletal site was higher in non-Hispanic Asian women than in all other race/Hispanic origin groups examined and that non-Hispanic Asian men had a higher prevalence of low bone mass than both non-Hispanic white and non-Hispanic black men. It is important to note that these findings are based on a comparison of BMD values of non-Hispanic Asians with reference data from young non-Hispanic white women. Both WHO and ISCD have recommended that Caucasian reference data be used when diagnosing these conditions in non-whites [9, 12]. However some researchers have questioned the use of Caucasian reference data to define low skeletal status in Asians, in light of their smaller body size and lower hip fracture risk [2]. Since Asians have lower BMD than many non-Asian groups, use of Asian reference data results in lower prevalence estimates. For example, Walker et al. [31] found that prevalence estimates of osteoporosis at the lumbar spine and femur neck, when considered separately, in older Chinese American women were 16–17 percentage units lower when based on young Chinese American female reference data than on Caucasian data. However, it is not clear whether Asians have a lower risk of fracture at all skeletal sites, as some studies have found similar or higher vertebral fracture risk in Asians as in Caucasians [32, 33]. Furthermore, the non-Hispanic Asian group in NHANES 2013–2014 consisted of a mixture of different Asian groups, including individuals of Chinese, Asian Indian, Korean, Filipino, Vietnamese, and Japanese descent. There are some data to suggest that BMD may vary between Asian subgroups, which complicates the choice of the appropriate Asian reference database to use for a group with this mixture.
Study limitations include the ability to examine the impact of only a limited number of potential explanatory variables for observed trends, either because they were not available for use at the time of the present study for all four survey periods or because they were not measured. Furthermore, while trend tests indicated that significant trends in femur neck BMD had occurred overall and the magnitude of the prevalence of low femur neck status was higher in 2013–2014 than in the earlier survey cycles, statistically significant differences were primarily limited to differences observed between 2013–2014 and 2007–2008. Thus, it is possible that the prevalences observed in one of these two periods reflects a random fluctuation in femur neck status. Data on femur neck status from future cycles of NHANES can likely provide better clarification of the nature of trends in femur neck status.
Other limitations include possible non-response bias in the estimates. Non-response bias due to refusal to participate in the physical examinations in NHANES is reduced by a non-response adjustment factor included in the calculation of the sample weights for use with examinee data. However, 24% of examined respondents did not have usable femur and spine BMD data, and this is not addressed by those sample weight adjustments. Results from the analysis in which sample weights were adjusting for missing data by age, sex, and race/Hispanic origin in the analytic sample produced similar results as those based on the publicly available sample weights, which suggests that non-response bias in these demographic variables was not likely affecting results. These analyses do not address non-response bias due to other factors, however. Finally, institutionalized people, an important at-risk group for osteoporosis, are not included in the NHANES sampling frame by design.
In conclusion, the prevalence of femur neck osteoporosis in older US adults was significantly higher in 2013–2014 than in 2007–2008, which is consistent with a recent report indicating that hip fracture incidence among older US adults may have stopped declining as of 2013–2014 [4]. However, lumbar spine status did not change during the same time period. The reason for the discrepancy between observed trends in femur neck versus lumbar spine status is not clear. Adjusting for changes in body mass index, smoking, milk intake, and physician’s diagnosis of osteoporosis between surveys did not appreciably alter conclusions about the femur neck BMD trend, which suggests these factors cannot account for the observed increase in poorer BMD status. The present study also updated osteoporosis estimates to 2013–2014 for US adults aged 50 years and older, in whom the prevalence of osteoporosis was 6% at the femur neck, 8% at the lumbar spine, and 11% at either skeletal site.
Notes
Data from NHANES III (1988–1994) were not included in the present study because proximal femur BMD was measured with pencil-beam DXA.
References
Looker AC, Melton LJ, Harris TB, Borrud LG, Shepherd JA (2010) Prevalence and trends in low femur bone density among older US adults: NHANES 2005–2006 compared with NHANES III. J Bone Miner Res 25:64–71
Wright NC, Saag KG, Curtis JR, Smith WK, Kilgore ML, Morrisey MA, Yun H, Zhang J, Delzell ES (2012) Recent trends in hip fracture rates by race/ethnicity among older US adults. J Bone Miner Res 27:2325–2332
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB (2009) Incidence and mortality of hip fractures in the United States. JAMA 302:1573–1579
Lewiecki EM, Curtis J, Gagel R, Saag K, Singer A, Siris E, Wright NC, Yun H, Steven PM (2016) Hip fractures and declining DXA testing: at a breaking point? J Bone Miner Res 31(Suppl 1). http://www.asbmr.org/education/AbstractDetail?aid=2af8747d-5eaa-48e0-a47f-1dfd676dbccb. Accessed 3 Oct 2016
Looker AC, Borrud LG, Dawson-Hughes B, Shepherd JA, Wright NC (2012) Osteoporosis or low bone mass at the femur neck or lumbar spine in older adults: United States, 2005-2008. NCHS Data Brief 93:1–8 https://www.cdc.gov/nchs/products/databriefs/db93.htm. Accessed 19 Oct 2016
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29:2520–2526
Johnson CL, Dhormann S, Burt VL, Mohadjer LK (2014) National Health and Nutrition Examination Survey: sample design, 2011–2014. National Center for Health Statistics, Hyattsville http://www.cdc.gov/nchs/data/series/sr_02/sr02_162.pdf. Accessed 19 Oct 2016
Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J (2013) National Health and Nutrition Examination Survey: plan and operations, 1999–2010. National Center for Health Statistics, Hyattsville http://www.cdc.gov/nchs/data/series/sr_01/sr01_056.pdf. Accessed 19 Oct 2016
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J Clin Densitom 16:455–466
Centers for Disease Control and Prevention National Center for Health Statistics (2007) Dual energy X-ray absorptiometry (DXA) procedures manual. Centers for Disease Control and Prevention, National Center for Health Statistics. http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_dexa.pdf. Accessed 19 Oct 2016
Fan B, Lewiecki EM, Sherman M, Lu Y, Miller PD, Genant HK, Shepherd JA (2008) Improved precision with Hologic Apex software. Osteoporos Int 19:1597–1602
Kanis JA, Melton LJ, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC Jr, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489
National Center for Health Statistics Key concepts about age standardization. https://www.cdc.gov/nchs/tutorials/Nhanes/NHANESAnalyses/AgeStandardization/Info1.htm. Accessed 19 Oct 2016
Klein RJ SC (2001) Age adjustment using the 2000 projected population. Healthy People Statistical Notes, no. 20. USDHHS, Centers for Disease Control and Prevention, National Center for Health Statistics. https://www.cdc.gov/nchs/data/statnt/statnt20.pdf. Accessed 19 Oct 2016
Riggs BL, Melton LJ, Robb RA, Camp JJ, Atkinson EJ, Peterson JM, Rouleau PA, McCollough CH, Bouxsein ML, Khosla S (2004) Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res 19:1945–1954
Looker AC, Melton LJ 3rd, Borrud LG, Shepherd JA (2012) Lumbar spine bone mineral density in US adults: demographic patterns and relationship with femur neck skeletal status. Osteoporos Int 23:1351–1360
Miller PD (2016) Underdiagnoses and undertreatment of osteoporosis: the battle to be won. J Clin Endocrinol Metab 101:852–859
Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, Krohn KD (2014) Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res 29:1929–1937
Zhang J, Delzell E, Zhao H, Laster AJ, Saag KG, Kilgore ML, Morrisey MA, Wright NC, Yun H, Curtis JR (2012) Central DXA utilization shifts from office-based to hospital-based settings among Medicare beneficiaries in the wake of reimbursement changes. J Bone Miner Res 27:858–864
Yoo JW, Nakagawa S, Kim S (2012) Effect of reimbursement reductions on bone mineral density testing for female Medicare beneficiaries. J Womens Health (Larchmnt) 21:1144–1148
Hayes BL, Curtis JR, Laster A, Saag K, Tanner SB, Liu C, Womack C, Johnson KC, Khaliq F, Carbone LD (2010) Osteoporosis care in the United States after declines in reimbursements for DXA. J Clin Densitom 13:352–360
O’Malley CD, Johnston SS, Lenhart G, Cherkowski G, Palmer L, Morgan SL (2011) Trends in dual-energy X-ray absorptiometry in the United States, 2000-2009. J Clin Densitom 14:100–107
Intenzo CM, Parker L, Levin DC, Kim SM, Rao VM (2016) Provider distribution changes in dual-energy X-ray absorptiometry in the Medicare population pver the past decade. J Clin Densitom 19:266–269
Wysowski DK, Greene P (2013) Trends in osteoporosis treatment with oral and intravenous bisphosphonates in the United States, 2002-2012. Bone 57:423–428
Jha S, Wang Z, Laucis N, Bhattacharyya T (2015) Trends in media reports, oral bisphosphonate prescriptions, and hip fractures 1996–2012: an ecological analysis. J Bone Miner Res 30:2179–2187
Simpson CF, Boyd CM, Carlson MC, Griswold ME, Guralnik JM, Fried LP (2004) Agreement between self-report of disease diagnoses and medical record validation in disabled older women: factors that modify agreement. J Am Geriatr Soc 52:123–127
Peeters GMEE, Tett SE, Dobson AJ, Mishra GD (2013) Validity of self-reported osteoporosis in mid-age and older women. Osteoporos Int 24:917–927
Ip TP, Cheung SK, Cheung TC et al (2013) The Osteoporosis Society of Hong Kong (OSHK): 2013 OSHK guideline for clinical management of postmenopausal osteoporosis in Hong Kong. Hong Kong Med J 19(Suppl 2):1–40
Nam HS, Kweon SS, Choi JS, Zmuda JM, Leung PC, Lui L-Y, Hill DD, Patrick AL, Cauley JA (2013) Racial/ethnic differences in bone mineral density among older women. J Bone Miner Metab 31:190–198
Donovan Walker M, Babbar R, Opotowsky AR et al (2006) A referent bone mineral density database for Chinese American women. Osteoporos Int 17:878–887
Bow CH, Cheung E, Cheung CL et al (2011) Ethnic difference of clinical vertebral fracture risk. Osteoporos Int 23:879–885
Tsang SWY, Bow CH, Chu EYW, Yeung SC, Soong CC, Kung AWC (2011) Clinical risk factor assessment had better discriminative ability than bone mineral density in identifying subjects with vertebral fracture. Osteoporos Int 22:667–674
Acknowledgements
Financial support for the collection of osteoporosis-related data in NHANES 2005–2010 was provided by the National Institute of Arthritis, Musculoskeletal and Skin Diseases, National Institutes of Health through an interagency agreement, and in NHANES 2013–2014 by Eli Lilly and Company through a grant to the CDC Foundation. Eli Lilly and Company had no role in the collection of the data, the production of the public use datasets for NHANES 2013–2014, or the design and conduct of the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Required disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Looker, A.C., Sarafrazi Isfahani, N., Fan, B. et al. Trends in osteoporosis and low bone mass in older US adults, 2005–2006 through 2013–2014. Osteoporos Int 28, 1979–1988 (2017). https://doi.org/10.1007/s00198-017-3996-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-3996-1




 ) women (
) women ( ) men
) men