Abstract
Summary
In a cohort of 169,145 patients with a hip fracture and 524,010 controls we observed an excess mortality among patients compared to controls for as long as 20 years after the hip fracture. The main reason for the excess mortality was linked to the trauma that caused the hip fracture.
Introduction
Patients with a hip fracture have a significant excess mortality. However, it remains unclear if the mortality is linked to the pre-morbid conditions or to complications to the fracture.
Methods
All subjects with a hip fracture in Denmark between 1977 and 2001 were compared with three age- and gender-matched subjects from the general population.
Results
A total of 169,145 fracture cases were compared to 524,010 controls. The cases had a much higher prevalence of co-morbidity than the controls. The mortality rate was twice as high in fracture cases compared with controls (HR = 2.26, 95% CI: 2.24–2.27). Adjustments for confounders only changed the excess mortality risk little. The mortality after the hip fracture was divided into two categories: an excess mortality of 19% within the first year following the fracture (relative survival = 0.81 compared to controls), and an excess mortality of 1.8% per year (relative survival 0.982) for every additional year following the fracture. The major causes of the excess mortality were due to complications to the fracture event (70.8% within the first 30 days).
Conclusions
Patients with a hip fracture have a pronounced excess mortality risk. The major cause was linked to the fracture event and not to pre-existing co-morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
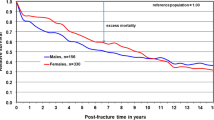
Patients suffering a hip fracture have a significant excess mortality compared with the general population [1–4]. After two years the observed survival rate was approximately 75% in women and 65% in men compared with an expected survival of approximately 85% in both genders [2]. The number of life-years lost after a hip fracture is, thus, substantial as hip fracture incidence is high in many communities [5]. If survival through a preventive programme could be modified to the level observed in the general population, only ten women or five men would need to undergo the programme for two years to prevent one excess death [2].
A number of studies have addressed excess mortality in hip fracture patients compared to controls [2–4, 6–15]. Most studies reported that the excess mortality is linked to the period of the first 6 to 12 months following the hip fracture [2, 3, 6–13], with one study describing an excess mortality for up to 5 years following the hip fracture [4], and another study reporting excess mortality for as long as 10 years after the fracture [14]. Some of the prior studies have been limited in size [6, 8, 10, 13] or duration of follow-up [3, 9, 12], thus making them less likely to detect small excess mortality risks over a prolonged period of time. Many studies also used cohorts that did not contain recent data [2–4, 9, 11, 14], i.e., operative management may have changed along with postoperative care. Furthermore, none of the studies addressed causes of death among the hip fracture cases or controls.
The causes of the excess mortality have been subject to debate. The excess mortality may be linked to complications following the fracture such as pulmonary embolism [16], infections [17, 18], and heart failure [17, 18]. However, the excess mortality may also be linked to co-morbid conditions prior to the fracture [13]. e.g., may patients with heart diseases be more likely to fall and thus sustain a fracture as a consequence of the impaired circulation, but the impaired circulation may also increase the likelihood of dying after having sustained a fracture. In the same way patients with immobilisation and osteoporosis following a stroke may have not only an increased risk of falls and fractures [19] but also an increased risk of dying following complications to the neurovascular disease. An excess mortality as in patients with hip fractures has also been observed in patients with fractures of the spine and forearm [20, 21] as well as after other types of osteoporotic fractures [22]. This could indicate that pre-existing factors associated with the risk of osteoporotic fractures may be responsible for the excess mortality. This is supported by one study finding that after adjustment for weight loss and other markers of physical disability no excess mortality was present in patients with a spine fracture [21]. Another study has shown that pre-existing heart- [23] or lung diseases were associated with an increased mortality after a hip fracture [24], also supporting the role of co-morbid conditions in the excess mortality. Postoperative occurrence of lung infections and heart failure are both associated with a very high short-term mortality (65% and 43% respectively after 30 days) indicating a strong role of complications occurring after the fracture [17]. This is supported by a study finding that pre-morbid conditions did not predict post fracture mortality, but rather that the mortality was associated with infections occurring after the fracture [18]. In addition to these factors a number of factors play a role. These may include surgical management with good operative techniques [25], experience [26], anaesthetics [27], and time from fracture to surgery [28]. In connection with time from fracture to surgery, one study indicated that time used to control co-morbid conditions pre-operatively did not adversely affect mortality [29]. Peri- and post-operative management with blood transfusion [30], prevention of deep venous thrombosis and pulmonary embolism, etc. are also important.
The following were thus the aims of the present study:
-
1)
To assess the effects of pre-morbid conditions on the risk of death following a hip fracture.
-
2)
To establish whether causes of death were related to pre-morbid conditions or post-operative complications in the short and long-term perspective.
-
3)
To evaluate the excess mortality after a hip fracture compared to the general population both in the short and long-term perspective.
Material and methods
In Denmark the widespread existence of registers covering contacts to the health sector offers good possibilities for studies on the occurrence of fractures [31]. The Danish National Health Service provides tax-supported healthcare for all inhabitants, allowing free access to general practitioners and hospitals. In addition, reimbursement is provided for a variable proportion of the costs of prescribed drugs. Using the unique 10-digit civil registry number that is assigned to all Danish citizens shortly after birth, a complete hospital discharge and prescription history can be established for each individual, and valid linkage between population-based registries can be obtained. The unique civil registry number definitively identifies each individual in all registers.
In Denmark, the National Hospital Discharge Register covers all contacts (on in- or out-patient basis) to the hospitals [32]. The register was founded in 1977, but outpatient records were first completely incorporated from 1995. The files of the National Hospital Discharge Register include information on the civil registry number of the patient, date of discharge, and discharge diagnoses (both principal diagnoses and additional diagnoses), assigned exclusively by the physician at discharge according to the Danish version of the International Classification of Diseases, 8th revision (ICD-8) until the end of 1993, and to the Danish version of the International Classification of Diseases, 10th revision (ICD-10). For fractures a classification of the energy of the trauma that led to the fracture (low, medium, high etc.) is available along with codes of the activity that was associated with the fracture (say an automobile accident), and the place where the accident took place (street, home etc.). The register has nationwide coverage of public hospitals with an almost 100% completeness of recordings and a high precision of diagnoses [32], especially of fracture diagnoses [33].
This cohort study was performed within the Danish population that constituted approximately 5.3 million individuals during the study period.
The study was subject to control by the National Board of Health, and the Danish Data Protection Agency.
Study design
The study was designed as a classical historic cohort study where exposure was presence of a hip fracture or not, and outcome was mortality. Covariates were co-morbidity, drug use and social variables.
Identification of hip fracture cases
All patients with a fracture of the hip (ICD8 codes 820.00 and 820.01, ICD10 codes S72.0 and S72.1) in Denmark in the 25-year period between January 1, 1977 and December 31, 2001 were retrieved from the National Hospital Register [32].
Identification of controls
Using the Civil Registration System, which has electronic records on all changes in vital status, including change of address and date of death for the entire Danish population since 1968, we randomly selected three controls for each case, matched by gender and year of birth. The controls were selected using the incidence-density sampling technique [34], i.e., the controls had to be alive and at risk for fracture diagnosis at the time the corresponding case was diagnosed.
The controls were required not to have been hip or femur fracture cases in the period from 1977 to 2001.
Identification of co-morbidity and other covariates
For both cases and controls all contacts to the national health system in the period January 1, 1977 to December 31, 2001 were retrieved to allow quantification of co-morbidity that was present before the time of fracture or emerged after the time of fracture.
The Charlson index, which is a validated index of 19 co-morbid conditions, was used to express a weighted index of co-morbidity [35]. Alcoholism was defined as having had a diagnosis related to alcoholism in the National Hospital Discharge Register [36].
Social covariates on income, educational and occupational status were retrieved from the National Bureau of Statistics (Statistics Denmark) [36]. These variables were retrieved for the year the fracture occurred.
Information on vital status
We retrieved information of migrations and date of death from the Central Person Register (via the National Bureau of Statistics). Information on cause of death was retrieved from the National Register of Causes of Death under the National Board of Health (via the National Bureau of Statistics).
Death certificates were completed by the treating hospital physicians or after discharge by the responsible general practitioners. In these certificates the cause of death is graduated into three levels: 1) the primary cause of death (the immediate cause of death), 2) the secondary contributing cause of death, and 3) the tertiary contributing cause of death. The secondary and tertiary causes of death are used when concurrent factors are part of the cause of death, e.g., a person dying after a trauma may have a heart condition that contributed to the death.
In our analyses of causes of death, we used two principal types of categorisation: 1) primary cause of death, which is the cause of death registered as the immediate cause of death, and 2) the underlying cause of death. The causes of death given by the treating physician are subsequently recoded by the National Board of Health using ICD8 and 10 codes and codes for deaths related to the accident/trauma that led to the fracture.
If a patient dies within 30 days of a major accident such as a car crash, the primary cause of death is coded as related to the trauma by international standards irrespective of the actual cause of death (say a myocardial infarction complicating the fracture). The actual cause of death is then coded as the secondary cause of death (the contributing cause of death). This classification thus necessitates analyses on two levels. In the latter case it was assessed if a secondary or tertiary cause was part of the underlying cause of death, i.e., if other factors besides the accident or trauma contributed.
Statistics
Data from the different registers were merged at the National Bureau of Statistics, and for each subject the ten-digit civil registry number was substituted by a unique case number i.e., as investigators we had no access to personally identifiable information. Mean and standard deviation were used as descriptive statistics. Crude odds ratios (OR’s) were calculated and 95% confidence intervals approximated using the method of Miettinen [37]. Survival was analysed using Cox proportional hazard method. It was checked that the effect of risk factors was proportional with time and this was found to be the case. From Fig. 1 it can be seen that for the controls, the risk was proportional with time, while for the fracture cases the risk was a little higher within the first year than within the subsequent years. However, this deviation did not affect the overall results.
Analyses were performed using STATA 8.1 (STATA Corp., College Station, Tx) and SPSS 14.0 (SPSS Inc., Chicago Ill.) -both in the Unix version.
Results
Baseline characteristics
Table 1 shows baseline characteristics of the fracture cases and controls. The cases and controls were well matched for age and gender. The prevalence of co-morbidity was statistically significantly higher in cases than in controls, while the difference in clinical terms was limited (45.3 vs. 40.5% with any co-morbid condition). One particular feature was that the hip fracture cases actually had a lower proportion with prior cancer, acute myocardial infarction and heart failure (Table 1). The proportion with extensive co-morbidity (Charlson index ≥ 5) was higher among the controls than the cases. A higher proportion of fracture cases than controls died during follow-up.
The mean number of days spent in hospital after the date of the hip fracture (or the corresponding dummy date among the controls, excluding the admission for the hip fracture among the cases) was 12.0 ± 22.1 in cases and 8.2 ± 16.0 among the controls, 2p < 0.01.
Effects of pre-fracture co-morbidity
Table 2 shows the effects of stratification for confounders on survival.
Crude analysis
Table 2 shows that the crude mortality risk for the entire time period after was more than doubled for the time period after the hip fracture in the patients compared to the time period after the corresponding “dummy” index date in the controls (HR = 2.26, 95% CI: 2.24–2.27). Men with hip fractures had a somewhat higher relative risk of death than women with hip fractures (HR = 2.75 vs. 2,09, p < 0.01 for direct comparison). There was an inverse relationship between age and excess risk of death. The older hip fracture patients had a much lower excess mortality than the younger (HR = 1.79 for patients ≥ 85 years, 2.06 for patients aged 75–84 years, 2.52 for patients aged 65–74 years, and 3.46 for patients < 65 years at the time of hip fracture, which was statistically significant: 2p < 0.01 for change with age by test for trend). This crude analysis shows that age interacted with the excess mortality risk associated with a hip fracture (i.e., age was an effect modifier), the excess mortality being higher among younger than older individuals, in the adjusted analysis below, the effect of age per se is presented. Co-morbidity had little influence on the risk of excess mortality in hip fracture cases compared to controls (no trend in HR with degree of co-morbidity).
Adjusted analysis
Table 2 shows that fracture cases had a mortality risk that was approximately twice that of the controls (HR = 1.95, 95% CI: 1.94–1.97) after adjustment for age, gender, and pre-fracture co-morbidity (Charlson index). These adjustments changed the overall mortality hazard ratio (HR = 1.95 adjusted vs. 2.26 unadjusted). Upon further adjustment for income a significant change in relative risk was observed (HR changed from 2.26 unadjusted to 1.66, p < 0.01 by direct comparison). The other variables only induced small changes in relative risk of death among hip fracture cases. Following adjustment, increasing degree of co-morbidity (Charlson index) was associated with an increase in relative mortality. Some co-morbid conditions (AIDS, dementia, kidney disease) were associated with a significantly higher relative risk than others (acute myocardial infarction and stomach and duodenal ulcers). However, the relative risk using the Charlson index (HR = 1.66) was similar to using the individual diseases (HR = 1.67) along with the other confounder variables.
The mortality increased steeply with increasing age at the time of fracture, and this association only changed little upon introduction of confounders. Please note that this age adjustment deviates from the crude analysis as it shows the effect of age per se, i.e., an increasing risk of death with age whereas the crude analysis shows that the effect of age on mortality differed between fracture cases and controls.
The trauma energy only seemed to play a minor role for the causes of death: 16.9% of patients with a hip fracture resulting from a fall at the same level died from trauma whereas this was the case for 16.4% of patients suffering a fall from one level to another (data not shown).
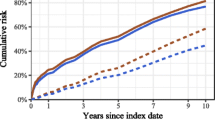
Actuarial survival
Figure 1 shows observed and expected survival. From Fig. 1a it can be seen that an excess mortality is present. The mean survival time was 11.1 ± 0.02 years in controls and 6.2 ± 0.02 years in hip fracture patients, i.e., a loss of life of 4.9 years on average. As the distribution of survival times tended to be skewed, an analysis of median survival was also performed. The median survival was 9.4 years among controls and 3.8 years among hip fracture patients. This is equal to a median loss of 5.8 years.
From Fig. 1b (log scale) it can be seen that a significant excess mortality takes place within the first year after the hip fracture. The survival after one year among the hip fracture patients was only 81% of that expected in an age- and gender matched normal population (equal to a loss of 19% of the expected survival). However, an excess mortality was still present more than one year after the hip fracture. For each year after the first year the observed survival was only 98.2% of what was expected (a loss of 1.8% per year). Although this was a numerically small excess mortality per year, it amounted to a large loss when cumulated over many years. After 20 years, the observed survival was only 57.4% of that expected (0.81 * 0.982(20–1) = 0.81 * 0.708 = 0.574), equalling a loss of 42.3% of that expected. However, the loss was 19% (81% of the expected within the first year), but 29.2% over the following 19 years (0.982(20–1) = 0.708 or 70.8% of that expected). The long-term excess mortality thus contributes more than the short-term excess over a period of 20 years. The general formula computed from Fig. 1 for observed survival (O) vs. expected (E) in an age- and gender matched section of the background population was: O = E * 0.81 * 0.982(y–1) for y ≥ 1 years, where y is years from hip fracture, and E = 0.9y, i.e., O = 0.81 * 0.9y * 0.982(y–1) for y ≥ 1 years.
Figure 2 shows that the relative risk of death was higher within the first half year following the hip fracture than later.
Causes of death
Primary cause of death
Table 3 shows the distribution of primary causes of death. The fracture cases had a significant excess mortality from causes linked to trauma complications, with smaller proportions of the excess mortality linked to infectious diseases, psychiatric disorders, neurological disorders, dementia, and a variety of other infrequent causes. Deaths caused by cancer and cardiovascular diseases were under-represented as a consequence of the relative excess of the before-mentioned causes.
Within the first 30 days following the index date, 70.8% of all deaths within the hip fracture cases were due to trauma related complications versus only 2.5% trauma related complications among controls, i.e., an excess of 68.3%. More than 30 days after the fracture 7.6% of all deaths were due to complications related to the fracture-releasing trauma versus 1.8% trauma related deaths among the controls.
Within the first year following a hip fracture, 30.7% of all primary causes of death were related to the fracture-releasing trauma among hip fracture cases vs. 2.2% trauma related deaths among the controls. More than one year after the hip fracture, 2.8% of all deaths were primarily caused by traumas vs. 0.9% among controls.
The proportion of deaths linked to complications related to the trauma increased steadily from 7.5% in patients < 65 years over 9.5% in hip fracture patients aged 65–74 years, 14.3% in patients aged 75–84 years to 21.9% in patients aged 85 years or more (p for trend < 0.01).
Underlying cause of death besides trauma related
Table 4 shows the underlying cause of death besides the trauma (patients whose primary cause of death were trauma related were examined for secondary or tertiary causes of death). In most cases other causes than the accident were contributing to the death (almost all patients dying with a primary cause of death registered as trauma related had secondary of tertiary causes not related to the accident). In only 562 and 88 subjects, respectively, was the trauma the only registered cause of death. Table 4 shows a somewhat different picture from Table 3. Although statistically significant differences were still present, the absolute differences were much smaller for several causes of death. Whereas the percent of cardiovascular deaths changed little among the controls (from 40.1% to 40.5%) there was a large change from 31.2 to 38.0% among the hip fracture cases, i.e., a relatively large part of deaths primary linked to trauma had a component linked to cardiovascular disease.
Table 4 also shows that there was an excess risk of death from all causes in hip fracture cases compared to controls in absolute terms. i.e., was the overall excess risk of death around 2.26 times that of the controls. Hip fracture cases also had a risk of death from cancer that was higher than in controls (HR = 1.64). However, as this relative risk of dying from cancer was lower than the overall relative risk, the percent that died from cancer was smaller among hip fracture cases (13.2%) than among controls (20.6%- i.e., the ratio 13.2/20.6 = 0.64 was within the range of 1.64/2.26 = 0.73, the small difference being due to the fact the first ratio was a risk ratio, that did not take time till death into account, whereas the latter was a rate ratio that took time till death into account).
The factors that in both absolute and relative terms contributed the most to death following a hip fracture besides the trauma related deaths were: infections (relative difference 8.5–5.0 = 3.5%), psychiatric diseases (2% difference), pulmonary diseases (1.2%), dementia (1%), and neurological diseases (0.8%).
During the extended observation period changes took place in survival among cases and controls, but these did not interact with the results presented here (data not shown).
Discussion
In this large-scale cohort study we have shown a significant excess mortality after a hip fracture. Within the first year following the fracture a significant excess mortality of around 20% was present, mainly linked to trauma related complications. This is in accordance with the finding that the excess mortality only changed little upon adjustment for pre-morbid conditions except for income. There was a small excess annual mortality for the remainder of the observation period. Although small on an annual basis, this excess mortality amounted to a significant excess mortality with time. This long-term excess mortality seemed linked to a number of factors including income. Higher income may be a proxy for a number of variables related to social status (having a job, social position, social security etc.). This points to not only medical measures but also perhaps social measures in the prevention of mortality following a hip fracture.
Our study thus supports that it is post fracture conditions related to the trauma rather than pre-fracture co-morbid conditions that predicts mortality. The fact that co-morbidity was a less significant predictor of survival is interesting, as it may signal that the care for the hip fracture patients is at a level where the effects of pre-fracture co-morbidity is neutralised by the medical care, whereas the medical care needs to be optimised to reduce the mortality linked to immediate post-fracture conditions. The post fracture conditions that contributed the most to the excess mortality were infections and psychiatric conditions.
As post fracture conditions seemed responsible for the increased mortality, medical measures to prevent mortality should be directed at these factors, infections in particular. Lung diseases such as asthma, chronic obstructive pulmonary disease and emphysema could also be points of prevention as they also contributed to the excess mortality.
The observation that post fracture rather than pre-fracture conditions were responsible for the excess mortality is in accordance with the studies by Roche et al. [17] and Wehren et al. [18]. In the study by Roche et al. [17], 59% had at least one co-morbid condition compared to around 55% in our study. However, the definition of co-morbidity was broader in the study by Roche et al. [17] than in our study. Roche et al. reported a mortality of 9.6% at 30 days compared to 13% in our study, and a one-year mortality of 33% compared to 29% in our study. The mean age in their study was 82 years [17] compared to 77 years in our study, and 80% of their patients were women [17] compared to 72% in our study. They also reported a higher mortality in men than in women [17]. The observed 30 days mortality in their study [17] is considerably lower than in our study given that the age of their patients was higher and the proportion of men smaller. However, their one-year survival [17] was about the same level as in our study. They excluded patients < 60 years, patients with pathological fractures, and patients not undergoing surgery [17]. This may have led to a selection of more “fit” patients in their cohort [17], which may explain the differences in short-term mortality as our cohort included all patients with a hip fracture.
In the study by Wehren et al. [18] 78% were women, which was also a higher proportion than in our study. The mean age in their study of 81 years [18] was also considerably higher than in our study. They reported a one-year mortality of around 25%, i.e., lower than in our study considering age and gender distribution.
The finding that the majority of mortality in the short-term perspective is attributable to the hip fracture is in accordance with Dutch results [38].
The prior studies on mortality rates and causes of death have focused on short-term mortality (two years in the study by Wehren et al. [18], and one year in the study by Roche et al. [17]). Our study provides insight into long-term mortality showing an excess mortality even many years after the hip fracture pointing at the necessity of not only short-term prevention of mortality but also long-term prevention. The long-term excess mortality is in accordance with the findings by Schroder and Erlandsen [14], but in contrast with several other studies on excess mortality in hip fracture patients compared to the general population finding only an excess mortality for the first year or less following the hip fracture [2, 3, 6–13]. However, as mentioned in the introduction, several of these studies were small and had a limited time of follow-up. In our study the excess mortality was still present after adjustment for several important confounders.
If the hip fracture trauma per se is the main predictor of mortality, the main focus for preventing the excess deaths after a hip fracture is to prevent the fracture to occur. Antiosteoporotic drugs that increase BMD decrease the risk of hip fractures, and thus potentially the overall mortality [39]. However, all measures to prevent osteoporosis and falls or other traumas that may lead to hip fractures or to ameliorate the consequences of say a fall (e.g., hip protectors) may also be efficient in reducing overall mortality in the general population of older age or in institutionalised elderly persons, as hip fractures are quite frequent.
During a long observation period as the one presented here changes in the management of patients with hip fractures took place both with respect to surgical practices, anaesthetics, and postoperative management. However, these changes with time did not interact with the results presented here.
The reasons for the lower cancer mortality among cases than controls are not readily explained. However, several factors may play a role. The prevalence of cancer was a little lower among hip fracture cases than controls (12 vs. 14%, Table 1). The lower frequency of cancer as primary cause of death among hip fracture patients than controls (12.5 vs. 20.4%, Table 3) may be due to the fact that trauma related causes of death were so frequent that other causes of death were very low among patients. However, this does not completely explain the difference, as cancer was only present as underlying cause of death in 13.2% of cases vs. 20.6% of controls (Table 4). Another possibility is the fact that the incidence of cancer increases with age. However patients with a hip fracture have a substantial reduction in observed rest lifetime. Their shorter lifetime may, thus, mean that fewer live long enough to develop cancer or to have a cancer diagnosed.
Strengths and weaknesses of the study
The main strengths of the study are the high validity of a hip fracture diagnosis [33], the completeness of registration and the completeness of follow-up [32]. The study is thus considerably larger than prior studies within the field and offers a much longer follow-up, which has disclosed a long-term excess mortality besides the short-term excess mortality.
The weaknesses are lack of detailed information on individual life-style variables, like smoking habits, consumption of alcohol, and e.g., body mass index. The fact that the high mortality in the hip fracture group meant that many in this group had a recent major event namely the fracture and that many deaths may have occurred during hospitalisations in contrast to deaths occurring later in the course and in the control population. The attention on causes of death may thus have been different, e.g., may more diagnostic procedures and autopsies have been performed in patients dying after a recent hip fracture than in controls where a larger proportion of deaths may have been considered as natural. We did not have information on the frequency of autopsies in the two groups, and cannot therefore decide whether differences in these may have affected the registration of causes of death.
The consumption of health services after the hip fracture may also have affected the registration of the causes of death; patients being in tight contact with (or admitted to) say a hospital department, an outpatient clinic, or their general practitioner may be more likely to have an exact diagnosis of the cause of deaths in contrast to patients not having such contacts. We did not have information on the number and nature of contacts to the general practitioner, and this is a weakness of the study. Regarding hospital contacts, the patients had about 4 more days in hospital than the controls on average after the date of the fracture (12 vs. 8 days), perhaps due to complications after the fracture, re-operations, and re-admissions for rehabilitation. This may have meant a better registration of complications in cases than in controls.
In conclusion patients with a hip fracture have a pronounced excess mortality risk. The major cause was linked to factors associated with the accident that caused the fracture. Prevention may thus best be directed at reducing the number of hip fractures and the immediate medical care of the patients.
References
Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ (2002) Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc 50:1644–1650
Jacobsen SJ, Goldberg J, Miles TP et al (1992) Race and sex differences in mortality following fracture of the hip. Am J Public Health 82:1147–1150
Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE (1989) Survival experience of aged hip fracture patients. Am J Public Health 79:274–278
Magaziner J, Lydick E, Hawkes W et al (1997) Excess mortality attributable to hip fracture in white women aged 70 years and older. Am J Public Health 87:1630–1636
Johnell O, Kanis JA (2004) An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 15:897–902
Pitto RP (1994) The mortality and social prognosis of hip fractures. A prospective multifactorial study. Int Orthop 18:109–113
Miller CW (1978) Survival and ambulation following hip fracture. J Bone Joint Surg Am 60:930–934
Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ III (1993) Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Kreutzfeldt J, Haim M, Bach E (1984) Hip fracture among the elderly in a mixed urban and rural population. Age Ageing 13:111–119
Dahl E (1980) Mortality and life expectancy after hip fractures. Acta Orthop Scand 51:163–170
Holmberg S, Conradi P, Kalen R, Thorngren KG (1986) Mortality after cervical hip fracture. 3002 patients followed for 6 years. Acta Orthop Scand 57:8–11
Parker MJ, Anand JK (1991) What is the true mortality of hip fractures? Public Health 105:443–446
Poor G, Atkinson EJ, O’Fallon WM, Melton LJ III (1995) Determinants of reduced survival following hip fractures in men. Clin Orthop Relat Res 260–265
Schroder HM, Erlandsen M (1993) Age and sex as determinants of mortality after hip fracture: 3,895 patients followed for 2.5–18.5 years. J Orthop Trauma 7:525–531
Jensen JS, Tondevold E (1979) Mortality after hip fractures. Acta Orthop Scand 50:161–167
Handoll HHG, Farrar MJ, McBirnie J et al (2002) Heparin, low molecular weight heparin and physical methods for preventing deep vein thrombosis and pulmonary embolism following surgery for hip fractures. Cochrane Database of Systematic Reviews CD000305
Roche JJW, Wenn RT, Sahota O, Moran CG (2005) Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 331:1374
Wehren LE, Hawkes WG, Orwig DL et al (2003) Gender differences in mortality after hip fracture: the role of infection. J Bone Mineral Res 18:2231–2237
Ramnemark A, Nyberg L, Borssén B, Olsson T, Gustafson Y (1998) Fractures after stroke. Osteoporosis Int 8:92–95
Ensrud KE, Thompson DE, Cauley JA et al (2000) Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc 48:241–249
Kado DM, Duong T, Stone KL et al (2003) Incident vertebral fractures and mortality in older women: a prospective study. Osteoporosis Int 14:589–594
Browner WS, Pressman AR, Nevitt MC, Cummings SR (1996) Mortality following fractures in older women. The study of osteoporotic fractures. Arch Intern Med 156:1521–1525
Ceder L, Elmqvist D, Svensson SE (1981) Cardiovascular and neurological function in elderly patients sustaining a fracture of the neck of the femur. J Bone Joint Surg Br 63B:560–566
Nettleman MD, Alsip J, Schrader M, Schulte M (1996) Predictors of mortality after acute hip fracture. J Gen Intern Med 11:765–767
Bannister GC, Gibson AG, Ackroyd CE, Newman JH (1990) The fixation and prognosis of trochanteric fractures. A randomized prospective controlled trial. Clin Orthop Relat Res 242–246
Lavernia CJ (1998) Hemiarthroplasty in hip fracture care: effects of surgical volume on short-term outcome. J Arthroplasty 13:774–778
Davis FM, Woolner DF, Frampton C et al (1987) Prospective, multi-centre trial of mortality following general or spinal anaesthesia for hip fracture surgery in the elderly. Br J Anaesth 59:1080–1088
Bottle A, Aylin P (2006) Mortality associated with delay in operation after hip fracture: observational study. BMJ 332:947–951
Bergeron E, Lavoie A, Moore L et al (2006) Is the delay to surgery for isolated hip fracture predictive of outcome in efficient systems? J Trauma 60:753–757
Halm EA, Wang JJ, Boockvar K et al (2003) Effects of blood transfusion on clinical and functional outcomes in patients with hip fracture. Transfusion 43:1358–1365
Frank L (2000) Epidemiology. When an entire country is a cohort. Science 287:2398–2399
Andersen TF, Madsen M, Jørgensen J, Mellemkjær L, Olsen JH (1999) The Danish National Hospital Register. Dan Med Bull 46:263–268
Vestergaard P, Mosekilde L (2002) Fracture risk in patients with celiac disease, Crohn’s disease, and ulcerative colitis: a nation-wide follow-up study in 16,416 patients in Denmark. Am J Epidemiol 156:1–10
Wacholder S, McLaughlin JK, Silverman DT, Mandel JS (1992) Selection of controls in case-control studies. I. Principles. Am J Epidemiol 135:1019–1028
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 40:373–383
Vestergaard P, Rejnmark L, Mosekilde L (2006) Socioeconomic aspects of fractures within universal public healthcare: a nationwide case-control study from Denmark. Scand J Public Health 34:371–377
Miettinen OS (1985) Theoretical epidemiology: principles of occurrence research in medicine, 1 edn. Wiley, New York
Boereboom FT, Raymakers JA, Duursma SA (1992) Mortality and causes of death after hip fractures in The Netherlands. Neth J Med 41:4–10
Cree MW, Juby AG, Carriere KC (2003) Mortality and morbidity associated with osteoporosis drug treatment following hip fracture. Osteoporos Int 14:722–727
Acknowledgements
Statistics Denmark (Danmarks Statistk) is acknowledged for invaluable help with the data.
Research Librarian miss Edith Clausen is acknowledged for skilful technical assistance with the references.
Financial support
Financial support was provided by the family Christenson-Ceson’s Family Foundation and Helga and Peter Korning’s Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vestergaard, P., Rejnmark, L. & Mosekilde, L. Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int 18, 1583–1593 (2007). https://doi.org/10.1007/s00198-007-0403-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-007-0403-3