Abstract
Summary
Falling and fractures are a public health problem in elderly people. The aim of our study was to investigate whether nutritional status is associated with the risk of falling or fracture in community-dwelling elderly. Poor nutritional status was significantly associated with a higher risk of both falling and fractures.
Introduction
Nutrition could play a role to prevent falls and fractures. The purpose of this study is to investigate whether a poor nutritional status is associated with the risk of falling and of fracture in community dwelling elderly.
Methods
Baseline nutritional status of participants was assessed using the Mini Nutritional Assessment (MNA). After a follow-up of 12 years, 6040 individuals with available data for falls and 6839 for fracture were included. People who presented the outcomes at baseline were excluded. Cox models were used to evaluate the associations between nutritional status and the risks of fall or fracture.
Results
The frequency of poor nutritional status (MNA ≤ 23.5), at baseline, was respectively 12.0 % in the “fall study sample” and 12.8 % in the “fracture study sample.” Incident fall and fracture over 12 years were reported in 55.8 and 18.5 % of the respective samples, respectively. In multivariate models controlled for sociodemographic data and several baseline health indicators, poor nutritional status was significantly associated with a higher risk of falling (hazard ratio (HR) = 1.66, 95 % confidence interval (95 % CI) 1.35–2.04 in men and HR = 1.20, 95 % CI 1.07–1.34 in women) and with a higher risk of fracture (HR = 1.28, 95 % CI 1.09–1.49).
Conclusion
Poor nutritional status was associated with a higher risk of both falling and fractures in French elderly community-dwellers. Early screening and management of the nutritional status may be useful to reduce the frequency of these events in older people.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Falling and fractures are an important public health challenge for elderly population whose proportion is growing worldwide. In older population, falling and fractures are important determinants of functional decline and disability [1, 2], increase the mortality rate, and lead to dramatic medical costs to society [3]. It is estimated that about 30 % of elderly people living at home fall at least once each year [4, 5]. The risk and severity of injuries after a fall are important, and falling appears to be a key determinant of fracture risk [6]. In elderly people, some body sites of fractures, such as the hip, the wrist, or the spine, are a clinical manifestation of osteoporosis [7]. Other bones common to fracture in older people are the arms or legs. The prevention of falling could decrease the occurrence of fractures. Among modifiable risk factors for falls and fractures, malnutrition could play a role through its impact on muscle and bone health [8]. Adequate protein intake is recommended for optimal muscle function with aging and to maintain strength and physical endurance [9], while the role of protein intake on bone health is more controversial [10]. A low protein intake has been associated with a decrease of bone mineral density [11] and with higher risk of bone fractures in women [12]. Among other nutrients, adequate calcium and vitamin D intake have been consistently associated with preserved bone health [13, 14]. We have previously shown that a nutrient pattern with higher intakes of calcium, phosphorus, vitamins B12, proteins, unsaturated fats, and moderate alcohol was associated with a lower risk of fracture [15]. Furthermore, malnutrition has been associated with lower bone mineral density [16] that could have an effect on fracture. Taken altogether, these findings suggest that global malnutrition could be a risk factor for both falling and fracture.
Malnutrition, as evaluated by the Mini Nutritional Assessment (MNA), is present in 4 to 10 % of seniors living at home [17]. The MNA, sign of energy and multiple nutrient deficiencies and particularly of a low intake of protein, has been validated specifically in older persons to identify people with a poor nutritional status [18]. Malnutrition has been associated with poor muscle strength [19] and impaired balance [20], two conditions that could lead to falling. Saka et al. have shown that 43 % of people with a poor nutritional status experience one or more falls in the next year, which is significantly higher when compared to 31 % of people with a satisfying MNA score (p = 0.02) [21]. Other studies have shown an association between malnutrition and the risk of falling [22–26], but most of them examined subjects living in hospitals or in nursing homes and during a short follow-up. At our knowledge, no study has explored the association between the nutritional status assessed by the MNA and the occurrence of fracture. The aim of this study was to determine whether nutritional status (evaluated by the MNA) is associated with the overall and fracture site-specific (i.e., the hip, wrist, spine, upper and lower limbs) risk of falling and fracture in community-dwelling older people.
Methods
Study population
The Three-City (3C) study is an observational cohort study of vascular risk factors for dementia; the methodology has been described elsewhere [27]. In 1999–2001, 9294 community-dwellers aged 65 years and over were randomly recruited from electoral rolls of three French cities: Bordeaux (n = 2104), Dijon (n = 4931), and Montpellier (n = 2259). The study was approved by the Ethics Committee of the Kremlin-Bicêtre Hospital. Written consent was provided by all participants. At baseline, psychologists collected sociodemographic and medical history of participants by a questionnaire. To date, five follow-up examinations were performed at about 2, 4, 7, 10, and 12 years after inclusion.
Two subsamples were analyzed. For the falling subsample, from the 7464 participants with no recent falls at baseline, we included 6040 individuals with available nutritional status information at baseline, who were followed at least once during the 12 years of follow-up, and had no missing data in the covariates. We employed the same selection criteria for the fracture subsample: from the 8560 participants with no recent fractures at baseline, 6839 subjects were included.
Outcomes
Self-reported history of falling was provided by participants at baseline and at each follow-up visit (except at the 7 years follow-up). Self-reported history of fractures and information about the body sites of the fractures (the hip, wrist, spine, upper limb (arm, shoulder, collarbone, excluding wrist), lower limb (excluding hip), and other site) were collected at baseline and at each follow-up visit. The two main outcomes of interest in this analysis were the occurrences of a first fall and of a first fracture. In secondary analyses, we studied fractures for each site separately.
Nutritional status assessment
MNA is a questionnaire identifying elderly people who are at risk of malnutrition or malnourished [18]. It is composed of 18 items grouped into four parts (anthropometric measurements, a global assessment, a dietary questionnaire, and a self-assessment) and provides a total score on 30 points. A score superior to 23.5 indicates a good nutritional status, inferior or equal to 23.5 a risk of malnutrition, and inferior to 17 indicates malnutrition. In the present study, the MNA was not strictly administered but similar questions from the baseline survey allowed us to build an equivalent from proxy items. This form has shown a good agreement with the standard form in a previous study [28]. In 3C, the proportion of malnourished individuals was only small; therefore, these malnourished were grouped with those at risk of malnutrition representing people in a “poor nutritional status” opposed to a “good nutritional status.”
Other variables
Whatever the outcome studied, i.e., risk of falling or risk of fracture, a set of common adjustment variables, including gender; study center (Bordeaux, Dijon, or Montpellier); marital status (married, widowed, or other); education level (defined as high for subjects with at least a high school diploma vs the others); smoking status (never smoker, former smoker, or current smoker); cognitive function evaluated by the Mini Mental State Examination (MMSE) [29]; using more than five drugs, hypertension (defined as having systolic blood pressure >160 mmHg or diastolic blood pressure >95 mmHg or use of antihypertensive drugs); and the presence of dyspnea, arteritis, and heart failure were considered. Regarding the risk of fracture, treatments for osteoporosis (bisphosphonates, raloxifene, strontium ranelate, teriparatide, and calcitonin) and supplementation with calcium and/or vitamin D were considered in addition to the abovementioned common covariates.
Statistical analyses
A description of sociodemographic and medical information was performed in the two subsamples according to their nutritional status. The χ 2 test and Student’s t test were used to determine bivariate differences. Cox proportional hazard regression models with delayed entry and taking age as the time scale were performed to estimate the associations between poor nutritional status and the risks of incident fall and the overall and site-specific fractures. We secondarily tested effect modification by gender, by including a malnutrition-by-gender interaction term in our model. Statistical analyses were conducted using SAS statistical package release 9.3 (SAS Institute Inc., Cary, NC).
Results
Subjects characteristics
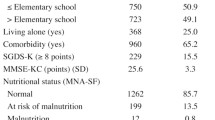
Table 1 presents the characteristics of the sample included in the “falling subsample.” These subjects were 73.5 years old on average and 58.2 % were female. At baseline, 12.0 % were in poor nutritional status according to the MNA, with a twofold higher prevalence in women compared to men (15.5 vs 7.1 %, respectively). During a maximum follow-up of 12 years (mean 7.8 years), 3369 subjects (55.8 %) reported at least one incident fall. The incidence rates was 14.3/100 person years (PY) (95 % confidence interval (95 % CI) 13.8–14.9) among women and 8.8/100 PY (95 % CI 8.3–9.3) among men. People who reported a fall during the follow-up were significantly older, more often female, widowed, never smoker, user more than five drugs, and had more often history of heart failure compared with those without experience of falls.
Table 2 presents the characteristics of the sample included in the “fracture subsample.” These subjects were 73.7 years old on average and 59.8 % were female. At baseline, 12.8 % had a poor nutritional status according to the proxy MNA. Over 12 years, 1264 subjects (18.5 %) had at least one incident fracture at any site. Among this sample, 2.3 % had a hip fracture, 1.8 % a spinal fracture, 4.6 % a wrist fracture, 4.6 % a lower limb fracture, 3.6 % an upper limb fracture, and 5.5 % a fracture at other body sites as first fracture. The incidence rate for fracture at any site was 2.6/100 PY (95 % CI 2.5–2.7), without significant differences between men and women. People with an incident fracture were significantly older, more often female, widowed, and never smokers. They also reported more often supplementation with vitamin D and/or calcium and medication for osteoporosis than those without experience of fracture.
Poor nutritional status and risk of falling
The results of the Cox proportional hazards model analyses of the association between nutritional status and the incidence of falling are presented in Table 3. As the interaction between nutritional status and gender was statistically significant (p < 0.01), we presented results stratified by gender. A poor nutritional status was significantly associated with an increased risk of falling in both genders. Indeed, the association appeared stronger in males (hazard ratio (HR) = 1.67; 95 % CI = 1.36–2.05) than in females (HR = 1.21, 95 % CI = 1.08–1.36).
Poor nutritional status and risk of fracture
A poor nutritional status was significantly associated with a higher risk of fracture at any site (Table 4) after controlling for potential confounders (HR = 1.28, 95 % CI 1.09–1.49). There was no significant interaction between the nutritional status and gender. The analysis by site-specific fractures did not show significant association. Also, lower and upper limbs were close to significance.
Discussion
In this large population-based cohort of elderly individuals followed for up to 12 years, a baseline poor nutritional status, assessed by the proxy MNA, was significantly associated with an increased risk of falling, especially in males. Poor nutritional status was also significantly associated in both genders with a higher risk of fracture. These associations were independent of major potential confounders.
Our results are in accordance with different population-based studies using MNA to assess risk of malnutrition. First, Chien et al. examined the association between the baseline nutritional status and the incidence of falls between the third and the fourth year after baseline [22] among 4440 community-dwelling Taiwanese aged 53 years and older. A poor nutritional status was associated with a higher risk of falling (odds ratio (OR) = 1.73; 95 % CI 1.23–2.42) in particular among men. Second, as reported by Visvanathan et al., elderly people receiving domiciliary care services in Australia and identified in poor nutritional status were more likely to fall (HR = 1.65; 95 % CI 1.13–2.41) over a 12-month period [30]. However, in an Australian study on a sample of 254 subjects with only 10 defined at risk of malnutrition, there were no association with the risk of falls over a 1-year period [31].
Other studies have investigated the association between nutritional status and the risk of falling in different populations, i.e., in frail elderly people [23], in elderly receiving home care [24], in residential long-term care [25], and during a hospital admission [26], and generally found consistent associations between poor nutritional status and higher prevalence of falls. Yet, these studies were mainly cross-sectional and did not observed incident falling. Thus, no causal link between nutritional status and falls could be derived from these studies, where malnutrition could be a consequence of falling in these elderly people due to for example inability to go out for shopping and prepare adequate meals. Our study adds to this literature showing a prospective relation between nutritional status and the occurrence of fall, an association which support different hypotheses.
With aging, muscle mass and muscle strength decrease, a phenomenon also known as sarcopenia [32] with multiple related factors such as inadequate nutritional intake, imbalance protein metabolism, and malnutrition [33, 34]. The risk of falling associated with malnutrition could be related to muscle weakness and deficiencies in the coordination of movement as well as protective mechanisms such as reaction time and muscle strength [35]. In our study, unexpectedly, the relation between malnutrition and a greater risk of falling was stronger in men than in women; we could hypothesize that the hormone secretion plays a role on the muscle metabolism involving a difference according to the gender.
To our knowledge, no published study has investigated the association between nutritional status and the risk of total fractures (i.e., fractures at any site) since most studies were restricted to hip fractures [36–38], which is the most frequent fracture in the elderly. Wilsgaard et al. showed in older non-smokers Norwegian that loss of BMI over 10 years was significantly associated with a risk of non-vertebral fracture [39]. Weight loss has been associated with a higher risk of hip fracture [36–38] and frailty fractures [40].
As the risk factors differed according to the body sites of fracture [3], we have explored the association between poor nutritional status and the risk of fracture by subtypes. However, no association was observed between poor nutritional status and the risk of fracture by sites. These analyses were performed on a limited number of events with a maximum of 300 fractures, and a lack of power is expected. Nevertheless, the risks of fracture of the hip, lower limbs, and upper limbs ranged from 1.3 to 1.4, and the last two were close to significance. Surprisingly, no study so far has been conducted to assess a potential detrimental effect of poor nutritional status evaluated by the MNA on the risk of fracture over time, which precludes comparisons with existing literature. However, our results were consistent with the other analyses from a subsample of the 3C study, reporting that a higher adherence to the Mediterranean diet [41] and a “nutrient-dense” pattern rich, among others, in calcium and protein [15] were significantly associated with a lower risk of fracture. MNA reflects multiple deficiencies, including proteins. This is a more general and easy tool to assess nutritional deficiencies in older adults compared to the dietary surveys that are more difficult to administer.
Regarding the underlying mechanisms linking malnutrition to falling and fracture, we could hypothesize that the effect of poor nutritional status on fracture relies on the loss of muscle strength [42] and that falls might mediate the relationship between malnutrition and the risk of fractures. However, it could be also due to a bone metabolism disturbance since Bischoff-Ferrari et al. have shown that a vitamin D supplementation decreased the risk of hip fracture and any non-vertebral fracture [43]. A study has found that a higher protein intake, rather than calcium or vitamin D, was a preventive factor of hip fracture in postmenopausal women [44]. Moreover, multiple intertwined biological mechanisms between the metabolisms of bone and muscle may underlie relationships between sarcopenia and frailty fractures [45]. There are many common pathogenic pathways leading to osteoporosis and sarcopenia including the decrease of anabolic hormone secretion, increase of inflammatory cytokine activity, and decreased physical activity. The decrease in muscle strength in sarcopenia leads to lower bone strength. Yu et al. has studied the association between sarcopenia and incident fracture among older men aged 65 years and over living at home [46] and found that sarcopenia was associated with an increased fracture risk.
While the strengths of our study are the large sample size of community-dwellers in relatively good health, not yet malnourished, and that were followed for more than a decade, there are also some limitations. By selecting subjects with no missing data in the covariates, we excluded individuals who were older, in poorer health, and with a higher risk of fracture. This may have resulted in possible underestimation of observed associations. In addition, the assessments of fall and fracture were self-reported and some events may have been missed. However, the frequency of falls, even if underestimated, appears high (45 % in men and 63 % in women) in this community-based sample. It is likely that only the most significant events were reported and reinforces the fact that poor nutritional status measured with MNA is associated with major clinical events.
In conclusion, this longitudinal population-based study suggests that a poor nutritional status is associated with a higher risk of falling and fractures in elderly community-dwellers. MNA could be a good indicator for the clinicians to target people at risk before malnutrition is established. Early and routinely screening of elderly people living at home and management of their nutritional status may be useful to reduce the frequency of these events. Further studies to identify the deficiencies of specific nutrients, the mechanisms involved, and the impact of nutritional intervention are needed.
References
Tinetti ME, Williams CS (1997) Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 337(18):1279–1284. doi:10.1056/NEJM199710303371806
Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J (2005) Prevention of falls and consequent injuries in elderly people. Lancet 366(9500):1885–1893. doi:10.1016/S0140-6736(05)67604-0
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767. doi:10.1016/S0140-6736(02)08657-9
Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ (2007) Will my patient fall? JAMA J Am Med Assoc 297(1):77–86. doi:10.1001/jama.297.1.77
Gill T, Taylor AW, Pengelly A (2005) A population-based survey of factors relating to the prevalence of falls in older people. Gerontology 51(5):340–345. doi:10.1159/000086372
Bischoff-Ferrari HA (2011) The role of falls in fracture prediction. Curr Osteoporos Rep 9(3):116–121. doi:10.1007/s11914-011-0059-y
Rachner TD, Khosla S, Hofbauer LC (2011) Osteoporosis: now and the future. Lancet 377(9773):1276–1287. doi:10.1016/S0140-6736(10)62349-5
Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention (2001) J Am Geriatr Soc 49(5):664–672
Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy-Westphal A, Cederholm T, Cruz-Jentoft A, Krznaric Z, Nair KS, Singer P, Teta D, Tipton K, Calder PC (2014) Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr. doi:10.1016/j.clnu.2014.04.007
IOM (Institute of Medicine) (2011) Dietary reference intakes for calcium and Vitamin D. The National Academies Press, Washington, DC
Geinoz G, Rapin CH, Rizzoli R, Kraemer R, Buchs B, Slosman D, Michel JP, Bonjour JP (1993) Relationship between bone mineral density and dietary intakes in the elderly. Osteoporos Int J Established Result Cooperation Between Eur Found Osteoporos Natl Osteoporos Found USA 3(5):242–248
Feskanich D, Willett WC, Stampfer MJ, Colditz GA (1996) Protein consumption and bone fractures in women. Am J Epidemiol 143(5):472–479
Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A (2007) Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet 370(9588):657–666. doi:10.1016/S0140-6736(07)61342-7
Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, Wong JB (2004) Effect of vitamin D on falls: a meta-analysis. JAMA J Am Med Assoc 291(16):1999–2006. doi:10.1001/jama.291.16.1999
Samieri C, Ginder Coupez V, Lorrain S, Letenneur L, Alles B, Feart C, Paineau D, Barberger-Gateau P (2013) Nutrient patterns and risk of fracture in older subjects: results from the Three-City Study. Osteoporos Int J Established Result Cooperation Between Eur Found Osteoporos Natl Osteoporos Found USA 24(4):1295–1305. doi:10.1007/s00198-012-2132-5
Ulger Z, Halil M, Kalan I, Yavuz BB, Cankurtaran M, Gungor E, Ariogul S (2010) Comprehensive assessment of malnutrition risk and related factors in a large group of community-dwelling older adults. Clin Nutr 29(4):507–511. doi:10.1016/j.clnu.2010.01.006
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, Thomas DR, Anthony PS, Charlton KE, Maggio M, Tsai AC, Vellas B, Sieber CC, Mini Nutritional Assessment International G (2010) Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc 58(9):1734–1738. doi:10.1111/j.1532-5415.2010.03016.x
Guigoz Y, Vellas B, Garry PJ (1996) Assessing the nutritional status of the elderly: the Mini Nutritional Assessment as part of the geriatric evaluation. Nutr Rev 54(1 Pt 2):S59–S65
Ahmed T, Haboubi N (2010) Assessment and management of nutrition in older people and its importance to health. Clin Interv Aging 5:207–216
Avila-Funes JA, Gray-Donald K, Payette H (2008) Association of nutritional risk and depressive symptoms with physical performance in the elderly: the Quebec longitudinal study of nutrition as a determinant of successful aging (NuAge). J Am Coll Nutr 27(4):492–498
Saka B, Kaya O, Ozturk GB, Erten N, Karan MA (2010) Malnutrition in the elderly and its relationship with other geriatric syndromes. Clin Nutr 29(6):745–748. doi:10.1016/j.clnu.2010.04.006
Chien MH, Guo HR (2014) Nutritional status and falls in community-dwelling older people: a longitudinal study of a population-based random sample. PLoS One 9(3):e91044. doi:10.1371/journal.pone.0091044
Johnson CS (2003) The association between nutritional risk and falls among frail elderly. J Nutr Health Aging 7(4):247–250
Meijers JM, Halfens RJ, Neyens JC, Luiking YC, Verlaan G, Schols JM (2012) Predicting falls in elderly receiving home care: the role of malnutrition and impaired mobility. J Nutr Health Aging 16(7):654–658
Neyens J, Halfens R, Spreeuwenberg M, Meijers J, Luiking Y, Verlaan G, Schols J (2013) Malnutrition is associated with an increased risk of falls and impaired activity in elderly patients in Dutch residential long-term care (LTC): a cross-sectional study. Arch Gerontol Geriatr 56(1):265–269. doi:10.1016/j.archger.2012.08.005
Vivanti A, Ward N, Haines T (2011) Nutritional status and associations with falls, balance, mobility and functionality during hospital admission. J Nutr Health Aging 15(5):388–391
3C Study Group (2003) Vascular factors and risk of dementia: design of the Three-City Study and baseline characteristics of the study population. Neuroepidemiology 22(6):316–325
Torres MJ, Dorigny B, Kuhn M, Berr C, Barberger-Gateau P, Letenneur L (2014) Nutritional status in community-dwelling elderly in France in urban and rural areas. PLoS ONE 9(8):e105137
Cockrell JR, Folstein MF (1988) Mini-Mental State Examination (MMSE). Psychopharmacol Bull 24(4):689–692
Visvanathan R, Macintosh C, Callary M, Penhall R, Horowitz M, Chapman I (2003) The nutritional status of 250 older Australian recipients of domiciliary care services and its association with outcomes at 12 months. J Am Geriatr Soc 51(7):1007–1011
Isenring E, Baker J, Kerr G (2013) Malnutrition and falls risk in community-dwelling older adults. J Nutr Health Aging 17(3):277–279. doi:10.1007/s12603-012-0408-2
Boirie Y (2009) Physiopathological mechanism of sarcopenia. J Nutr Health Aging 13(8):717–723
Jeejeebhoy KN (1994) How should we monitor nutritional support: structure or function? New Horiz 2(2):131–138
Kinney JM (2004) Nutritional frailty, sarcopenia and falls in the elderly. Curr Opin Clin Nutr Metab Care 7(1):15–20
Rizzoli R, Ammann P, Chevalley T, Bonjour JP (2001) Protein intake and bone disorders in the elderly. Joint Bone Spine Rev Rhum 68(5):383–392
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332(12):767–773. doi:10.1056/NEJM199503233321202
Langlois JA, Mussolino ME, Visser M, Looker AC, Harris T, Madans J (2001) Weight loss from maximum body weight among middle-aged and older white women and the risk of hip fracture: the NHANES I epidemiologic follow-up study. Osteoporos Int J Established Result Cooperation Between Eur Found Osteoporos Natl Osteoporos Found USA 12(9):763–768. doi:10.1007/s001980170053
Meyer HE, Tverdal A, Selmer R (1998) Weight variability, weight change and the incidence of hip fracture: a prospective study of 39,000 middle-aged Norwegians. Osteoporos Int J Established Result Cooperation Between Eur Found Osteoporos Natl Osteoporos Found USA 8(4):373–378. doi:10.1007/s001980050077
Wilsgaard T, Jacobsen BK, Ahmed LA, Joakimsen RM, Stormer J, Jorgensen L (2011) BMI change is associated with fracture incidence, but only in non-smokers. The Tromso Study. Osteoporos Int J Established Result Cooperation Between Eur Found Osteoporos Natl Osteoporos Found USA 22(4):1237–1245. doi:10.1007/s00198-010-1318-y
Ensrud KE, Cauley J, Lipschutz R, Cummings SR (1997) Weight change and fractures in older women. Study of Osteoporotic Fractures Research Group. Arch Intern Med 157(8):857–863
Feart C, Lorrain S, Ginder Coupez V, Samieri C, Letenneur L, Paineau D, Barberger-Gateau P (2013) Adherence to a Mediterranean diet and risk of fractures in French older persons. Osteoporos Int J Established Result Cooperation Between Eur Found Osteoporos Natl Osteoporos Found USA 24(12):3031–3041. doi:10.1007/s00198-013-2421-7
Mithal A, Bonjour JP, Boonen S, Burckhardt P, Degens H, El Hajj Fuleihan G, Josse R, Lips P, Morales Torres J, Rizzoli R, Yoshimura N, Wahl DA, Cooper C, Dawson-Hughes B, Group ICNW (2013) Impact of nutrition on muscle mass, strength, and performance in older adults. Osteoporos Int J Established Result Cooperation Between Eur Found Osteoporos Natl Osteoporos Found USA 24(5):1555–1566. doi:10.1007/s00198-012-2236-y
Bischoff-Ferrari HA, Willett WC, Orav EJ, Lips P, Meunier PJ, Lyons RA, Flicker L, Wark J, Jackson RD, Cauley JA, Meyer HE, Pfeifer M, Sanders KM, Stahelin HB, Theiler R, Dawson-Hughes B (2012) A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med 367(1):40–49. doi:10.1056/NEJMoa1109617
Munger RG, Cerhan JR, Chiu BC (1999) Prospective study of dietary protein intake and risk of hip fracture in postmenopausal women. Am J Clin Nutr 69(1):147–152
Cederholm T, Cruz-Jentoft AJ, Maggi S (2013) Sarcopenia and fragility fractures. Eur J Phys Rehabil Med 49(1):111–117
Yu R, Leung J, Woo J (2014) Incremental predictive value of sarcopenia for incident fracture in an elderly Chinese cohort: results from the Osteoporotic Fractures in Men (MrOs) Study. J Am Med Dir Assoc. doi:10.1016/j.jamda.2014.02.005
Study funding
The Three-City Study is conducted under a partnership agreement between the Institut National de la Santé et de la Recherche Médicale (INSERM), the Victor Segalen–Bordeaux II University, and Sanofi-Aventis. The Fondation pour la Recherche Médicale funded the preparation and initiation of the study. The 3C Study is also supported by the Caisse Nationale Maladie des Travailleurs Salariés, Direction Générale de la Santé, MGEN, Institut de la Longévité, Conseils Régionaux of Aquitaine and Bourgogne, Fondation de France, and Ministry of Research–INSERM Programme « Cohortes et collections de données biologiques. » This work was supported by the « Fondation Plan Alzheimer » and by grants from the « ANR—Agence Nationale de la Recherche, » The French National Research Agency « Programme National de Recherche en Alimentation et nutrition humaine, » project « COGINUT ANR-06-PNRA-005, » and the « Programme Longévité et vieillissement, » COGICARE 07-LVIE 003 01. The funding organizations played no role in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; or in preparation, review, or approval of the manuscript.
Conflicts of interest
Marion J Torres was supported by Nutricia France and participated at different meetings with Danone Research. Beatrice Dorigny and Yvette Luiking are employed by Nutricia. Pascale Barberger-Gateau reports grants and non-financial support from Danone Research and Vifor Pharma, personal fees and non-financial support from Nutricia, grants and non-financial support from Groupe Lipides et Nutrition, and non-financial support from ILSI Europe. C. Féart received fees for conferences from Danone Research and Nutricia. L. Letenneur received fees for conferences from Danone Research. Cécilia Samieri and Claudine Berr declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Torres, M.J., Féart, C., Samieri, C. et al. Poor nutritional status is associated with a higher risk of falling and fracture in elderly people living at home in France: the Three-City cohort study. Osteoporos Int 26, 2157–2164 (2015). https://doi.org/10.1007/s00198-015-3121-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3121-2