Abstract
Introduction
While osteoporosis is common among women of Chinese descent, a readily available bone mineral density (BMD) referent database for Chinese American women does not exist. Fracture risk among this population is currently assessed using a Caucasian reference as well as diagnostic criteria for osteoporosis developed for postmenopausal Caucasian women. Many studies indicate that there are important racial differences in skeletal health and fracture risk, an observation that makes the application of Caucasian data to all groups problematical. This study was undertaken to establish a BMD referent database in Chinese American women and to compare it with a Caucasian female database. It is expected that a race-specific database will be useful in the assessment of bone health for Chinese American women.
Methods
Healthy Chinese American women (n=359), ages 20–90, were recruited. Along with dual-energy X-ray absorptiometry (DXA) of the total hip and lumbar spine, demographic, medical, familial, nutritional, and behavioral data were obtained. The mean and standard deviation for BMD at each site was calculated for each 10-year age group and compared to mean BMD values for Caucasian women supplied as found in the Hologic DXA instrument. Osteoporosis diagnosis rates for this cohort, calculated with the Caucasian and newly established Chinese American BMD referent values, were compared with each other.
Results
Compared with Caucasian women, Chinese American women have significantly lower BMD at the lumbar spine, total hip, and femoral neck across a wide spectrum of age groups. As a consequence, more than one-half of Chinese American women ≥50 years of age, who would be characterized as osteoporotic using a Caucasian referent, would not be diagnosed as such if a Chinese American referent were utilized.
Conclusion
Chinese American reference BMD values are significantly lower than those for Caucasian women. Future studies relating Chinese American BMD values to fracture risk are necessary in order to determine if ethnic database-derived T-scores would be more predictive of fracture risk and to develop meaningful diagnostic criteria for this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is characterized by compromised bone strength predisposing to an increased risk of fracture [1]. Bone mineral density (BMD), measured by bone densitometry, can establish the diagnosis of osteoporosis before the first fracture has occurred. BMD, a key determinant of bone strength, predicts fracture risk in a powerful manner. In the Caucasian postmenopausal population, for every standard deviation (SD) reduction in BMD, fracture risk is approximately doubled [2]. It is this relationship along with life-time fracture risk data among postmenopausal Caucasian women that led the World Health Organization (WHO) to define the criterion for osteoporosis as a BMD≥2.5 SD below the young normal mean for Caucasian women. Although osteoporosis is common among postmenopausal Caucasian women, it is not infrequent among non-Caucasian races, particularly Chinese women [3–6]. Recent studies suggest that as many as 88 million Chinese individuals in China may have osteoporosis [7]. Chinese Americans are also a growing population at risk for osteoporosis. The US Census Bureau estimates that by the year 2050, one-tenth of the US population will be of Asian descent, many of them, Chinese American [8, 9]. Osteoporosis is clearly an important public health problem among Chinese women living in the US, yet a relevant BMD referent database as well as diagnostic and treatment guidelines, based upon epidemiologic data for this population, are lacking.
Although the WHO densitometric definition of osteoporosis only strictly pertains to postmenopausal Caucasian women, it has been assumed by clinicians, due to lack of adequate prospective data, that the quantitative relationship between bone density and fracture risk, so well established for the group studied [2], can also be applied to non-Caucasian populations and to men. Thus, the densitometric definition of osteoporosis and treatment guidelines designed for Caucasians have been utilized for non-Caucasian races and for men without direct evidence [10–13]. Based upon data that are currently available, it is becoming increasingly apparent that there are clear racial differences in assigning fracture risk to a given BMD measurement.
For example, a number of studies have shown consistently that Chinese women have lower areal BMD (in grams per square centimeter) than Caucasian women [14–16]. Prospective studies in Asia and the United States suggest that, despite a lower bone density, Asian women actually have a significantly lower rate of hip fracture than Caucasian women [17–19], while vertebral fracture rate is only slightly lower [20]. This observation implies that the quantitative relationship between BMD and fracture risk may differ for Caucasian and Chinese women. This possibility is supported by data from the National Osteoporosis and Risk Assessment (NORA) study, a large epidemiological survey of postmenopausal women in the United States. In the NORA study, relative risk of fracture per standard deviation decrease in bone density (RR/SD) as measured by ultrasound was compared among multiple US ethnic groups, using the Caucasian female referent database [13]. While the RR/SD for fracture was similar among US Caucasians, Hispanics, and Native-Americans, it was distinctly lower for Asian Americans and African Americans. These findings make the application of the WHO diagnostic and treatment guidelines to Chinese Americans problematical. At the present time it is not clear what T-score value should be used to describe the Chinese American population at significant risk for fracture. These findings also underscore the need for further prospective studies to elucidate the BMD/fracture risk relationship in different ethnic populations so that applicable diagnostic and treatment guidelines for non-Caucasian races may be established.
Because of the lack of data relating BMD to fracture risk for many ethnicities, there is also confusion about which referent database to use for different races [10]. Some investigators advocate a single Caucasian referent standard to which all racial groups and even both sexes should be related [21]. Others argue that because of inherent differences in skeletal qualities among races and the sexes, separate referent databases should be established with which race- and sex-specific risk can be determined. While BMD referent databases have been created for African Americans and Hispanic Americans, no such database exists for Asian Americans or any Asian American subgroup. Local BMD reference databases have been created for Asian populations living in Asia [14–16, 22]. However, just as fracture risk assessment in Asian Americans using a Caucasian database is problematical, the evaluation of Asian Americans using a native Asian database is equally challenging; environmental factors and acculturation are likely to cause differences in BMD and fracture risk, even in individuals of the same or similar genetic backgrounds [23]. While it is not yet clear whether an ethnic database derived T-score would be more predictive of fracture risk for a Chinese American individual nor what T-score would define the population at significant risk, the creation of a Chinese American BMD referent database represents the first step toward further delineating this information. The aim of this study was to establish a BMD referent database in healthy, Chinese American women and to compare it with the Caucasian female database in order to examine BMD differences.
Materials and methods
Database subjects
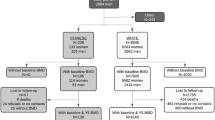
All patients gave written, informed consent. This study was approved by the Institutional Review Boards of Columbia University Medical Center and New York Downtown Hospital. Subjects were recruited from New York City’s Chinatown through physician referrals, by fliers, and at community centers, health fairs, churches, and schools. Women were screened for conditions or medications known to affect bone metabolism. A total of 359 healthy Chinese American women were enrolled from November 2002 to November 2004. Inclusion criteria were full Chinese descent (all four grandparents Chinese), female sex, age 20–90 years, and current residence in the United States. We included women born both in the United States and abroad. Exclusion criteria were bilateral hip replacement, ankylosing spondylitis, low trauma fracture, primary hyperparathyroidism, hyperthyroidism, hyperprolactinemia, current pregnancy, bilateral oophorectomy, amenorrhea ≥6 months before age 40 except during pregnancy or lactation, kidney or liver disease, organ transplantation, Paget disease, residence in a nursing home, malabsorption, a history of cancer, current or past glucocorticoid usage ≥6 months, current use of estrogen replacement, history of immunosuppressant, anti-epileptic, bisphosphonate, SERM, and calcitonin or teriparatide usage. Oral (combination estrogen/progesterone) contraceptive use was not an exclusion criterion as it does not appear to significantly affect bone mineral density among normally menstruating premenopausal women [24].
Questionnaire
All participants were interviewed by a research assistant fluent in three Chinese dialects that encompassed the entire language set of the study population. We requested information regarding birth country, age of emigration, calcium intake, lactose intolerance, physical activity, gynecologic and reproductive history, attitudes toward hormone replacement and osteoporosis treatment, falls during the previous year, difficulty with activities of daily living, fracture history, living environment, sun exposure, vision, tobacco and alcohol use, medical problems, and surgical as well as medication history.
The amount of dietary calcium was assessed by an investigator-developed food frequency questionnaire (FFQ) modified after Pun’s 24-item FFQ for calcium assessment in Hong Kong Chinese [25]. Because neither a calcium-specific FFQ developed for native Chinese populations or those developed for the general US population is directly applicable to the hybrid Chinese American diet, we added seven additional items to the original FFQ of Pun. Pilot testing of this FFQ among a sampled subset of Chinese American women revealed a good 1-month reproducibility [Spearman rank correlation coefficient (r s) = 0.72, intraclass correlation coefficient (ICC)=0.71]. There was also good agreement between the FFQ and a food diary (ICC=0.66).
Physical activity was evaluated using Paffenbarger’s physical activity questionnaire that quantifies the number of kilocalories expended per week in sports, leisure, and recreational activities [26, 27].
Physical examination
Weight and height were measured by a balance beam and a wall-mounted, calibrated Harpenden stadiometer, respectively.
Bone densitometry
Bone density was measured at the lumbar spine (L1–L4) and total hip using dual energy x-ray absorptiometry (QDR 4500C, Hologic, Waltham, Mass.). Scans were performed at the New York Downtown Family Care Center by two experienced technicians certified by the International Society for Clinical Densitometry. Each participant was measured on the same densitometer utilizing the same software and scan speed. The instrument was calibrated with reference spine and hip phantoms with anatomically correct contours (Hologic) to read BMD to within 1%. The reference phantoms (Hologic) are re-scanned at 6-month intervals. Additional quality control procedures include daily scanning of a Hologic phantom. In vivo precision, determined according to a standard method [28], at this facility is 1.28% at the lumbar spine and 1.36% at the hip. Our reproducibility using a spine phantom is 0.51%. Scans were reviewed for technical artifacts. Lumbar spine vertebral images were inspected visually for focal structural abnormalities such as degenerative changes, sclerosis, fracture, surgery, overlying metal, or calcium pills. All such vertebrae were excluded. Vertebrae for which the elevated bone mineral densities were artifactual (T-score >1 SD from other vertebrae) were excluded.
Statistical analysis
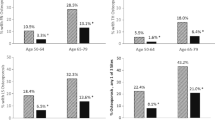
SAS statistical software (SAS, Cary, N.C.) was used for the analysis. Demographic, dietary, gynecologic, reproductive, medical, and lifestyle factors for the cohort were described using summary statistics. Age-related BMD changes at various sites among the Chinese American population were examined by plotting age versus BMD (in grams per square centimeter). Various polynomial regression models, including linear, logarithmic, quadratic, cubic, and power models, were fit to the data and compared using Aikaike’s Information Criterion (AIC) [29]. The simplest model which significantly improved the fit to the data was selected, according to Hologic’s protocol for establishing local reference databases [30]. Subjects were then stratified by age according to decade. The mean and SD for BMD at the lumbar spine (LS), total hip (TH), femoral neck (FN), trochanter, intertrochanter, and Ward’s triangle were calculated for each 10-year age group. Scans with BMD values >2 SD from the decade’s mean were evaluated for technical difficulty. Scans with BMD values >3 SD from the decade’s mean were excluded from the database. Peak adult bone mass was defined as the mean BMD of the age group with the highest mean BMD value [30]. Mean BMD for each decade at all sites was compared to mean values for Caucasian women provided in the Caucasian databases supplied by the manufacturer of the densitometer using Student’s t-test. T-scores were calculated using Caucasian BMD means and standard deviations as well as our newly established Chinese American cohort’s BMD means and standard deviations with the following equation: T-score=(BMDsubject−Peak BMD)/SDpeak. A T-score of ≤−2.5 was used as the cutoff value in the diagnosis of osteoporosis; a T-score between −1 and −2.5 was diagnostic of low bone mass (osteopenia); a T-score ≥−1 was considered normal. (We acknowledge that the WHO guidelines may not be applicable to this population, but they remain the most widely accepted and useful diagnostic guidelines available). Osteoporosis diagnosis rates, calculated with the Chinese American and Caucasian referent values, were compared using Fisher’s Exact test.
Results
The database was compiled from BMD values of 359 Chinese American women varying in age from 20 to 90 years. Baseline characteristics of this cohort are shown in Table 1. On average, BMI was normal (23.1±0.2) [mean ± standard error of the mean (SEM)], but ranged from 17 to 39. In general, this cohort engaged in bone healthy behaviors. Only 3.9% of participants were current smokers, and the mean number of pack-years among smokers was low (1.5±1.1). Thirty-four percent of subjects drank alcohol, but weekly intake was minimal (4.9±0.9 gm/week). Seventy-five percent stated that they participated in weekly exercise, and mean exercise energy expenditure (including walking) was high (1753±79 kcal/week). Daily dietary calcium intake was 612±17 mg. A maternal history of osteoporosis was present in 5.6% of patients, while 59.9% reported no maternal history of osteoporosis, and 34.5% did not know their family history. A maternal history of hip fracture was present in 6.7% of patients; there was no maternal history of hip fracture in 55.7%, while the family history was unknown in 37.6%. Birth country for participants in this cohort is shown in Fig. 1. Only 5.6% were born in the United States. Of those born abroad, the majority were born in mainland China (60.7%), followed in frequency by Hong Kong (17.3%) and Malaysia (7%). The preponderance of subjects from mainland China emigrated from Southeast China. Mean age of emigration was 29.7±0.9 years, and mean duration of residence in the United States was 14.9±0.6 years.
Figure 2 depicts age-related changes in BMD and regression curves at various skeletal sites for the Chinese American cohort. Table 2 displays the polynomial regression equations that describe the relationship between age and BMD at each site. The cubic regression model was the simplest model that significantly improved the fit to the data at every site except the femoral neck, where the quadratic model fit this criterion. The fitting effect (R2) of the regression models at each site is also shown in Table 2. Table 3 and Fig. 3 indicate the mean BMD values for each 10-year age group at various skeletal sites and the comparison with Caucasian women. At the lumbar spine (LS), BMD among Chinese American women remains stable between ages 20–49 and declines thereafter. Similar findings are apparent at the TH and other hip sites. Though there is no statistically significant difference in the BMD values for Chinese American women ages 20–29, 30–39, and 40–49 years, peak BMD is identified from the age interval with the highest BMD mean for purposes of calculating T-scores [30]. Defined in this way, peak bone density for Chinese American women occurs at age 20–29 years for the FN and at 40–49 years for the LS and TH.
Compared to Caucasian women, BMD among Chinese American women is 3.3–8.9% lower at the LS for the decades beginning at ages 30, 50, and 60 years. The LS BMD differences between Chinese American and Caucasian women at the other age groups (20–29, 40–49, 70–79, 80–89 years) are not statistically significant. Compared to Caucasian women, BMD is 4.3–8.5% lower at the TH for the decades beginning at ages 20, 30, 50 and 60 years, but not at those beginning at ages 40, 70 or 80 years. BMD values for the FN are 5.3–6.1% lower in Chinese American women for the age groups 20–29 and 30–39 years, respectively, compared to Caucasian women. Compared to Caucasian women, BMD values for the trochanter (at age 30–39 years) and intertrochanter (at age 50–59 years) were 6.0 and 6.1% lower, respectively, in Chinese American women. BMD differences for the other age groups were not statistically significant at these sites. There were no significant differences in BMD at Ward’s triangle.
Table 4 shows the comparison of peak BMD values at the LS, TH, and FN between the Chinese American cohort and the Caucasian database. The peak BMD for the sites compared is 3.3–6.1% higher in Caucasian women than in the Chinese American cohort, but these differences are only significant at the FN. When the Caucasian peak BMD and SD values are used to calculate T-scores for Chinese American women in this cohort, 1.9–2.9-fold as many women are diagnosed with osteoporosis at each site than if the newly derived Chinese American peak BMD and SD values are used (Table 5). Among women aged ≥50 years, 43% are characterized as osteoporotic at one or more sites (LS, TH or FN) if the Caucasian reference is used, whereas only 21% are categorized as osteoporotic if the Chinese American reference is used as the comparator.
Discussion
Compared with Caucasian women, Chinese American women have significantly lower BMD at the LS, TH and FN across a spectrum of age groups. In addition, peak bone mass is lower among Chinese American women. As a consequence, more than one-half of Chinese American women ≥age 50 years, characterized as osteoporotic using a Caucasian referent, would not be diagnosed as such if a Chinese American referent were utilized. Although not formally evaluated, given the cross-sectional nature of our data, our findings may also suggest that there are differences in the rate of bone mass accrual and loss between these populations. Among our Chinese American cohort, peak BMD occurred at ages 40–49 years for the LS and TH compared to ages 30–39 and 20–29 years at the LS and TH in the Caucasian population.
These results are similar to findings in native Chinese women. Woo et al. reported lower BMD values for Chinese women in Hong Kong at the LS, trochanter, FN and Ward’s triangle (except for ages 40–49 years) [14] as compared to Caucasian reference data. Similarly, Xioage et al. reported lower BMD at all hip sites across all ages and lower peak BMD for all hip sites for women in Changsha, China as compared to Caucasian reference data; LS values were not reported in this study. Additionally, the authors reported that peak BMD was achieved 10 years later at the FN and 5 years later at the TH in Chinese women than in Caucasian women, though their data too was cross-sectional [16]. Wu et al. reported lower BMD in a group of Southern Chinese women compared to Hologic Caucasian referent values at the LS, trochanter, intertrochanter and Ward’s triangle, while the BMD values were similar or higher among Chinese women at some ages for the FN, TH, and ultradistal forearm. Furthermore, peak BMD was lower for Chinese women at the LS and all hip sites. The age at which peak BMD occurred (determined using cross-sectional data) at the LS, FN, and forearm was later in Chinese women than in Caucasians, but similar at Ward’s triangle [15]. In our study, mitigation of some of the ethnic BMD differences observed in Native Chinese women may be secondary to the adoption of a Westernized diet and activity pattern among Chinese Americans.
The reasons underlying lower areal BMD among Chinese American women were not examined in this study as historical data were not available for the Caucasian reference population. However, we feel a comparison of BMD between these populations is justifiable given that the Caucasian values are used as a referent to calculate T-scores within densitometers. Lower areal BMD among Chinese Americans may in part be explained by true density differences secondary to both genetic and environmental factors. However, areal BMD differences are also likely to be secondary to a lower body weight or smaller bone size [31–34] among Chinese American women compared to Caucasians. While the effect of weight on bone density may reflect a true “weight bearing” biologic consequence [31], smaller bone size creates an artifact of lower bone density when BMD is measured by DXA, a two-dimensional technology. When areal BMD is corrected for bone size, some race-specific differences are reduced [35] or eliminated [32]. It remains unclear whether true volumetric BMD (in grams per cubic centimeter) is lower among Chinese American women than among Caucasian women, as this has not been directly measured and compared by quantitative computed tomography (QCT) in these populations.
While some may propose that lower BMD among Chinese women is irrelevant if eliminated by bone size correction, Cundy et al., among others, have deftly suggested that bone density measured by absorptiometry incorporates information that is relevant both to true density and bone size. Bone size itself may be an important component of fracture risk assessment using DXA because bone size contributes to fracture risk [31, 36, 37]. Thus, the ‘artifact’ of bone size incorporated into the bone density measurement by DXA takes into account the greater strength of a bone that has greater cross-sectional area. Theoretically, a lower BMD among Chinese women, as measured by DXA, should still predict a higher fracture risk, even if this is due, in part, to bone size; BMD as measured by DXA remains a powerful predictor of fracture within the postmenopausal Caucasian population, despite huge variations in BMI and bone size. While the “bone size artifact” may in part account for lower areal BMD among Chinese women, it does not adequately explain the lower hip fracture rates, given smaller bone size, compared to Caucasian women. Alternative explanations include shorter hip axis length (HAL) [38, 39], fewer falls [40], shorter height [41], lower bone turnover [42], or more favorable aspects of bone quality (such as volumetric density measured by QCT, microarchitecure, mineralization density, matrix components) that have yet to be compared between these races. Many of these factors, including bone size or other aspects of bone quality, may in some way alter the relationship between BMD, as measured by DXA, and fracture risk among Chinese American women; they need to be examined in more detail along with the BMD/fracture risk relationship in the Chinese American population.
In conclusion, this study demonstrates significant racial differences in bone mass between Caucasian and Chinese American women. The clinical significance of the observed BMD differences is not clear. While the use of the Caucasian versus the Chinese American database might lead to different T-score designations and therapeutic decisions for a given Chinese American individual, neither score is currently linked to relevant fracture risk data for this population. These findings highlight the need to establish a quantitative relationship between BMD and fracture risk in this growing population, so that pertinent diagnostic and treatment guidelines can ultimately be established. In future studies, our database may be employed to help establish a quantitative BMD/fracture risk relationship among Chinese American women.
It is important to note that our study population may not reflect a truly random selection of Chinese Americans. Nevertheless, this data set is likely to provide a valid BMD referent standard. We acknowledge that the WHO diagnostic thresholds applied to this population may not be directly applicable. They were, however, utilized to demonstrate that osteoporosis diagnosis rates vary if a Chinese American referent, rather than a Caucasian database, is used; further, they represent the most useful diagnostic guidelines available. Observations regarding the rate of bone mass accrual and decline need to be examined by longitudinal studies. Despite these limitations, we believe the results of the study establish the first useful BMD referent database with direct relevance to the Chinese American population.
References
NIH Consensus Development Panel on Osteoporosis (2001) Osteoporosis prevention, diagnosis and therapy. JAMA 285:785–795
Cummings SR, Nevitt, MC, Browner, WS, Stone, K, Fox, KM, Ensrud, KE, Cauley, J, Black, D, Vogt, TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:767–773
Forsen L, Sogaard AJ, Meyer HE, Edna T, Kopjar B (1999) Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int 10:73–78
Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gilbert M, Morrison RS, McLaughlin MA, Orosz GM, Siu AL (2001) Mortality and locomotion 6 months after hospitalization for hip fracture: risk factors and risk-adjusted hospital outcomes. JAMA 285:2736–2742
Katelaris AG, Cumming RG (1996) Health status before and mortality after hip fracture. Am J Public Health 86:557–560
Riggs BL, Melton LJ 3rd (1995) The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone 17:505S–511S
Liu Z, Piao J, Pang L, Qing X, Nan S, Pan Z, Guo Y, Wang X, Li F, Liu J, Cheng X (2002) The diagnostic criteria for primary osteoporosis and the incidence of osteoporosis in China. J Bone Miner Metab 20:181–189
Barnes J, Bennett CE (2002) The Asian population:2000. United States Census 2000 Brief
Day JC (2001) National Population Projections. In: US Census Bureau. http://www.census.gov/population//www/pop-profile/natproj.html
Binkley NC, Schmeer P, Wasnich RD, Lenchik L (2002) What are the criteria by which a densitometric diagnosis of osteoporosis can be made in males and non-Caucasians? J Clin Densitom 5[Suppl]S19–S27
Cummings SR, Bates D, Black DM (2002) Clinical use of bone densitometry: scientific review. JAMA 288:1889–1897
Melton LJ 3rd (2001) The prevalence of osteoporosis: gender and racial comparison. Calcif Tissue Int 69:179–181
Miller PD (2003) Bone mineral density-clinical use and application. Endocrinol Metab Clin N Am 32:159–179, vii
Woo J, Li M, Lau E (2001) Population bone mineral density measurements for Chinese women and men in Hong Kong. Osteoporos Int 12:289–295
Wu XP, Liao EY, Huang G, Dai RC, Zhang H (2003) A comparison study of the reference curves of bone mineral density at different skeletal sites in native Chinese, Japanese, and American Caucasian women. Calcif Tissue Int 73:122–132
Xiaoge D, Eryuan L, Xianping W, Zhiguang Z, Gan H, Zaijing J, Xiaoli P, Hongzhuan T, Hanwen W (2000) Bone mineral density differences at the femoral neck and Ward’s triangle: a comparison study on the reference data between Chinese and Caucasian women. Calcif Tissue Int 67:195–198
Lauderdale DS, Jacobsen SJ, Furner SE, Levy PS, Brody JA, Goldberg J (1997) Hip fracture incidence among elderly Asian-American populations. Am J Epidemiol 146:502–509
Silverman SL, Madison RE (1988) Decreased incidence of hip fracture in Hispanics, Asians, and blacks: California hospital discharge data. Am J Public Health 78:1482–1483
Xu L, Lu A, Zhao X, Chen X, Cummings SR (1996) Very low rates of hip fracture in Beijing, People’s Republic of China the Beijing Osteoporosis Project. Am J Epidemiol 144:901–907
Ling X, Cummings SR, Mingwei Q, Xihe Z, Xioashu C, Nevitt M, Stone K (2000) Vertebral fractures in Beijing, China: the Beijing osteoporosis project. J Bone Miner Res 15:2019–2025
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Koh SK, Cho SH, Hwang YY, Moon H, Kim DS, Cho JL, Cho SS (1992) Spinal bone mineral density of normal and osteoporotic women in Korea. J Korean Med Sci 7:136–140
Kin K, Lee JH, Kushida K, Sartoris DJ, Ohmura A, Clopton PL, Inoue T (1993) Bone density and body composition on the Pacific rim: a comparison between Japan-born and U.S.-born Japanese-American women. J Bone Miner Res 8:861–869
Berenson AB, Breitkopf CR, Grady JJ, Rickert VI, Thomas A (2004) Effects of hormonal contraception on bone mineral density after 24 months of use. Obstet Gynecol 103:899–906
Chi I, Pun KK (1991) Dietary calcium intake and other risk factors: study of the fractured patients in Hong Kong. J Nutr Elder 10:73–87
Paffenbarger RS Jr, Hyde RT, Wing AL, Hsieh CC (1986) Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med 314:605–613
Paffenbarger RS Jr, Wing AL, Hyde RT (1978) Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol 108:161–175
Bonnick SL, Johnston CC Jr, Kleerekoper M, Lindsay R, Miller P, Sherwood L, Siris E (2001) Importance of precision in bone density measurements. J Clin Densitom 4:105–110
Akaike H (1981) Likelihood of a model and information criteria. J Econom 16:3–14
Kelly T (1996) Developing DXA Reference Databases. In: Hologic, Inc. (unpublished work; available upon request form Hologic, Waltham, Mass.)
Cundy T, Cornish J, Evans MC, Gamble G, Stapleton J, Reid IR (1995) Sources of interracial variation in bone mineral density. J Bone Miner Res 10:368–373
Finkelstein JS, Lee ML, Sowers M, Ettinger B, Neer RM, Kelsey JL, Cauley JA, Huang MH, Greendale GA (2002) Ethnic variation in bone density in premenopausal and early perimenopausal women: effects of anthropometric and lifestyle factors. J Clin Endocrinol Metab 87:3057–3067
Russell-Aulet M, Wang J, Thornton JC, Colt EW, Pierson RN Jr (1993) Bone mineral density and mass in a cross-sectional study of white and Asian women. J Bone Miner Res 8:575–582
Bhudhikanok GS, Wang MC, Eckert K, Matkin C, Marcus R, Bachrach LK (1996) Differences in bone mineral in young Asian and Caucasian Americans may reflect differences in bone size. J Bone Miner Res 11:1545–1556
Lau EM, Lynn H, Woo J, Melton LJ 3rd (2003) Areal and volumetric bone density in Hong Kong Chinese: a comparison with Caucasians living in the United States. Osteoporos Int 14:583–588
Seeman E (2001) Clinical review 137: sexual dimorphism in skeletal size, density, and strength. J Clin Endocrinol Metab 86:4576–4584
Turner CH, Burr DB (1993) Basic biomechanical measurements of bone: a tutorial. Bone 14:595–608
Cummings SR, Cauley JA, Palermo L, Ross PD, Wasnich RD, Black D, Faulkner KG (1994) Racial differences in hip axis lengths might explain racial differences in rates of hip fracture. Study of Osteoporotic Fractures Research Group. Osteoporos Int 4:226–229
Faulkner KG, Cummings SR, Black D, Palermo L, Gluer CC, Genant HK (1993) Simple measurement of femoral geometry predicts hip fracture: the study of osteoporotic fractures. J Bone Miner Res 8:1211–1217
Davis JW, Nevitt MC, Wasnich RD, Ross PD (1999) A cross-cultural comparison of neuromuscular performance, functional status, and falls between Japanese and white women. J Gerontol A Biol Sci Med Sci 54:M288–M292
Lau EM, Suriwongpaisal P, Lee JK, Das De S, Festin MR, Saw SM, Khir A, Torralba T, Sham A, Sambrook P (2001) Risk factors for hip fracture in Asian men and women: the Asian osteoporosis study. J Bone Miner Res 16:572–580
Finkelstein JS, Sowers M, Greendale GA, Lee ML, Neer RM, Cauley JA, Ettinger B (2002) Ethnic variation in bone turnover in pre- and early perimenopausal women: effects of anthropometric and lifestyle factors. J Clin Endocrinol Metab 87:3051–3056
Acknowledgements
This investigation was supported in part by: NIDDK T32 DK07271, the Endocrine Fellows Foundation, the Merck Medical School Grant Progam, Procter & Gamble Pharmaceuticals, and the Chinese American Medical Society-Chinese American Independent Physicians Association (CAMS-CAIPA) Community Service Fund
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donovan Walker, M., Babbar, R., Opotowsky, A.R. et al. A referent bone mineral density database for Chinese American women. Osteoporos Int 17, 878–887 (2006). https://doi.org/10.1007/s00198-005-0059-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-0059-9