Abstract
Summary
This study evaluated bone health in adults with galactosemia. Associations between bone mineral density (BMD) and nutritional and biochemical variables were explored. Calcium level predicted hip and spine BMD, and gonadotropin levels were inversely associated with spinal BMD in women. These results afford insights into management strategies for these patients.
Introduction
Bone loss is a complication of galactosemia. Dietary restriction, primary ovarian insufficiency in women, and disease-related alterations of bone metabolism may contribute. This study examined relationships between clinical factors and BMD in patients with galactosemia.
Methods
This cross-sectional sample included 33 adults (16 women) with classic galactosemia, mean age 32.0 ± 11.8 years. BMD was measured by dual-energy X-ray absorptiometry, and was correlated with age, height, weight, fractures, nutritional factors, hormonal status, and bone biomarkers.
Results
There was a significant difference in hip BMD between women and men (0.799 vs. 0.896 g/cm2, p = 0.014). The percentage of subjects with BMD-Z <−2.0 was also greater for women than men [33 vs. 18 % (spine), 27 vs. 6 % (hip)], and more women reported sustaining fractures. Bivariate analyses yielded correlations between BMI and BMD-Z [at the hip in women (r = 0.58, p < 0.05) and spine in men (r = 0.53, p < 0.05)]. In women, weight was also correlated with BMD-Z (r = 0.57, p < 0.05 at hip), and C-telopeptides (r = −0.59 at spine and −0.63 hip, p < 0.05) and osteocalcin (r = −0.71 at spine and −0.72 hip, p < 0.05) were inversely correlated with BMD-Z. In final regression models, higher gonadotropin levels were associated with lower spinal BMD in women (p = 0.017); serum calcium was a significant predictor of hip (p = 0.014) and spine (p = 0.013) BMD in both sexes.
Conclusions
Bone density in adults with galactosemia is low, indicating the potential for increased fracture risk, the etiology of which appears to be multifactorial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Classic galactosemia is an autosomal recessive disorder resulting in a deficiency of the galactose-1-phosphate uridyltransferase (GALT) enzyme, which converts galactose-1-phosphate to uridine diphosphate-galactose [1, 2]. GALT deficiency leads to an accumulation of galactose-1-phosphate, resulting in increased production of galactitol and galactonate, metabolites that may have adverse effects on the ovaries and bone, among other tissues [1–12].
Classic galactosemia occurs in approximately 1 per 40,000–50,000 Caucasian newborns [1, 2]. Neonatal complications associated with untreated disease include: feeding difficulties, jaundice, vomiting, diarrhea, hepatomegaly, renal tubular dysfunction, muscle hypotonia, cataracts, and sepsis, accompanied by a high mortality rate [1, 2]. Treatment with a lactose-restricted diet, which is the only current therapy for these patients, can reverse these acute neonatal manifestations [2]. However, long-term complications include intellectual disability, verbal dyspraxia, motor abnormalities, primary ovarian insufficiency (previously known as premature ovarian failure) in adolescent girls and women, as well as bone mineralization and body composition abnormalities. These disease sequelae can be seen, although not all complications are seen in all patients, despite adherence to a lactose-restricted diet [8, 9].
The pathophysiologic mechanisms underlying skeletal losses in patients with classic galactosemia are not well understood. However, several have been proposed, including nutritional deficiencies, alterations in the endocrine axis, and intrinsic factors related to bone metabolism, all which may contribute to bone loss in this patient group. The necessary lifelong lactose-restricted diet to which these patients must adhere is a primary risk factor for bone loss and/or inadequate accrual. Galactose is a monosaccharide found in lactose. Therefore the lactose-restricted diet is devoid of vitamin D-fortified milk and dairy products. These restrictions may then lead to low calcium and vitamin D intake unless an individual is properly supplemented [4, 6]. Several studies have cited primary ovarian insufficiency in women with galactosemia as a contributing factor to low bone mineral density (BMD) [10–12]. Patients with this disease may also exhibit abnormal collagen formation as a result of deficient galactose residues needed for normal bone formation and mineralization processes [12]. This theory is further supported by a study showing that in a group of patients with galactosemia, which included females receiving estrogen replacement therapy, calcium supplementation was able to improve, but not normalize, bone density [12]. These data suggest that other intrinsic abnormalities in bone and mineral metabolism may be involved.
While previous bone-related studies have evaluated children with galactosemia, there is little information regarding the long-term consequences of this disease during adulthood. The present study evaluated adult patients with galactosemia who were diagnosed during infancy. We aimed to evaluate skeletal outcomes in a group of adults with this disease, to add to the sparse data that currently exist. The second aim of the study was to examine clinical variables within this patient group that correlated with bone density and predicted skeletal outcomes.
Methods
Subjects
Thirty-three adult patients (16 women) with classic galactosemia (age 32.0 + 11.8 years) were enrolled into a cross-sectional study. The subjects were recruited via newsletter announcements sent to patients and their families through the Galactosemia Foundation. Participants traveled to Boston from throughout the USA and Europe to participate in multiple assessments over a single weekend in the Children’s Hospital Boston Clinical and Translational Study Unit. All were diagnosed during early infancy and placed on a lactose-restricted diet. Only a minority of individuals were detected by newborn screening. The diagnosis in all participants was confirmed by a severely deficient or absent erythrocyte GALT enzyme activity, and a GALT gene mutation analysis. The protocol was approved by the Committee on Clinical Investigation at Children’s Hospital Boston, and each participant gave informed consent at the time of study enrollment.
BMD measures
Participants underwent measurements of BMD by dual-energy X-ray absorptiometry (DXA) at the hip and lumbar (L1–L4) spine using a Hologic Discovery A scanner (Hologic Inc., Bedford, MA). The results were expressed as areal BMD in grams per square centimeter. These data were used to generate BMD Z-scores (BMD-Z) as recommended for this age group by the International Society for Clinical Densitometry [13, 14], which were calculated using age-, gender-, and ethnicity-specific software [15, 16]. BMD data were correlated with clinical and environmental variables including age, height, weight, nutritional and hormonal status, and bone biomarkers. Additionally, information regarding fractures was obtained from follow-up phone conversations with participants (made by LAB and CMG).
Biochemical measures
Serum LH, FSH, and E2 were measured using direct immunoassays (Architect i2000; Abbott Laboratories, Abbott Park, IL) [17]. LH and FSH are expressed in international units per liter, as equivalents of the International Pituitary Standard for LH 80/552 and FSH 92/510. Laboratory measures included serum 25-hydroxyvitamin D (immunochemiluminometric assay, DiaSorin LIAISON®), and plasma calcium and phosphorus concentrations.
Nutritional measures
Study participants were weighed and measured, and body mass index (BMI) was calculated. All participants were interviewed by a nutritionist regarding diet history, foods avoided, and the type and frequency of vitamin and mineral supplementation. Three-day food records were sent to participants and completed prior to the study visit; subjects who did not complete records reported a 24-h recall/typical daily intake. Dietary intake data were analyzed using the Nutrition Data System for Research (NDSR, University of Minnesota). Nutrient intake from food records was obtained for 11 participants and 1-day intake based on 24-h recall for 22 participants. Intakes are reported with and without vitamin D and calcium supplementation. Fourteen participants reported supplement intake, but could not specify the amount or frequency, or did not answer the question; these were counted as zero in calculating total intake. Multivitamin intake was not included; therefore, dietary intakes are underestimated by an unknown amount in about 25 % of cases.
Bone biomarkers
Biomarkers of bone formation, serum levels of osteocalcin and bone-specific alkaline phosphatase (BSAP), were measured in study participants. Osteocalcin was measured by double-antibody RIA (%CV 11–13 %), and immunoradiometric assay (IRMA) was used to measure BSAP (%CV 5.2–5.6 %; Esoterix Inc. Laboratory Services, Calabasas Hills, CA). Serum C-telopeptide (CTx) levels (surrogate markers of bone resorption) were measured using an IRMA (%CV 5.2–6.8 %; Immunodiagnostic Systems, Fountain Hills, AZ).
Fractures
Study participants were mailed a letter requesting permission to be contacted with additional questions related to their bone health. If a subject did not return an opt-out card within 2 weeks, they were asked the following: Have you broken any bones in your life? If so, how many? What were you doing when you broke the bone?
Statistical analysis
Continuous measures were compared between sexes by Student’s independent t test, corroborated or replaced by Wilcoxon’s two-sample test in cases of skewed distribution. Dichotomies were compared by Fisher’s exact test. Mean BMD-Z at each skeletal site was compared with the normal reference of Z = 0 by Student’s one-sample t test. Pearson’s correlation coefficient was used to assess the bivariate associations between bone mineral density and each of the anthropometric measures, nutrient intakes, and serum levels of vitamin D, minerals, hormones, and bone markers. Multiple regression models were constructed to determine the joint influence of those variables on BMD, accounting for confounding variables. Interaction terms were added to the model to account for sex differences in the effects of covariates. Statistical significance was taken as p < 0.05. SAS version 9.2 (Cary, NC, 2008) was used for all computations.
Results
Anthropometric and clinical measures
Characteristics of the sample are detailed in Table 1. The mean age was just over 30 years in both sexes. Men were significantly taller on average, by 8.7 cm, but the sexes did not differ as to weight or BMI. The percentages of subjects in each of the BMI categories were: underweight 6 %, normal weight 58 %, overweight 24 %, and obese 12 %. The women reported higher vitamin D and calcium supplement intake. Serum hormones and bone biomarkers did not differ by sex (Table 2). Vitamin D deficiency, defined as total 25-hydroxyvitamin D (25(OH)D) in serum less than 20 ng/mL, was not different between women and men: 2 out of 16 (13 %) vs. 5 out of 17 (29 %), respectively; p = not significant (NS). Similarly, there was no difference in the prevalence of vitamin D insufficiency (serum 25(OH)D 21–30 mg/mL) in women vs. men [9 out of 16 (56 %) vs. 6 out of 17 (35 %), respectively; p = NS]. As expected, FSH and LH levels were elevated in women.
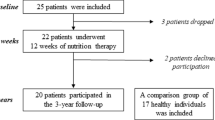
Bone measures
The distribution of BMD-Z is shown in Fig. 1. In both sexes at each skeletal site, the majority of the measurements fell below Z = 0, with the mean Z-score significantly below 0. As detailed in Table 1, the absolute BMD was lower on average in women than in men, both at the spine (0.903 vs. 0.991 g/cm2, p = 0.06) and at the hip (0.799 vs. 0.896 g/cm2, p = 0.014).
Histograms illustrating the distribution of BMD in 33 adults with classical galactosemia. The majority of women (upper panels) as well as men (lower panels) fell below normal BMD for sex and age, both at the spine (left) and at the hip (right). Dashed line indicates the sex- and age-specific population mean, BMD-Z = 0. The arrows indicate the sample mean BMD-Z, falling significantly below zero in each case as indicated by the 95 % confidence interval (crossbar) and the displayed p value
The percentage of subjects with BMD-Z under −2.0 was greater for women than men (33 vs. 18 % at the spine, 27 vs. 6 % at the hip), and a greater percentage of women reported a history of fractures (Table 1). Interview data revealed that 63 % of the women and 31 % of men had sustained at least one lifetime fracture. For these dichotomous outcomes, the sample size was too small to determine statistical significance.
Correlates of bone mineral density
Bivariate associations between BMD-Z at the spine and hip and each of the anthropometric measures, nutrient intakes, vitamin and mineral levels, hormones, and bone markers are detailed by sex in Table 3. Body weight and BMI showed moderate correlations with BMD-Z at the hip in women, and BMI was moderately correlated with BMD-Z at the spine in men. Calcium intake was correlated with lumbar spine BMD in women only. None of the other nutrient intakes, serum vitamin D or calcium levels, or hormonal concentrations showed notable correlations with BMD-Z at either site in men or women. Two of the bone markers, CTx and osteocalcin, showed a moderate and significant inverse correlation with BMD-Z at both sites in women. Similar correlations (not tabulated) were seen for absolute BMD, with the additional finding that serum calcium was moderately correlated with hip BMD in both women (r = 0.54, p = 0.03) and men (r = 0.49, p = 0.04).
Multivariable models
Results of multiple regression modeling are displayed in Table 4. Each model included adjustment for sex, age, and weight; height was omitted from multivariable modeling because of its colinearity with sex. Serum calcium level was consistently associated with BMD in the multivariable models. An increment of 1 mg/dL in serum calcium was associated with a benefit of 0.16–0.18 g/cm2 at the lumbar spine and 0.14–0.16 g/cm2 at the hip. The magnitude of effect was not attenuated by adjustment for other predictors and did not differ by sex (p > 0.50).
In women only, osteocalcin levels demonstrated an inverse association with BMD, independent of the calcium effect (model I). The gonadotropins (LH in model II, FSH in model III) also showed significant inverse associations with BMD at the spine and weaker nonsignificant effects on BMD at the hip. In models including both LH and FSH (not shown), the strong correlation between the two gonadotropins (Pearson r = 0.93) resulted in neither showing an independent influence on BMD. As detailed in Table 4, adjustment for the gonadotropins attenuated but did not abolish the osteocalcin effect at both skeletal sites.
The sex differences in BMD and the associations with body weight, evident in bivariate analyses (Tables 1 and 2), were attenuated and nonsignificant in the multivariable models. Dietary intake of calcium and vitamin D did not contribute significantly when tested in multivariable modeling, nor did the serum levels of 25(OH)D, phosphorus, bone markers, or hormones other than the osteocalcin and gonadotropin effects noted above. Multiple logistic regression modeling, using the dichotomized BMD Z-scores as outcome, was unsuccessful owing to the small sample size and consequent numerical instability of the model-fitting procedure.
Discussion
The current study evaluated bone density and skeletal turnover in adult patients with galactosemia and adds to the small fund of knowledge that currently exists regarding bone deficits in patients with this rare disorder. We sought both to determine how many patients exhibited skeletal deficits and to explore mechanisms of bone loss in these patients. Our data suggest that low bone density is a frequent finding in adult patients with classic galactosemia, confirming results from previous studies [5–7, 11, 12] and highlighting the point that its etiology is multifactorial. In final regression models, circulating calcium level was a predictor of hip and spine BMD in both sexes, and osteocalcin and gonadotropin levels were inversely correlated with spinal BMD in the women studied. To our knowledge, this is the first study to examine simultaneously clinical variables that contribute to bone loss in adults with this disease.
Fracture data revealed that a relatively large percentage of the study subjects had sustained at least one lifetime fracture, including over half of the women and almost one third of the men. To our knowledge, this is the only study to date that has sought to compare bone density measurements with fracture rates in this patient population. Fracture incidence is a difficult measure to quantify. Noteworthy is the fact that in healthy cohorts, one third to one half of all children and adolescents will sustain at least one fracture by the end of their teenage years [18–20]. However, adults with galactosemia are not typically athletic, and can be socially withdrawn, and exhibit overt signs of motor impairment [1, 2]. Therefore, the mechanism of fracture in these patients may be different than that observed in a healthy control population. Data from this small sample of young adults suggest that patients with galactosemia, especially women, may be at increased risk for fracture.
While the relationship between body weight and BMD was attenuated in the multivariable regression models, weight showed a significant correlation to BMD in bivariate analyses. Specifically, body weight and BMI were moderately correlated with BMD-Z at the hip in women, a weight-bearing site, and BMI was correlated with BMD-Z at the spine in men. The associations noted in the bivariate analyses deserve mention given that this disease involves dietary, although not caloric, restriction. These results highlight the importance of providing appropriate nutritional counseling to these patients to optimize not only calcium and vitamin D intake but also to meet their general caloric requirements. Yet, 90 % of the subjects reported that they did not currently see a nutritionist. These data suggest that the frequency of visits with a nutritionist may decrease as these patients enter adulthood. Lastly, dietary advice is needed for maintenance of an ideal body weight and potentially as a strategy to optimize bone accrual during adolescence and maintain bone mass during the adult years.
Also noteworthy is the fact that the skeletal deficits found in these patients were not uniform throughout the skeleton. A higher percentage of patients exhibited BMD Z-scores ≤−2.0 at the spine than the hip. The spine is composed primarily of trabecular bone in contrast to the hip, the latter of which is comprised primarily of cortical bone [21]. Trabecular bone is more hormonally responsive than cortical bone, and trabecular losses are seen commonly in other chronic illnesses associated with malnutrition such as anorexia nervosa [22]. Therefore, it was expected that skeletal deficits would be greater at the spine than hip, as was seen in this study. While the current study subjects were not underweight like patients with anorexia nervosa, the similar pattern of regional bone loss is interesting to consider. Also of note was the fact that osteocalcin and CTx levels, each representing surrogate markers of bone turnover, were inversely correlated with bone density at both the hip and spine in the women studied. These data suggest that skeletal losses in women with this disease reflect a high bone turnover state and that specific regions of the skeleton are most responsive to hormonal signals. The inverse correlation between osteocalcin and BMD in the women at both skeletal sites is especially intriguing and merits further study. Recently, there has been high interest in the multiple roles of osteocalcin, including its role in bone mineralization and calcium homeostasis, as well as that of a metabolic regulator [23]. Given the strength of the association noted in the women only, further work should address the role of osteocalcin in this metabolic disorder and whether osteocalcin may be facilitating “cross talk” between skeletal remodeling and energy metabolism.
To our surprise, there was no significant correlation found between age and bone density. Previous literature, however, has shown that even children with galactosemia may exhibit skeletal deficits [11]. Therefore, we expected to see an inverse correlation between BMD with age. A longitudinal study in these patients, beginning in childhood, to follow bone density as well as fracture rate and markers of skeletal strength would be more informative in understanding patterns of bone accretion. These longitudinal data will also be needed to confirm both the incidence of low bone mass during adulthood in this clinical model and the variables that mediate bone loss. The dimorphic pattern of bone loss, with a higher prevalence of low BMD and fractures in the women vs. men, and unique variables emerging that predict bone loss in each sex, merits careful attention in future studies. The skewing of the data in the women vs. men may reflect varying estrogen replacement regimens and is a hypothesis to investigate in future studies.
Another surprising finding was that there was no correlation noted between bone density and estradiol concentrations in the women with galactosemia. In the general population, it has been documented that low estradiol concentrations are a risk factor for osteoporosis [24]. It was expected, therefore, that the women in this study with lower BMD values would have corresponding lower estradiol levels. Complicating the analysis were the variable types of hormone replacement used in the study, some of which would not be measured in an estradiol assay, such as ethinyl estradiol in birth control pills. Nevertheless, the inverse correlation noted between gonadotropin levels and spinal BMD in the women studied may be revealing. Perhaps lower dose or inadequate hormone replacement therapy for primary ovarian insufficiency, which would result in higher gonadotropin levels, may be inadequate. It is possible that higher dose estrogen replacement, such as in the form of contraceptives, may be needed to protect bone in these women. Another possible explanation for this finding is that women with significant primary ovarian insufficiency and significant bone loss were more likely to be detected clinically and subsequently placed on estrogen replacement therapy, obscuring the relationship between circulating estradiol and skeletal endpoints. Because of the small sample size, a common situation when studying a rare disorder, we were not able to analyze subgroups of treated vs. untreated patients. Further study of the initiation and dose of estrogen replacement is needed as it appears to have implications for optimizing care in women with this disease.
One patient who was excluded from our final data analysis merits discussion. She showed partially preserved function of the GALT enzyme and is therefore different from other patients in the sample. She had been managed clinically from infancy with a lactose-restricted diet like the other patients in this study with classic galactosemia, yet her BMD at both the hip and the spine were in the normal range. She also had normal ovarian function. This case example emphasizes the point that the decreased BMD seen in patients with classic galactosemia is not only the result of dietary restriction; other intrinsic and extrinsic factors associated with this metabolic disorder may contribute to this phenomenon.
From an intervention standpoint, it is also important to discuss our findings related to calcium and vitamin D in this group. There was a statistically significant difference in calcium supplement intake in the male vs. female participants. Given that males with galactosemia also represent a high-risk group for low BMD, healthcare providers need to encourage maximizing calcium intake among both male and female patients with this disease as a way to optimize calcium status, which we ultimately showed using multiple regression to be correlated with higher BMD measures. With regard to vitamin D status, 13 % of the females and 29 % of the males in this study had serum 25-hydroxyvitamin D levels <20 ng/mL, placing them in the vitamin D-deficient range [25, 26]. The explanation for this difference in prevalence is unclear, but may reflect less consistent compliance with supplementation regimens or monitoring by a dietician, especially among the male participants. Improved monitoring of vitamin D status and appropriate supplementation in this patient population hold promise to improve skeletal outcomes in this patient population. While dietary intake of calcium and vitamin D did not affirmatively lead to BMD improvement, circulating calcium level was a significant predictor of BMD in both the men and women studied. Thus, efforts to encourage strategies to improve dietary intake of calcium and vitamin D, and appropriate supplementation of these nutrients to maintain a normal calcium concentration may ultimately lead to improved bone health for these patients.
Our study had several limitations that should be acknowledged. First, the sample size was unavoidably small due to the fact that classic galactosemia is a rare autosomal recessive disorder; therefore, the current results must be considered preliminary. Second, as mentioned, this study utilized a cross-sectional sample of adult patients, and thus, it was not possible to comment on cause and effect relationships between the observed correlations between clinical variables and bone density measures. Some of the data, including the patient histories related to fracture, diet, and nutritional intake, were obtained by self-report which has its inherent limitations. In addition, there were missing data for some of the nutritional outcomes, and sparse data related to the amount or frequency of consumption of some nutrients. The exclusion of multivitamin intake is also problematic as dietary intakes are likely underestimated in 25 % of the participants. We acknowledge each of these points as a major limitation that could have affected the data reported on nutrition. The fact that serum calcium was positively correlated with BMD, while calcium intake was not, is an example of discrepancies that were potentially introduced by some of the missing data. Information was also lacking on the type of fracture (i.e., vertebral or long bone) which would have afforded insight into the correlation between BMD and fracture type in this patient group. Information on whether fractures were atraumatic or not will be important to obtain in future studies. Detailed information on the participants’ estrogen replacement regimens was lacking, including age of onset and duration of therapy. These data will be important to collect in future studies, to understand the role of estrogen deficiency in the skeletal deficits observed in women with this disease. Finally, the bone density measurements were obtained by DXA, which provides a two-dimensional measure of a three-dimensional structure, and may introduce measurement error [9].
Overall, the current data suggest that children with classic galactosemia represent a risk group for low bone mass in adulthood and that these deficits occur despite adherence to a galactose-restricted diet. It is the hope that the factors that we have identified related to bone health in this adult population may lead to early intervention with treatment modifications for patients with galactosemia. Ideally, interventions would start during childhood to promote optimal bone accrual and thereby improve lifetime bone health for this high-risk group.
References
Holton JB, Walter JH, Tyfield LA (2001) Galactosemia. In: Scriver CR, Childs B (eds) The metabolic and molecular bases of inherited disease. McGraw-Hill, New York
Fridovich-Keil JL, Walter JH (2011) Galactosemia. In: Valle D, Beaudet AL, Vogelstein B, Kinzler BW, Antonarakis SE, Ballabio (eds) Scriver C, Sly WS, Childs B (eds emeriti). The On-line Metabolic and Molecular Bases of Inherited Disease (OMMBID). http://www.ommbid.com/. Accessed October 2011
Panis B, Forget PP, Nieman FH, van Kroonenburgh MJ, Rubio-Gozalbo ME (2005) Body composition in children with galactosaemia. J Inherit Metab Dis 28:931–937
Bosch AM (2006) Classical galactosaemia revisited. J Inherit Metab Dis 29:516–525
Panis B, Forget PP, van Kroonenburgh MJ, Vermeer C, Menheere PP, Nieman FH, Rubio-Gozalbo ME (2004) Bone metabolism in galactosemia. Bone 35:982–987
Panis B, Vermeer C, van Kroonenburgh MJ, Nieman FH, Menheere PP, Spaapen LJ, Rubio-Gozalbo ME (2006) Effect of calcium, vitamins K1 and D3 on bone in galactosemia. Bone 39:1123–1129
Gajewska J, Ambroszkiewicz J, Radomyska B, Chelchowska M, Oltarzewski M, Laskowska-Klita T, Milanowski A (2008) Serum markers of bone turnover in children and adolescents with classic galactosemia. Adv Med Sci 53:214–220
Waggoner DD, Buist NR, Donnell GN (1990) Long-term prognosis in galactosaemia: results of a survey of 350 cases. J Inherit Metab Dis 13:802–818
Schweitzer S, Shin Y, Jakobs C, Brodehl J (1993) Long-term outcome in 134 patients with galactosaemia. Eur J Pediatr 152:36–43
Fridovich-Keil JL, Gubbels CS, Spencer JB, Sanders RD, Rubio-Gozalbo E (2011) Ovarian function in girls and women with GALT-deficiency galactosemia. J Inherit Metab Dis 34:357–66
Rubio-Gozalbo ME, Hamming S, van Kroonenburgh MJ, Bakker JA, Vermeer C, Forget PP (2002) Bone mineral density in patients with classic galactosaemia. Arch Dis Child 87:57–60
Kaufman FR, Loro ML, Azen C, Wenz E, Gilsanz V (1993) Effect of hypogonadism and deficient calcium intake on bone density in patients with galactosemia. J Pediatr 123:365–370
Binkley TL, Berry R, Specker BL (2008) Methods for measurement of pediatric bone. Rev Endocr Metab Disord 9:95–106
Carey JJ, Delaney MF, Love TE, Cromer BA, Miller PD, Richmond BJ, Manilla-McIntosh M, Lewis SA, Thomas CL, Licata AA (2009) Dual-energy X-ray absorptiometry diagnostic discordance between T-scores and Z-scores in young adults. J Clin Densitom 12:11–6
Kelly TL (1990) Bone mineral density reference databases for American men and women. J Bone Miner Res 5:S249
Looker AC, Wahner HW, Dunn WL et al (1995) Proximal femur bone mineral levels of US adults. Osteoporos Int 5:389–409
Sluss PM, Hayes FJ, Adams JM, Barnes W, Williams G, Frost S, Ramp J, Pacenti D, Lehotay DC, George S, Ramsay C, Doss RC, Crowley WF Jr (2008) Mass spectrometric and physiological validation of a sensitive, automated, direct immunoassay for serum estradiol using the Architect. Clin Chim Acta 388:99–105
Khosla S, Melton LJ III, Dekutoski MB, Achenbach SJ, Oberg AL, Riggs BL (2003) Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA 290:1479–85
Landin LA (1983) Fracture patterns in children analysis of 8682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950–1979. Acta Orthop Scand Suppl 202:1–109
Jones IE, Williams SM, Dow N et al (2002) How many children remain fracture free during growth? A longitudinal study of children and adolescents participating in the Dunedin multidisciplinary health and development study. Osteoporos Int 13:990–995
Mosekilde L, Ebbesen EN, Tornvig L, Thomsen JS (2000) Trabecular bone structure and strength—remodeling and repair. J Musculoskel Neuron Interact 1:25–30
DiVasta AD, Feldman HA, Quach AE, Balestrino M, Gordon CM (2009) The effect of bed rest on bone turnover in young women hospitalized for anorexia nervosa: a pilot study. J Clin Endocrinol Metab 94:1650–5
Ducy P (2011) The role of osteocalcin in the endocrine cross-talk between bone remodeling and energy metabolism. Diabetologia 54:1291–1297
Shulman LP (2008) Transdermal hormone therapy and bone health. Clin Interv Aging 3:51–54
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM, Endocrine Society (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–30
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, Kovacs CS, Mayne ST, Rosen CJ, Shapses SA (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 96:53–8
Acknowledgments
The authors gratefully acknowledge all of the study participants and their families who made this study possible. We also thank Jamie Nydegger, CDT and Yailka Cardenas, CDT for the excellent technical assistance (Bone Health Program, Children’s Hospital Boston) and Nicolle Quinn, MS RD (research dietitian, Clinical and Translational Study Unit, Children’s Hospital Boston) for performing the food record analyses. This project was funded by the Galactosemia Foundation.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Batey, L.A., Welt, C.K., Rohr, F. et al. Skeletal health in adult patients with classic galactosemia. Osteoporos Int 24, 501–509 (2013). https://doi.org/10.1007/s00198-012-1983-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-1983-0