Abstract
Summary
Studies examining recent bone mineral density (BMD) trends in the US population are limited. In our study, we found that age-adjusted mean BMD among US men and women was stable from 2005 to 2010, but then declined in 2013–2014. We also explored factors associated with decreasing BMD in recent years.
Introduction
Osteoporosis prevalence in the USA declined between 1988 and 2006, while the declining trend in hip fracture may have plateaued in 2013–2014. We aimed to examine whether there has been a corresponding change in BMD trajectory for the US population.
Methods
Continuous National Health and Nutrition Examination Survey (NHANES) data from 2005–2006 to 2013–2014 were analyzed to examine BMD trends among US men and women aged 30 years and older and among different race/ethnicity subgroups. ANOVA and Bonferroni adjustments were used to examine the differences in mean BMD, and multiple linear regressions adjusting for potential confounding effects were employed to examine BMD trends.
Results
After age standardization, the mean BMD of the femur neck for the first three NHANES cycles was stable (all p > 0.1) in both men and women, but significantly decreased in 2013–2014, from 0.864 g/cm2 to 0.846 g/cm2 (p = 0.0025) in men and from 0.789 to 0.771 g/cm2 (p = 0.03) in women. The overall mean femur neck BMD in 2013–2014 was significantly lower than that in earlier survey cycles in both men and women, even after adjusting for multiple covariates, including age, race, physical activity, previous fracture, BMI, and other variables. Similar results were observed in subgroup analyses of race and sensitivity analyses.
Conclusions
Age-adjusted mean BMD decreased in 2013–2014 in both men and women, and this significant decrease was also observed in sensitivity and subgroup analyses. The decreased BMD in 2013–2014 still remained significant even after being adjusted for multiple potentially confounding effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis affects approximately 200 million people across the world [1]. In the USA alone, around 54 million people have osteoporosis or low bone mass [2]. Both conditions are associated with an increased risk of fracture [3]. It has been estimated that the number of osteoporotic fractures will grow by almost 50% to more than 3 million cases by 2025 and will cause the USA 25.3 billion dollars in economic loss [4]. Meanwhile, fractures often result in serious disability and excess mortality for patients [3]. The high prevalence of osteoporosis and the associated adverse impacts make this condition a major public health issue in this country.
The prevalence of osteoporosis among people aged 50 years and older appeared to decline between 1988 and 1994 and 2005 and 2006 [5]. However, a research from the US Medicare Database suggested that the decreasing trend in hip fracture incidence may have ended in 2013–2014 [6]. Since the hip fracture is considered as one of the most common manifestations of osteoporosis [4], this research might indicate the end of the decreasing trend of the disease. As BMD is the single most important predictor of osteoporotic fracture [7], identifying whether there has been a corresponding change in BMD trajectory for the US population in the past decade is imperative to understanding bone health and to the prevention of osteoporosis and fracture in the US population.
Although a recent study utilized BMD to examine the prevalence of osteoporosis and low bone mass from 2005 to 2006 to 2013 to 2014 [8], the research focused on the population aged 50 years and older. In addition, other related studies also have placed more emphasis on older people [9, 10]. Hence, the purpose of our study was to examine the bone health in an extensive population, including adults under 50 years of age. The aforementioned study also examined osteoporosis and low bone mass defined by the T-score method, in which the corresponding variable was a categorical variable. While using a categorical variable for the outcome has some advantages, studies found that transferring continuous variables into categorical variables may lead to information loss or other problems [11]. In our study, we directly utilized BMD to track the change in bone health, which would help to minimize loss of information. Furthermore, the mean BMD differences between the four survey cycles for men and women were examined after adjusting for potentially confounding effects, and possible explanations for the observed BMD trends were also explored.
Methods
Data source
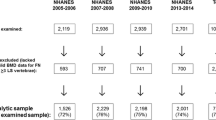
Data were obtained from continuous NHANES, which is a nationally representative cross-sectional survey of non-institutionalized civilian persons in the USA. NHANES is conducted by the National Center for Health Statistics at the Centers for Disease Control and Prevention (CDC) to examine collected data from approximately 5000 individuals across the country every 2 years [12]. The participants are selected by a complex, probability sampling design, and interviews and examination are conducted to obtain information on each participant. The interview includes demographic, socioeconomic, dietary, and health-related questions, while the examination consists of medical, dental, and physiological measurements. From 2005 to 2006, the survey started measuring the femur and spine BMD, but BMD was not measured for NHANES in 2011–2012. Therefore, only four cycles (2005–2006, 2007–2008, 2009–2010, and 2013–2014) of data were included in the analysis for this study. Subjects less than 30 years of age were excluded from the analysis to ensure that the sample included only those who had reached their peak BMD, since bone formation exceeds resorption until age 30 and BMD normally peaks at that time [13]. Subjects who lacked valid BMD data were also excluded.
BMD measurement
BMD was measured by dual-energy X-ray absorptiometry (DXA), the examination protocol for which is described in detail elsewhere [14]. The femur and spine scans in 2005–2006 through 2009–2010 were performed with a Hologic QDR-4500A fan-beam densitometer and with a Hologic Discovery model A densitometer (Hologic, Inc., Bedford, MA, USA) in 2013–2014. The femur scans in 2005–2010 were analyzed with Hologic Discovery v12.4, and the spine scans were analyzed with APEX v3.0. In the 2013–2014 segment, both femur and spine scans were analyzed with APEX v4.0. The Hologic Service Team performed a cross-calibration procedure to standardize the newer system to the legacy system [15]. A previous study assessed five femur regions and confirmed that there was no difference between mean BMD analyzed by Discovery 12.4 and by Apex 4.0 at the femur neck [8]. Because BMD measurement with DXA at the femur neck has the highest predictive value for hip fracture, and the hip is the site of highest clinical relevance [16], our study focused on analyzing the femur neck BMD data. However, to assess the robustness of our findings, we conducted a sensitivity analysis by examining BMD trends of total hip and total spine in the data. We also conducted a separate sensitivity analysis to examine femur neck BMD trends across the four survey cycles when limiting the age of participants to 40 years and above.
Demographic variables
Age, sex, and race/ethnicity were ascertained by questionnaire. For the race/ethnicity groups, “Mexican American” and “Other Hispanic” were merged into “Hispanic,” and the remaining groups were “non-Hispanic White,” “non-Hispanic Black,” and “non-Hispanic other,” respectively.
Clinical characteristics
BMD-related variables, including previous fracture [17], renal function [18], hypertension [19], family history of osteoporosis [20], physical activity [7], smoking status [21], rheumatoid arthritis [22], thyroid disease [23], thiazide diuretics use [24], bisphosphonate use [25], diabetes [26], insulin use [27], BMI [28], hormone therapy (women only) [29], menopausal status (women only), and oral contraceptives use (premenopausal women only) were considered for analysis [30, 31]. These variables were selected based on literature review as well as availability in the continuous NHANES data. Individuals who had suffered a broken or fractured hip, wrist, or spine were considered as having a previous fracture. Since mineral and bone disorder may happen among people with chronic kidney (CKD), the serum creatinine levels of subjects were used to estimate glomerular filtration rates (GFRs), which were then used to stratify their renal function within five stages: normal, mild CKD, moderate CKD, severe CKD, and end-stage [18]. Subjects were considered to have hypertension if they answered “yes” to the question “Have you ever been told by a doctor or other health professional that you had hypertension, also called high blood pressure?” In the present study, the participants were defined as having a family history of osteoporosis if their parent(s) ever had osteoporosis. Self-reported physical activity was categorized as “inactive” and “active.” Participants who were sedentary or only did basic activities, which refers to the light-intensity activities like standing and walking slowly, were considered to be inactive; otherwise, the individuals were classified as active [32]. Smoking status was categorized into current smokers, former smokers, and non-smokers [33]. Current smokers were respondents who had smoked at least 100 cigarettes during their lifetime and, at the time of the interview, who reported smoking either every day or some days. Former smokers were those who reported smoking at least 100 cigarettes during their lifetime but who currently did not smoke. Lastly, subjects who had not smoked 100 cigarettes during their lifetime were defined as non-smokers. Information about use of prescription drugs was collected by the questionnaire that focused on whether participants had used the medicine within the past month. Participants who have taken thiazide or a thiazide-like drug were defined as users of thiazide diuretics, while those who had not were defined as non-users. Participants who had taken bisphosphonates (including alendronate, etidronate, ibandronate, risedronate, and zoledronic acid) were classified as users of bisphosphonates [34]; otherwise, participants were classified as non-users. Subjects were categorized as insulin users if they were taking insulin at the time of the interview; otherwise, they were categorized as non-users. Body mass index (BMI) was derived from measured weight in kilograms divided by the square of height in meters. Women could be categorized as premenopausal, surgically menopausal, and naturally menopausal [35]. However, because we could not distinguish natural menopause and surgical menopause (hysterectomy) based on the questionnaire of NHANES, the menopausal status of women was dichotomously classified as premenopausal and postmenopausal.
Statistical analysis
All study analyses employed sampling weights to account for unequal selection probabilities, non-response, and non-coverage [36]. In order to allow the age profiles of the population to be comparable, the age-adjusted estimation of BMD was calculated by the direct method, using the US 2000 census as the standard population. The age-adjusted mean BMD at the femur neck and its 95% confidence interval in every survey cycle for each sex was calculated, as well as the race/ethnicity-specific age-adjusted mean BMD of each gender. Standard errors, which were employed to construct confidence intervals, were estimated using Taylor series linearization. After checking the assumptions for statistical testing, analysis of variance (ANOVA) was utilized to examine the difference in mean BMD over the four survey cycles, and Bonferroni adjustments were used for multiple comparisons between the four survey cycles (6 comparisons), with α = 0.05/6 = 0.0083. To test for linear trends in each sex over the four survey cycles, the null hypothesis of no linear trend was examined by using orthogonal contrast. The frequency distributions of BMD from the four survey cycles by sex were generated for graphical comparison. A separate stepwise model (with the p value for entry set at 0.15 and that for stay at 0.20) was employed in the selection of variables to predict BMD for each sex. Multiple linear regression was used to examine the association between a given independent variable and BMD, while holding other variables constant, and the standardized coefficient from linear regression was employed to examine the relative importance of each variable in the regression model for BMD prediction. Survey cycle was included as a categorical variable in the multiple linear regression in order to determine if the mean BMD in 2013–2014 differed from that in previous survey cycles after adjusting for major confounders. All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
The total number of eligible individuals across the four NHANES survey cycles was 14,188 and their characteristics are presented in Table 1. From 2005 to 2006 to 2013 to 2014, the percentage of women among participants increased from 46.33 to 50.56%; for non-Hispanic other, the percentage rose from 4.2 to 13.88%, while the percentage of non-Hispanic White decreased from 53.85 to 43.94%. The mean age increased in all subgroups, especially in both Hispanic and non-Hispanic other, whose mean ages increased the most. Mean BMI was stable in most gender- and race/ethnicity-specific groups during the period of 2005–2014. The distribution of risk factors related to BMD for men and women are shown in Table 2. Over the four survey cycles, the percentage of hypertensive patients increased from 35.46 to 45.08% in men and from 37.76 to 48.96% in women. Meanwhile, the percentage of physical inactivity increased from 5.87 to 22.38% in men and from 9.59 to 31.82% in women, and the percentage of self-reported diabetes increased approximately 6% for both men and women. The percentage of postmenopausal women was similar from 2005 to 2006 to 2013 to 2014, while the percentage of oral contraceptive use increased from 33.01 to 38.71%.
The mean BMD and the distribution of BMD by gender in the four survey cycles are presented in Fig. 1. Orthogonal contrast tests demonstrated that significant linear trends existed in the unadjusted mean BMD over the four cycles in each gender group (Fig. 1a, all P linear trend < 0.001). The decreased unadjusted mean BMD in 2013–2014 corresponded to the left shift of the BMD distribution (Fig. 1b, c).
Unadjusted mean bone mineral density and distribution of bone mineral density by sex, NHANES from 2005 to 2006 to 2013 to 2014. a Mean bone mineral density and linear trend in 2005–2014. b Distribution of bone mineral density in men, 2005–2014. c Distribution of bone mineral density in women, 2005–2014
Age-adjusted mean BMD
The age-adjusted mean femur neck BMDs of men and women, as well as the race/ethnicity-specific subgroups of each gender in the four survey cycles, are presented in Table 3. In men, the age-adjusted mean BMD of non-Hispanic other men was the lowest across all four survey cycles. We also observed a significant decrease in the age-adjusted BMD among overall (p = 0.0025, ANOVA) and in non-Hispanic White men (p = 0.0004, ANOVA). The overall age-adjusted mean BMD in men was similar in the first three survey cycles: 0.864 g/cm2 (95% CI, 0.857 g/cm2–0.871 g/cm2) in 2005–2006, 0.866 g/cm2 (95% CI, 0.858 g/cm2–0.873 g/cm2) in 2007–2008, and 0.867 g/cm2 (95% CI, 0.857 g/cm2–0.878 g/cm2) in 2009–2010. No significant differences were found between the first three survey cycles in men (all p > 0.5, Bonferroni adjustments). However, the overall age-adjusted mean BMD of men decreased significantly to 0.846 g/cm2 (95% CI, 0.837 g/cm2–0.853 g/cm2) in 2013–2014. The differences between the last survey cycle and each of the first three survey cycles in men were significant (all p < 0.0024, Bonferroni adjustments). In non-Hispanic White men, the age-adjusted mean BMD from 2005 to 2006 to 2009 to 2010 was 0.854 g/cm2 (95% CI, 0.846 g/cm2–0.862 g/cm2), 0.856 g/cm2 (95% CI, 0.845 g/cm2–0.866 g/cm2), and 0.859 g/cm2 (0.846 g/cm2–0.871 g/cm2), respectively and decreased to 0.832 g/cm2 (95%CI, 0.821 g/cm2–0.842 g/cm2) in 2013–2014. In non-Hispanic White men, the age-adjusted mean BMD in 2013–2014 was significantly lower than that in each of the first three survey cycles (all p ≤ 0.0007, Bonferroni adjustments).
For women, a significant difference in the overall age-adjusted mean BMD was observed in the four survey cycles (p = 0.03, ANOVA). In 2005–2006, the overall age-adjusted mean BMD was 0.780 g/cm2 (95% CI, 0.774 g/cm2–0.787 g/cm2); in 2007–2008, it was 0.789 g/cm2 (95% CI, 0.780 g/cm2–0.798 g/cm2); in 2009–2010, it was 0.784 g/cm2 (95% CI, 0.776 g/cm2–0.791 g/cm2); and in 2013–2014, the overall age-adjusted mean BMD significantly decreased to 0.771 g/cm2 (95% CI, 0.762 g/cm2–0.779 g/cm2). A significant difference in the age-adjusted mean BMD was observed in women between 2007 and 2008 and 2013 and 2014 (p = 0.0046, Bonferroni adjustments).
Our sensitivity analysis found that the age-adjusted mean BMD in the total spine and in the total femur were similar to those of the femur neck. For men, the overall age-adjusted mean BMD of the total spine varied little (1.054–1.061 g/cm2) from 2005 to 2006 to 2009 to 2010 but then declined to 1.042 g/cm2 in 2013–2014. Similarly, for women, the overall age-adjusted mean BMD of the total spine was stable in the first three survey cycles (0.992–0.995 g/cm2) but then declined to 0.987 g/cm2 in 2013–2014. Additionally, for men, the overall age-adjusted mean BMD of the total femur in the first three NHANES cycles was stable between 1.013 and 1.016 g/cm2 but declined to 1.00 g/cm2 in 2013–2014. However, for women, the overall age-adjusted mean BMD of the total femur varied little over the four survey cycles (0.900–0.910 g/cm2). When the analysis was limited to participants 40 years of age and older, we observed similar results (Supplementary Tables 1 and 2).
Multiple linear regression
In men, the multiple linear regression indicated that older age, previous fracture, family history of osteoporosis, and physical inactivity were significantly associated with decreased BMD (all p < 0.0001; Table 4). In women, older age, previous fracture, physical inactivity, bisphosphonates use, and postmenopausal status contributed significantly to decreased BMD (all p < 0.0018; Table 5). The standardized coefficient from linear regression demonstrated that age was the most significant risk factor for decreased BMD in both men and women. Physical inactivity in men and postmenopausal status of women were also important factors that contributed to decreased BMD. The selected covariates in the multiple linear models explained approximately 28% of femur neck BMD variance in men and approximately 43% in women. After adjusting for these major confounders, the multivariate adjusted mean BMD in 2013–2014 was still significantly lower than that of each survey cycle from 2005 to 2006 to 2009 to 2010 in both men (p ≤ 0.004; Table 4) and women (p < 0.0001; Table 5).
Discussion
In this study, we found that the age-adjusted mean BMD of the femur neck was stable from 2005 to 2006 to 2009 to 2010 but significantly decreased in 2013–2014 for both men and women. In addition, our sensitivity analyses found a similar trend of BMD when using BMD data either from the total spine or from the total femur. Similar results were also observed when we limited the analysis to participants 40 years of age and older. Finally, our multiple regression analyses demonstrated that the decreased BMD in 2013–2014 was still significant in both men and women after controlling for multiple confounders, including age, race/ethnicity, fracture history, renal function, family history of osteoporosis, hypertension, physical activity, alcohol consumption, and BMI. Although the BMD change in recent years is small, these consistent results indicate a future downward shift of Americans’ bone health may be occurring in both men and women.
Our research also corresponds to other studies in the field. Our findings were consistent with the study conducted by Dr. Lewiecki [6], which found that the decline in age-adjusted hip fracture incidence among US adults may have plateaued in 2013–2014. The declining age-adjusted BMD trend observed in this study may explain the changing trend of hip fracture incidence found in Dr. Lewiecki’s study, considering that BMD is a strong predictor of hip fracture [37]. As well, our findings also support the increased prevalence of osteoporosis and low bone mass found in a study done by Dr. Looker [8].
The results of the multiple linear regression indicated that age, race/ethnicity, renal function, previous fracture, BMI, and physical activity were significantly associated with BMD in both men and women, which is consistent with previous studies [7, 17, 28, 38, 39]. Most notably, the percentage of physical inactivity increased from 5.87 to 22.38% among men and from 9.59 to 31.82% among women. Considering that physical inactivity is associated with lower BMD and osteoporosis [7], the increased percentage for sedentary lifestyle across the four survey cycles might explain the decreasing BMD trend. In addition, bisphosphonates are effective for the prevention and treatment of osteoporosis [40]. However, we observed that taking this medication was negatively associated with BMD in women, which is likely because the medication was prescribed to these patients who already had lower bone mass, osteoporosis, or a broken bone. Furthermore, in 2008, the US Food and Drug Administration highlighted the possible connection between severe and sometimes incapacitating bone, joint, and/or muscle pain in patients taking bisphosphonates [25], while several reports found other adverse effects associated with bisphosphonates, including atypical fracture of the femur, osteonecrosis of the jaw, and esophageal cancer [41, 42]. These alerts may have led to less prescribing and less use of bisphosphonates, which has been found to be associated with decreased mean BMD in the population [43, 44]. In this study, we found that the percentage of bisphosphonate medication decreased from 3.1 to 1.9% in women, and the decreased trend of bisphosphonate use corresponded to the decreased BMD trend that we observed. The deceased BMD in 2013–2014 remained significant after considering a comprehensive list of BMD-related risk factors and controlling for major confounding effects in the multiple regression analysis. Nevertheless, it is highly likely that residual confounding existed. Additional studies are warranted in order to explain the recent BMD decline in the US population.
Our analyses have several limitations. First, many of the NHANES participants (aged 30 years and older) did not receive BMD testing due to hip fracture, pregnancy, or other reasons. However, the non-response in the examination data was accounted by sample weights in NHANES. Second, all of the NHANES participants were non-institutionalized. Since institutionalized persons may have lower bone mass [45], the actual mean BMD of individuals aged 30 years and older in this country may be lower than the estimate in this study. Nevertheless, this limitation is unlikely to have altered the significant decreased BMD in 2013–2014 observed in this study. Third, the effect of software updates on BMD measurements of the total femur and total spine in our sensitivity analysis was not clear. However, a previous study did confirm that the software updates had no impact on the femur neck BMD measurements [8]. Finally, information regarding dose and duration of bisphosphonate use was not available, as the NHANES questionnaire only focused on whether participants had used the medication within the past month. Hence, the effect of bisphosphonates could not be quantified accurately in this study.
In summary, from 2005 to 2006 to 2013 to 2014, a decreasing age-adjusted mean BMD trend was observed in both men and women. After adjusting for race/ethnicity, age, BMI, physical activity, alcohol consumption, bisphosphonate use, and other bone-related variables, the mean femur neck BMD in recent years (2013–2014) was still significantly lower than in earlier survey cycles. The physical inactivity among both men and women may contribute to the decreased age-adjusted BMD trend in 2013–2014. Additional studies are warranted to further explain the decreasing trend of BMD in order to determine proper prevention and treatment of osteoporosis in the USA.
Abbreviations
- NHANES:
-
National Health and Nutrition Examination Survey
- BMI:
-
Body mass index
- CDC:
-
Centers for Disease Control and Prevention
- DXA:
-
Dual-energy X-ray absorptiometry
- CKD:
-
Chronic kidney disease
- GFR:
-
Glomerular filtration rate
- ANOVA:
-
Analysis of variance
References
Kanis JA (2007) WHO technical report. University of Sheffield
National Osteoporosis Foundation (2014) 54 million Americans affected by osteoporosis and low bone mass. https://www.nof.org/news/54-million-americans-affected-by-osteoporosis-and-low-bone-mass/. Accessed 06/02 2017
Riggs BL, Melton LJ 3rd (1995) The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone 17(5 Suppl):505s–511s
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 22(3):465–475. https://doi.org/10.1359/jbmr.061113
Looker AC, Melton LJ 3rd, Harris TB, Borrud LG, Shepherd JA (2010) Prevalence and trends in low femur bone density among older US adults: NHANES 2005-2006 compared with NHANES III. J Bone Miner Res 25(1):64–71. https://doi.org/10.1359/jbmr.090706
Michael Lewiecki E, Wright NC, Curtis JR, Siris E, Gagel RF, Saag KG, Singer AJ, Steven PM, Adler RA (2017) Hip fracture trends in the United States, 2002 to 2015. Osteoporos Int 29:717–722. https://doi.org/10.1007/s00198-017-4345-0
Office of the Surgeon General (US) (2004) Bone health and osteoporosis: a report of the surgeon general. Assessing the Risk of Bone Disease and Fracture
Looker AC, Sarafrazi Isfahani N, Fan B, Shepherd JA (2017) Trends in osteoporosis and low bone mass in older US adults, 2005-2006 through 2013-2014. Osteoporos Int 28(6):1979–1988. https://doi.org/10.1007/s00198-017-3996-1
Coughlan T, Dockery F (2014) Osteoporosis and fracture risk in older people. Clin Med (Lond) 14(2):187–191. https://doi.org/10.7861/clinmedicine.14-2-187
Diab DL, Watts NB (2013) Postmenopausal osteoporosis. Curr Opin Endocrinol Diabetes Obes 20(6):501–509. https://doi.org/10.1097/01.med.0000436194.10599.94
Altman DG, Royston P (2006) The cost of dichotomising continuous variables. BMJ : British Medical Journal 332(7549):1080–1080
Centers for Disease Control and Prevention (CDC) (2017) About NHANES. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed 11/27 2017
NIH Osteoporosis and Related Bone Diseases National Rescource Center (2015) Osteoporosis: Peak Bone Mass in Women. https://www.bones.nih.gov/health-info/bone/osteoporosis/bone-mass. Accessed 06/02 2017
Centers for Disease Control and Prevention (CDC) (2009) Dual Energy X-ray Absorptiometry - Femur (DXXFEM_D). https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/DXXFEM_D.htm. Accessed 06/02 2017
Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N (2008) A reference standard for the description of osteoporosis. Bone 42(3):467–475. https://doi.org/10.1016/j.bone.2007.11.001
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312(7041):1254–1259
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15(4):721–739. https://doi.org/10.1359/jbmr.2000.15.4.721
KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Anemia in Chronic Kidney Disease (2006) Am. J Kidney Dis 47(5 Suppl 3):S11–S145. https://doi.org/10.1053/j.ajkd.2006.03.010
Nam H-S, Kweon S-S, Choi J-S, Zmuda JM, Leung PC, Lui L-Y, Hill DD, Patrick AL, Cauley JA (2013) Racial/ethnic differences in bone mineral density among older women. J Bone Miner Metab 31(2):190–198. https://doi.org/10.1007/s00774-012-0402-0
Orchard TS, Larson JC, Alghothani N, Bout-Tabaku S, Cauley JA, Chen Z, LaCroix AZ, Wactawski-Wende J, Jackson RD (2014) Magnesium intake, bone mineral density, and fractures: results from the Women’s Health Initiative observational study. Am J Clin Nutr 99(4):926–933. https://doi.org/10.3945/ajcn.113.067488
Mackey DC, Lui L, Cawthon PM et al (2007) High-trauma fractures and low bone mineral density in older women and men. JAMA 298(20):2381–2388. https://doi.org/10.1001/jama.298.20.2381
Lodder M, de Jong Z, Kostense P, Molenaar E, Staal K, Voskuyl A, Hazes J, Dijkmans B, Lems W (2004) Bone mineral density in patients with rheumatoid arthritis: relation between disease severity and low bone mineral density. Ann Rheum Dis 63(12):1576–1580. https://doi.org/10.1136/ard.2003.016253
Dhanwal DK (2011) Thyroid disorders and bone mineral metabolism. Indian J Endocrinol Metab 15(Suppl2):S107–S112. https://doi.org/10.4103/2230-8210.83339
Lim LS, Fink HA, Kuskowski MA, Cauley JA, Ensrud KE (2005) Diuretic use and bone mineral density in older USA men: the osteoporotic fractures in men (MrOS) study. Age Ageing 34(5):504–507. https://doi.org/10.1093/ageing/afi133
Lewiecki EM (2010) Bisphosphonates for the treatment of osteoporosis: insights for clinicians. Ther Adv Chronic Dis 1(3):115–128. https://doi.org/10.1177/2040622310374783
National Institute of Diabetes and Digestive and Kidnay Disease Mineral & Bone Disorder in Chronic Kidney Disease. https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd/mineral-bone-disorder. Accessed 04/09/2018
Thrailkill KM, Lumpkin CK, Bunn RC, Kemp SF, Fowlkes JL (2005) Is insulin an anabolic agent in bone? Dissecting the diabetic bone for clues. Am J Phys Endocrinol Metab 289(5):E735–E745. https://doi.org/10.1152/ajpendo.00159.2005
Rexhepi S, Bahtiri E, Rexhepi M, Sahatciu-Meka V, Rexhepi B (2015) Association of body weight and body mass index with bone mineral density in women and men from Kosovo. Materia Socio-Medica 27(4):259–262. https://doi.org/10.5455/msm.2015.27.259-262
Gartlehner G, Patel SV, Feltner C, Weber RP, Long R, Mullican K, Boland E, Lux L, Viswanathan M (2017) Hormone therapy for the primary prevention of chronic conditions in postmenopausal women: evidence report and systematic review for the US preventive services task force. JAMA 318(22):2234–2249. https://doi.org/10.1001/jama.2017.16952
Ertungealp E, Seyisoglu H, Erel CT, Senturk LM, Gezer A (1999) Changes in bone mineral density with age, menopausal status and body mass index in Turkish women. Climacteric 2(1):45–51
Prior JC, Kirkland SA, Joseph L, Kreiger N, Murray TM, Hanley DA, Adachi JD, Vigna YM, Berger C, Blondeau L, Jackson SA, Tenenhouse A, the CaMos Research Group f (2001) Oral contraceptive use and bone mineral density in premenopausal women: cross-sectional, population-based data from the Canadian multicentre osteoporosis study. CMAJ 165(8):1023–1029
National Heart L, and Blood Institute (1998) Clinical guidelines on the identification, Evaluation, and Treatment of Overweight and Obesity in Adults
Kahende JW, Adhikari B, Maurice E, Rock V, Malarcher A (2009) Disparities in health care utilization by smoking status—NHANES 1999–2004. Int J Environ Res Public Health 6(3):1095–1106. https://doi.org/10.3390/ijerph6031095
U.S. Food & Drug Administration (2017) Postmarket drug safety information for patients and providers. https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/default.htm. Accessed 06/02 2017
Nash D, Magder L, Lustberg M et al (2003) Blood lead, blood pressure, and hypertension in perimenopausal and postmenopausal women. JAMA 289(12):1523–1532. https://doi.org/10.1001/jama.289.12.1523
Wirth KE, Tchetgen Tchetgen EJ (2014) Accounting for selection bias in association studies with complex survey data. Epidemiology 25(3):444–453. https://doi.org/10.1097/ede.0000000000000037
Rivadeneira F, Zillikens MC, De Laet CE, Hofman A, Uitterlinden AG, Beck TJ, Pols HA (2007) Femoral neck BMD is a strong predictor of hip fracture susceptibility in elderly men and women because it detects cortical bone instability: the Rotterdam study. J Bone Miner Res 22(11):1781–1790. https://doi.org/10.1359/jbmr.070712
Kamei T, Aoyagi K, Matsumoto T, Ishida Y, Iwata K, Kumano H, Murakami Y, Kato Y (1999) Age-related bone loss: relationship between age and regional bone mineral density. Tohoku J Exp Med 187(2):141–147
Shin M-H, Zmuda JM, Barrett-Connor E, Sheu Y, Patrick AL, Leung PC, Kwok A, Kweon S-S, Nam H-S, Cauley JA, for the Osteoporotic Fractures in Men research G (2014) Race/ethnic differences in associations between bone mineral density and fracture history in older men. Osteoporos Int 25 (3):837–845. doi:https://doi.org/10.1007/s00198-013-2503-6
Drake MT, Clarke BL, Khosla S (2008) Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clinic proceedings Mayo Clinic 83(9):1032–1045
Wysowski DK (2009) Reports of esophageal cancer with oral bisphosphonate use. N Engl J Med 360(1):89–90. https://doi.org/10.1056/NEJMc0808738
Schilcher J, Michaelsson K, Aspenberg P (2011) Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med 364(18):1728–1737. https://doi.org/10.1056/NEJMoa1010650
Rosen CJ (2005) Clinical practice. Postmenopausal osteoporosis. N Engl J Med 353(6):595–603. https://doi.org/10.1056/NEJMcp043801
Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster JY, Borgstrom F, Rizzoli R (2008) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 19(4):399–428. https://doi.org/10.1007/s00198-008-0560-z
Rudman D, Drinka PJ, Wilson CR, Mattson DE, Scherman F, Cuisinier MC, Schultz S (1994) Relations of endogenous anabolic hormones and physical activity to bone mineral density and lean body mass in elderly men. Clin Endocrinol 40(5):653–661
Acknowledgments
Research reported in this publication was supported by the Knowledge Fund of the University of Nevada, Las Vegas, from the Nevada Governor’s Office, and the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R15MD010475. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Nevada Governor’s Office and the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Xu, Y., Wu, Q. Decreasing trend of bone mineral density in US multiethnic population: analysis of continuous NHANES 2005–2014. Osteoporos Int 29, 2437–2446 (2018). https://doi.org/10.1007/s00198-018-4648-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4648-9