Abstract
Summary
Bisphosphonates are the first-line treatment for osteoporotic (OP) women; however, therapy is not recommended in severe renal impairment (RI). This study examined RI prevalence among OP women. Nearly a quarter of women had moderate RI, and 3.59 % would not be recommended for bisphosphonates, demonstrating a need for better therapeutic alternatives.
Introduction
Bisphosphonates are the recommended first-line treatment for postmenopausal women with OP. However, bisphosphonates are cleared through the kidney, and therapy is not recommended in severe RI due to adverse treatment effects observed with intravenous formulations. The objective of this study was to examine the prevalence of RI among women with OP aged ≥50 years in the USA.
Methods
Women with OP aged ≥50 years were identified using the 2005–2008 National Health and Nutrition Examination Survey (NHANES) data. OP was defined as prior OP diagnosis, previous hip or spine fracture, or measured lumbar spine/femoral neck bone mineral density (BMD) T-score <−2.5. The 2005 Modification of Diet in Renal Disease (MDRD) formula was used to calculate the glomerular filtration rate (GFR). Moderate and severe RI was defined as GFR 30–59 and 15–29 mL/min, respectively. Bisphosphonate therapy was considered not recommended among women with OP if GFR was <35 mL/min.
Results
The prevalence of OP among women in USA aged ≥50 years was 27 % (12.7 million). Nearly a quarter of women with OP (23.54 ± 2.02 %; 2.9 million) had moderate RI and 1.88 ± 0.28 % (230,000) had severe RI. Correspondingly, bisphosphonate therapy would not be recommended for an estimated 439,000 women with OP (3.59 ± 0.73 %).
Conclusions
Nearly a quarter of postmenopausal women with OP have moderate RI, and over 3 % would not be recommended for bisphosphonate treatment. These data reveal a need for better therapeutic alternatives that can be used in this patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis (OP) poses a major health concern for postmenopausal women in the USA. Current estimates, using National Health and Nutrition Examination Survey (NHANES) 2005–2008 data, have found that approximately 11–30 % of women aged ≥50 years have OP, depending on the definition used, and the prevalence of low bone mineral density (BMD) of the spine or femoral neck is nearly 50 % in this group of women [1, 2]. Among postmenopausal women with OP, the rate of bone fractures is approximately four times that among women with normal BMD, and low BMD is associated with a 1.8-fold higher rate of fracture [3]. Furthermore, postmenopausal women with prior bone fractures are at increased risk of experiencing repeat fractures [4].
Current guidelines recommend bisphosphonates as first-line treatment for postmenopausal women with OP and low BMD at risk of spine or hip fracture [5]. The efficacy of both oral and intravenous bisphosphonates, including alendronate, ibandronate, risedronate, and zoledronic acid, to reduce the risk of fracture has been well documented [6–10]. On the other hand, all bisphosphonates are excreted through the kidneys [11], which has raised the concern that therapy may increase the risk of renal adverse events among patients with renal impairment (RI) [12, 13]. Although the clinical literature on the safety of bisphosphonates among osteoporotic women with moderate and severe RI remains limited [14], the US Federal Drug Administration (FDA) and product manufacturers have defined lower limits for impaired renal function below which therapy is not recommended [15–18]. For alendronate and zoledronic acid, this threshold is defined as creatinine clearance [CrCl] <35 mL/min; for ibandronate and risedronate, the threshold is CrCl <30 mL/min. In general, bisphosphonates are not considered to be toxic to the kidney, although intravenous zoledronic acid administration must follow labeled guidelines [13].
Given these treatment recommendations, understanding the current prevalence of RI among postmenopausal women with OP can help identify an important unmet medical need in this patient population. Therefore, the objective of this study was to examine the current prevalence of moderate and severe RI among women with OP aged ≥50 years in the USA, in comparison with the general population of females aged ≥50 years, using the NHANES 2005–2008 data.
Methods
Sample
The NHANES are conducted by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention, to examine the health and nutritional status of large representative cross-sectional samples of the non-institutionalized, US civilian population. Detailed descriptions of the NHANES data collection procedures are provided elsewhere [19, 20]. Briefly, the NCHS releases NHANES data in biennial cycles; the present study utilized data from the 2005–2006 and 2007–2008 cycles. The surveys are conducted using a complex, stratified, multistage, probability-cluster sampling design to provide representative data for three race/ethnic groups: non-Hispanic whites, non-Hispanic blacks, and Mexican Americans. As of 2007, the survey has been redesigned to oversample the entire Hispanic population, in addition to the Mexican American population. Variables used in the present study were collected from a combination of household interviews and physical examinations conducted in specially equipped mobile examination centers among a subgroup of the study participants. All procedures were approved by the NCHS Ethics Review Board, and written informed consent was obtained from all survey participants.
Sample inclusion criteria for the present study included women aged ≥50 years, a commonly accepted age group considered to be postmenopausal and at high risk for osteoporosis [1, 2]. Only participants with complete laboratory and physical examination information, including osteoporosis diagnosis status and measurement of renal function, as further described below, were included in the final study sample.
Study variables
Osteoporosis
The presence of OP was defined in accordance with the National Osteoporosis Foundation guidelines [5]. Women aged ≥50 years were considered to have OP if they reported: (1) prior OP diagnosis, (2) a previous hip or spine fracture, or (3) had a measured lumbar spine or femoral neck bone mineral density (BMD) T-score less than −2.5 at time of examination. If an individual reported prior OP diagnosis or hip fracture but the measured T-score did not meet the set criterion, the individual was still considered to have OP (and vice versa).
As described in the NHANES 2005–2006 and 2007–2008 study protocols, BMD of the lumbar spine and femoral neck were measured with Hologic QDR 4500A fan-beam densitometers (Hologic, Inc., Bedford, MA, USA) using Apex version 3.0 software (lumbar spine) or Discovery version 12.4 software (femur neck) [21–24]. In both surveys, the left hip was scanned unless there was a history of previous fracture or surgery. Rigorous quality control (QC) programs were employed, which included the use of anthropomorphic phantoms and review of each QC and respondent scan at a central site (Department of Radiology of the University of California, San Francisco), using standard radiologic techniques and study-specific protocols.
T-scores were calculated as follows:
The reference group for the femoral neck BMD measurements included non-Hispanic white women aged 20–29 years from NHANES III [25, 26], and the reference group for the lumbar spine included white females aged 30–40 years from the dual-energy X-ray absorptiometry manufacturer reference database [27]. Specific thresholds to define osteoporosis were ≤0.858 (SD, 0.120) g/cm2 and ≤1.047 (SD, 0.11) g/cm2 for the femoral neck and spine, respectively.
Renal impairment
Serum creatinine (Scr) was measured at the time of examination among participants aged ≥12 years as described in the NHANES study protocols [28, 29]. The 2005 Modification of Diet in Renal Disease (MDRD) formula was used to calculate the glomerular filtration rate (GFR), as a function of measured Scr, age, race, and gender [30]:
Lower levels of GFR correspond to diminished kidney function.
RI was categorized into stages, with increasing stage numbers corresponding to increased severity, according to the National Kidney Foundation classification system [31, 32]. Cut points for no/minor RI (stages 0–2), moderate RI (stage 3), severe RI (stage 4), and renal failure (stage 5) were categorized as GFR ≥60, 30–59, 15–29, and <15 mL/min, respectively. The upper limit for defining severe RI below which bisphosphonate therapy is not recommended was defined as GFR <35 mL/min [15–18].
Demographics and clinical characteristics
Relevant demographics including age, race/ethnicity, and education level, as well as documented risk factors associated with impaired renal function [31, 33], including increased body mass index (BMI), hypertension, diabetes, and cardiovascular disease (CVD), were identified. Race categories included White (non-Hispanic), Black (non-Hispanic) and other/Hispanic/mixed, and self-reported education level was categorized as less than high school or high school graduate/General Education Diploma or higher. BMI (kg/m2) was calculated using the height and weight measurements obtained at survey entry and classified according to World Health Organization definitions: normal BMI, <25; overweight BMI, 25–29.9; and obese BMI, >30 [34]. Diagnoses of hypertension were based on a systolic blood pressure >140 mmHg or a diastolic blood pressure >90 mmHg at latest examination, or self-reported diagnosis or self-reported use of a prescription medication. Diabetes mellitus (types 1 or 2) was defined based on self-reported diagnosis. Cardiovascular disease was also defined based on self-reported diagnosis of congestive heart failure, coronary heart disease, angina, stroke, or heart attack.
Statistical analysis
The prevalence of RI was estimated by the abovementioned demographic and clinical characteristics among women with osteoporosis aged ≥50 years and, to form a basis of comparison, among the overall US female population aged ≥50 years. Characteristics of the study population were described using percentages. Statistical analyses were conducted using SAS version 9.3, and SUDAAN version 10.1 (Research Triangle Institute, Research Triangle Park, North Carolina) was used to calculate national estimates and their 95 % confidence intervals (CI), age standardized to the 2000 US census population. Data were analyzed using sample weights to account for differential probabilities of sample selection, nonresponse, and sample noncoverage. Taylor series linearization was used for variance estimation. In cases where the sample size was too small to provide a reliable prevalence estimate, indicated by a ratio of the standard error/percent >40 %, results were not reported.
Results
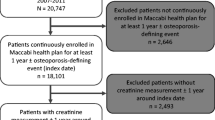
A total of 9,914 women participated in NHANES 2005–2008, of which 3,831 women were aged ≥50 years (Fig. 1) [35, 36]. Among female participants aged ≥50 years, 2,522 women (66 %) were both interviewed and examined, and 738 women were classified as having OP. Measurements of Scr for GFR calculations were unavailable for 7 % of women aged ≥50 years (n = 183) and 6 % of women aged ≥50 years with OP (n = 45). Characteristics among the full sample of women aged ≥50 years compared with those without available renal function measurements appeared similar; however, statistical tests comparing the two samples were not conducted, as the number without renal function measurement was too small to provide reliable national estimates [37]. Thus, the final analytical sample included 2,339 women aged ≥50 years, representing a projected 44.8 million females in the US population, and 693 osteoporotic women with available renal function measurements.
Among women aged ≥50 years, the estimated crude prevalence of OP was 26.9 % (N = 12.7 million; data not shown). Women with OP generally shared a similar distribution of demographics and clinical characteristics as the full sample of women aged ≥50 years (Table 1). However, women with OP tended to be older (48.61 vs. 30.78 % aged ≥70 years) and more educated (≥high school education, 79.13 vs. 72.02 %), had a slightly higher frequency of CVD (15.22 vs. 10.61 %) and diabetes (16.69 vs. 14.47 %), and lower frequency of obesity (24.47 vs. 37.05 %) compared with all women aged ≥50 years.
Nearly a quarter of women with OP (23.54 % [95 % CI, 19.42–27.65 %]; 2.9 million) had moderate RI (GFR, 30–59 mL/min), and 1.88 % (1.31–2.45 %; 230,000) had severe RI (GFR 15–29 mL/min) (Table 2). Correspondingly, an estimated 439,000 women with OP (3.59 % [2.10–5.08 %]) would not be recommended for bisphosphonate therapy based on a GFR <35 mL/min. The estimated prevalence of both moderate and severe RI among women with osteoporosis was slightly higher than the estimated prevalence for the full sample of women aged ≥50 years (moderate RI, 19.81 % [17.43–22.20 %]; severe RI, 1.12 % [0.78–1.45 %]).
Among women with OP, older compared with younger women had a higher prevalence of moderate RI (Table 3). The estimated prevalence of moderate RI among women with OP aged ≥70 years was 34.03 % (29.75–38.31 %) compared with 13.62 % (8.55–18.68 %) among women with OP aged 50–69 years. Osteoporotic women with hypertension and CVD also had a higher prevalence of moderate RI (hypertension, 29.75 % [23.99–35.51 %]; CVD, 32.79 % [25.32–40.25 %]), than women with OP who did not have these conditions (no hypertension, 15.81 % [10.53–21.10 %]; no CVD, 21.88 % [17.32–26.44 %]). Similar trends for the prevalence of GFR <35 mL/min, for which bisphosphonate therapy is not recommended, were observed across the CVD and hypertension categories; however, the sample size was generally too small to provide reliable prevalence estimates for these groups.
Discussion
Bisphosphonates are currently the recommended first-line treatment for postmenopausal women with OP [5]. However, bisphosphonates are cleared through the kidney, and therapy is not recommended in severe RI due to adverse treatment effects observed with intravenous formulations [38]. The results of this study suggest that nearly one quarter (24 %) of women aged ≥50 years with OP in the USA have moderate RI (GFR 30–59 mL/min) and approximately 4 % have a GFR <35 mL/min, below which bisphosphonate therapy is not recommended [15–18]. These results translate to an estimated 439,000 women who would not be recommended for bisphosphonate treatment.
Although the US Federal Drug Administration and product manufacturers currently do not recommend bisphosphonate therapy among osteoporotic women with severe RI [15–18], the clinical literature on the safety of bisphosphonates among individuals with OP and moderate to severe RI remains limited [14]. Studies of oral bisphosphonates were largely based on small sample sizes, particularly for patients with severe RI (GFR <30 mL/min), and a relatively short treatment duration [14]. A sub-analysis of the Fracture Intervention Trial did not find a significant difference in the number of renal or other adverse events associated with alendronate treatment among women with moderate (GFR <45–59 mL/min) to severe (GFR <45 mL/min) RI compared with no/moderate RI (GFR ≥60 mL/min) [39]. Likewise, a pooled analysis of nine clinical trials of risedronate in patients with mild (CrCl >50 to <80 mL/min) to severe (CrCl <30 mL/min) RI demonstrated a similar incidence of renal adverse events compared to placebo, regardless of renal function [40].
Results of the HORIZON Pivotal Fracture Trial have additionally established the short and long-term safety of IV zoledronic acid among postmenopausal women with severe RI (CrCl <30 mL/min) [41]. The study noted that zoledronic acid may be associated with transient increases in Scr over the first 9–11 days post-treatment. Follow-up among the small group of patients (n = 31) who experienced short-term significant increases in Scr showed that the levels had returned to pre-infusion values within 12 months, demonstrating no cumulative effect on renal function. Although transient, small increases in Scr should not be taken lightly. Current guidelines define acute kidney injury as an increase in Scr of ≥0.3 mg/dL within a 48-h period [42]. Acute kidney injury has been associated with an increased risk of progression to renal impairment, and implies even greater concern for patients with moderate to severe RI [42]. Therefore, further research, using larger sample sizes, is needed to better establish the safety of bisphosphonates among women with OP and severe RI before treatment can be recommended in this population.
In the present study, the prevalence of impaired renal function among osteoporotic women increased with age and was higher among individuals with certain risk factors, such as hypertension and CVD, which were fairly common in this patient population. As prior research suggests that RI can increase the risk of CVD, retinopathy and diabetes complications, clinical guidelines recommend regular monitoring of kidney function to prevent further complications [32]. Osteoporotic patients with chronic kidney disease mineral and bone disorder (CKD–MBD) represent an additional risk group for whom bisphosphonate treatment may pose increased cardiovascular risk by altering vascular calcification [43]. However, conclusive evidence regarding the safety and efficacy of bisphosphonates among patients with CKD–MBD is largely lacking, as few patients in clinical trials of bisphosphonates have had biochemical changes that could suggest CKD–MBD [43, 44]. Among postmenopausal women with OP, clinical trials of both the intravenous and oral formulations of ibandronate found that aortic calcifications increased over 3 years follow-up [45]. However, similar increases were seen among patients taking placebo, suggesting that ibandronate does not increase the risk of vascular calcification. Likewise, another study found increased calcium deposition in women with osteoporosis after 2 years of alendronate with a similar rate seen in the control group [46]. Recognizing the need for further research, clinical guidelines recommend that patients with moderate to severe RI (GFR <60 mL/min) with biochemical abnormalities of CKD–MBD and OP should be continually monitored for changes in renal function and receive additional investigation with bone biopsy prior to bisphosphonate therapy [43].
Recent clinical trial evidence suggests that denosumab is an effective alternative treatment to bisphosphonates for the prevention of fractures among women with OP. In postmenopausal women with OP, the subcutaneous administration of 60 mg of denosumab every 6 months for 36 months significantly reduced the risk of vertebral, nonvertebral, and hip fractures [47]. Furthermore, there were no significant differences between subjects who received denosumab and those who received placebo in the total incidence of adverse events, including renal adverse events. However, comparisons of efficacy are limited because there has been no head-to-head trial comparing rates of fracture reduction associated with denosumab and bisphosphonates. Therefore, further research is needed before denosumab can be used in the first-line setting, although results are promising for osteoporotic women with severe RI.
In the present study, approximately 27 % of postmenopausal women (12.7 million) were identified as having osteoporosis, which is consistent with reported prevalence estimates from prior NHANES studies [1, 2]. Looker et al. provided a more stringent definition of OP, based on a femoral neck or spine BMD score less than −2.5 at time of examination, resulting in a lower estimated prevalence of OP of approximately 11 % [2]. In contrast, Dawson-Hughes et al. provided a broader definition of eligibility for OP treatment, which included individuals with an elevated 10 years risk of fracture using the Fracture Risk Assessment Tool (FRAX) [5], in addition to self-reported hip or spine fractures and BMD T-scores less than −2.5 at examination. As a result, the study reported a higher estimated prevalence of OP among women aged ≥50 years (30.8 %, 13.8 million) [1]. Unfortunately, the algorithms used for FRAX score estimation were unavailable during the time of this study, which would have resulted in a slightly larger sample size of osteoporotic women for the estimation of RI prevalence.
Although prior studies have estimated the prevalence of RI for the general US population [48, 49], the present study, to the best of our knowledge, is the first to estimate the prevalence of RI among postmenopausal women with OP for whom bisphosphonate therapy is not recommended. The results showed that the prevalence of moderate and severe RI among osteoporotic women aged ≥50 years was slightly higher than the estimated prevalence among the broader population of females aged ≥50 years. Consistent with prior studies for the general population [48, 49], specific risk factors such as older age (≥70 years) and the presence of hypertension and CVD were associated with a higher prevalence of RI. These conditions were slightly more prevalent among women with osteoporosis than the full sample of women aged ≥50 years, largely explaining the higher prevalence of RI in this subpopulation.
This study, using a nationally representative sample of women aged ≥50 years, provides valuable insights into the burden of RI among postmenopausal women with osteoporosis in the USA. Nevertheless, the study has certain limitations. As with any survey-based study, certain variables may have measurement error due to recall bias. In the present study, potential recall bias was minimized through the use of T-scores to supplement self-reported diagnoses of OP, and renal function was estimated using laboratory data collected at examination. A number of subjects included in the study may have been on treatment or had been treated for OP before the study surveys were conducted. Unfortunately, the study surveys do not include information on prior medications, and current medications or treatments are not reliably captured. Additional information on prior OP treatment could provide further context on the prevalence of RI in this patient population. In addition, individuals who are institutionalized in nursing homes, an important risk group for osteoporosis [50], are excluded from the NHANES sampling frame by design. As a result, the prevalence of both osteoporosis and RI are likely higher than those reported in this study.
Based on available data, the study used the modified four-variable MDRD formula to estimate GFR, which has been validated for use in clinical practice, and according to nonbinding guidance published by the FDA, may be used during treatment assignment [30, 51]. Estimated GFR is now widely reported in general medicine and nephrology, and in most circumstances, is sufficient for clinical decision making including diagnosis, prognosis, and treatment of patients [30, 32]. It is important to note, however, that a GFR cut point of <35 mL/min is close but not directly equivalent to a CrCL cutpoint <35 mL/min, and may result in a slight overestimated prevalence [30, 32]. Likewise, estimated GFR was based on a single measurement, whereas in general practice, the clinical case definition requires multiple consecutive measurements [32]. Therefore, other nationally representative studies using both more precise and multiple measures of RI are needed to confirm the study results. A larger sample size would also likely improve estimates of the prevalence of severe RI according to important risk factors, such as increased BMI, hypertension, and CVD [31, 33]. Lastly, patients with CKD–MBD represent an additional risk group with RI who may not benefit from bisphosphonate treatment [43]. Given that NHANES is a cross-sectional survey, the database does not contain serial measurements of serum levels of calcium, phosphorus, parathyroid hormone, and alkaline phosphatase activity over time to effectively assess the prevalence of CKD–MBD among the population of patients with renal impairment. Further research is needed to better understand the prevalence of this important condition to further guide treatment decisions for women with OP.
Conclusions
In conclusion, bisphosphonates are currently the recommended treatment for postmenopausal women with OP. However, therapy is not recommended among women with severe RI due to adverse treatment effects. Nearly one quarter of US women with osteoporosis aged ≥50 years are estimated to have moderate RI, and over 3 %, translating to an estimated 439,000 women, would not be recommended for bisphosphonate treatment. These data reveal an unmet medical need in patients with both osteoporosis and impaired renal function, and a need for better therapeutic alternatives for use in this patient population.
References
Dawson-Hughes B, Looker AC, Tosteson AN, Johansson H, Kanis JA, Melton LJ III (2012) The potential impact of the National Osteoporosis Foundation guidance on treatment eligibility in the USA: an update in NHANES 2005–2008. Osteoporos Int 23(3):811–820. doi:10.1007/s00198-011-1694-y
Looker AC, Melton LJ III, Harris TB, Borrud LG, Shepherd JA (2010) Prevalence and trends in low femur bone density among older US adults: NHANES 2005–2006 compared with NHANES III. J Bone Miner Res 25(1):64–71. doi:10.1359/jbmr.090706
Siris ES, Miller PD, Barrett-Connor E, Faulkner KG, Wehren LE, Abbott TA, Berger ML, Santora AC, Sherwood LM (2001) Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA 286(22):2815–2822
Langsetmo L, Goltzman D, Kovacs CS, Adachi JD, Hanley DA, Kreiger N, Josse R, Papaioannou A, Olszynski WP, Jamal SA (2009) Repeat low-trauma fractures occur frequently among men and women who have osteopenic BMD. J Bone Miner Res 24(9):1515–1522. doi:10.1359/jbmr.090319
National Osteoporosis Foundation (2010) Clinician’s guide to prevention and treatment of osteoporosis. National Osteoporosis Foundation, Washington, http://www.nof.org/files/nof/public/content/file/344/upload/159.pdf. Accessed 12 Feb 2013
Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR (2000) Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab 85(11):4118–4124
Cranney A, Tugwell P, Adachi J, Weaver B, Zytaruk N, Papaioannou A, Robinson V, Shea B, Wells G, Guyatt G (2002) Meta-analysis of therapies for postmenopausal osteoporosis. III. Meta-analysis of risedronate for the treatment of postmenopausal osteoporosis. Endocr Rev 23(4):517–523
Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD, Tonino RP, Rodriguez-Portales JA, Downs RW, Gupta J, Santora AC, Liberman UA (2004) Ten years’ experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med 350(12):1189–1199. doi:10.1056/NEJMoa030897
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356(18):1809–1822. doi:10.1056/NEJMoa067312
Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357(18):1799–1809. doi:10.1056/NEJMoa074941
Green JR, Seltenmeyer Y, Jaeggi KA, Widler L (1997) Renal tolerability profile of novel, potent bisphosphonates in two short-term rat models. Pharmacol Toxicol 80(5):225–230
Khosla S, Bilezikian JP, Dempster DW, Lewiecki EM, Miller PD, Neer RM, Recker RR, Shane E, Shoback D, Potts JT (2012) Benefits and risks of bisphosphonate therapy for osteoporosis. J Clin Endocrinol Metab 97(7):2272–2282. doi:10.1210/jc.2012-1027
Miller PD (2011) The kidney and bisphosphonates. Bone 49(1):77–81. doi:10.1016/j.bone.2010.12.024
Sadowski CA, Spencer T, Yuksel N (2011) Use of oral bisphosphonates by older adults with fractures and impaired renal function. Can J Hosp Pharm 64(1):36–41
(2012) Fosamax [package insert]. Whitehouse Station, NJ: Merck and Co., Inc.
Federal Food and Drug Administration (FDA) (2011) FDA Drug Safety Communication: new contraindication and updated warning on kidney impairment for Reclast (zoledronic acid). U.S. Food and Drug Administration, Department of Health and Human Services, Silver Spring, http://www.fda.gov/Drugs/DrugSafety/ucm270199.htm. Accessed 15 May 2012
(2011) Boniva [package insert]. San Francisco, CA: Genentech, Inc.
(2012) Actonel [package insert]. North Norwich, NY: Norwich Pharmaceuticals, Inc.
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2009) National Health and Nutrition Examination Survey (NHANES) 2007–2008 Public Data General Release File Documentation. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/generaldoc_e.htm. Accessed: May 8, 2012
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2005) National Health and Nutrition Examination Survey (NHANES) 2005–2006 Public Data General Release File Documentation. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/general_data_release_doc_05_06.pdf. Accessed: May 8, 2012
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2009) National Health and Nutrition Examination Survey (NHANES): 2005–2006 Data documentation, codebook, and frequencies: dual-energy X-ray absorptiometry—femur bone measurements. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/DXXFEM_D.htm. Accessed 8 May 2012
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2009) National Health and Nutrition Examination Survey (NHANES): 2007–2008 Data documentation, codebook, and frequencies: dual-energy X-ray absorptiometry—femur. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/DXXFEM_E.htm Accessed 8 May 2012
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2010) National Health and Nutrition Examination Survey (NHANES): 2005–2006 Data documentation, codebook, and frequencies: dual-energy X-ray absorptiometry—spine. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/DXXSPN_D.htm. Accessed 8 May 2012
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2010) National Health and Nutrition Examination Survey (NHANES): 2007–2008 Data documentation, codebook, and frequencies: dual-energy X-ray absorptiometry—spine. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/DXXSPN_E.htm. Accessed 8 May 2012
Looker AC, Orwoll ES, Johnston CC Jr, Lindsay RL, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP (1997) Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res 12(11):1761–1768. doi:10.1359/jbmr.1997.12.11.1761
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC Jr, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8(5):468–489
Kelly TJ (1990) Bone mineral density reference databases for American men and women. J Bone Miner Res 5(Suppl 1):S249
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2009) National Health and Nutrition Examination Survey (NHANES): 2007–2008 Data documentation, codebook, and frequencies: urinary albumin and urinary creatinine. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/nhanes/nhanes2007–2008/ALB_CR_E.htm Accessed 15 May 2012
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2007) National Health and Nutrition Examination Survey (NHANES): 2005–2006 Data documentation, codebook, and frequencies: urinary albumin and urinary creatinine. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/nhanes/nhanes2005–2006/ALB_CR_D.htm Accessed 15 May 2012
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G (2003) National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 139(2):137–147
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39 (2 Suppl 1):S1-266
Thorp ML, Eastman L, Smith DH, Johnson ES (2006) Managing the burden of chronic kidney disease. Dis Manag 9(2):115–121. doi:10.1089/dis.2006.9.115
World Health Organization (2011) Global Database on Body Mass Index (BMI): BMI Classification. United Nations. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed 8 May 2012
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2011) Unweighted response rates for National Health and Nutrition Examination Survey (NHANES) 2005–2006 by Age and Gender. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/data/nhanes/response_rates_cps/RRT0506MF.pdf. Accessed 8 May 2012
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2011) Unweighted response rates for National Health and Nutrition Examination Survey (NHANES) 2007–2008 by age and gender. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/data/nhanes/response_rates_cps/RRT0708MF.pdf. Accessed 8 May 2012
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (1996) Analytic and reporting guidelines: the Third National Health and Nutrition Examination Survey, NHANES III (1988–94). U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, http://www.cdc.gov/nchs/data/nhanes/nhanes3/nh3gui.pdf Accessed 8 Nov 2013
Miller PD (2007) Is there a role for bisphosphonates in chronic kidney disease? Semin Dial 20(3):186–190. doi:10.1111/j.1525-139X.2007.00271.x
Jamal SA, Bauer DC, Ensrud KE, Cauley JA, Hochberg M, Ishani A, Cummings SR (2007) Alendronate treatment in women with normal to severely impaired renal function: an analysis of the fracture intervention trial. J Bone Miner Res 22(4):503–508. doi:10.1359/jbmr.070112
Miller PD, Roux C, Boonen S, Barton IP, Dunlap LE, Burgio DE (2005) Safety and efficacy of risedronate in patients with age-related reduced renal function as estimated by the Cockcroft and Gault method: a pooled analysis of nine clinical trials. J Bone Miner Res 20(12):2105–2115. doi:10.1359/jbmr.050817
Boonen S, Sellmeyer DE, Lippuner K, Orlov-Morozov A, Abrams K, Mesenbrink P, Eriksen EF, Miller PD (2008) Renal safety of annual zoledronic acid infusions in osteoporotic postmenopausal women. Kidney Int 74(5):641–648. doi:10.1038/ki.2008.193
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2:138
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group (2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl (113):S1-130. doi:10.1038/ki.2009.188
Miller PD, Jamal SA, Evenepoel P, Eastell R, Boonen S (2013) Renal safety in patients treated with bisphosphonates for osteoporosis: a review. J Bone Miner Res 28(10):2049–2059. doi:10.1002/jbmr.2058
Tanko LB, Qin G, Alexandersen P, Bagger YZ, Christiansen C (2005) Effective doses of ibandronate do not influence the 3 years progression of aortic calcification in elderly osteoporotic women. Osteoporos Int 16(2):184–190. doi:10.1007/s00198-004-1662-x
Hill JA, Goldin JG, Gjertson D, Emerick AM, Greaser LD, Yoon HC, Khorrami S, Aziz D, Adams JS (2002) Progression of coronary artery calcification in patients taking alendronate for osteoporosis. Acad Radiol 9(10):1148–1152
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361(8):756–765. doi:10.1056/NEJMoa0809493
Centers for Disease Control and Prevention (2007) Prevalence of chronic kidney disease and associated risk factors—United States, 1999–2004. MMWR Morb Mortal Wkly Rep 56 (8):161–165
Whaley-Connell AT, Sowers JR, Stevens LA, McFarlane SI, Shlipak MG, Norris KC, Chen SC, Qiu Y, Wang C, Li S, Vassalotti JA, Collins AJ (2008) CKD in the United States: Kidney Early Evaluation Program (KEEP) and National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis 51(4 Suppl 2):S13–20. doi:10.1053/j.ajkd.2007.12.016
Zimmerman SI, Girman CJ, Buie VC, Chandler J, Hawkes W, Martin A, Holder L, Hebel JR, Sloane PD, Magaziner J (1999) The prevalence of osteoporosis in nursing home residents. Osteoporos Int 9(2):151–157
Center for Drug Evaluation and Research (CDER) (2010) Guidance for industry: Pharmacokinetics in patients with impaired renal function—study design, data analysis, and impact on dosing and labeling. U.S. Food and Drug Administration, Department of Health and Human Services, Silver Spring, http://www.fda.gov/Drugs/DrugSafety/ucm270199.htm. Accessed 24 May 2013
Acknowledgements
None.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lubwama, R., Nguyen, A., Modi, A. et al. Prevalence of renal impairment among osteoporotic women in the USA, NHANES 2005–2008: Is treatment with bisphosphonates an option?. Osteoporos Int 25, 1607–1615 (2014). https://doi.org/10.1007/s00198-014-2645-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2645-1