Abstract
Decreased bone mass is frequently encountered in classic galactosemia, an inborn error of galactose metabolism. This decrease is most prominent in adults, but is already seen in prepubertal children with increased risk of osteoporosis and fractures later in life. Therefore, bone health in patients with classic galactosemia is increasingly monitored. Although the pathophysiological mechanism is still not fully understood, several factors could negatively affect bone metabolism in this disease. Patients are at risk of nutritional deficiencies due to the galactose-restricted diet. Primary ovarian insufficiency (POI) in female patients also contributes to decreased bone mass. Furthermore, patients with classic galactosemia might be less physically active due to motor or neurological impairments. A disease-specific intrinsic abnormality has been suggested as well. This revised proposal is an update of the 2007 recommendations. In this current approach, we advise comprehensive dietary evaluation, optimization of calcium intake if needed, monitoring and if necessary supplementation of vitamin D, hormonal status evaluation and hormone replacement therapy (HRT) consideration, as well as a regular exercise and assessment of skeletal deformities and clinically significant fractures. We propose bone mineral density (BMD) assessment by serial DXA scans of the lumbar spine, femoral neck, and total hip in adults and lumbar spine and total body less head (TBLH) in children.
Competing interests: None declared
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Decreased bone mass is frequently encountered in classic galactosemia (OMIM 230400), an inborn error of galactose metabolism (Kaufman et al. 1993; Rubio-Gozalbo et al. 2002; Panis et al. 2004; Jumbo-Lucioni et al. 2012; Waisbren et al. 2012; Batey et al. 2013; Coss et al. 2013). This decrease in bone mass is most prominent in adults, but is already seen in prepubertal children (Kaufman et al. 1993; Rubio-Gozalbo et al. 2002; Panis et al. 2004). Since bone mass increases quickly during puberty and reaches its peak at the end of adolescence or early adulthood, a low bone mass at an early age predisposes to osteoporosis and an increased risk of fractures later in life (Eisman 1999). Therefore, bone health in patients with classic galactosemia is increasingly monitored.
Scarce data are available with regard to reduced bone mass and its clinical relevance in this patient population. The average reported bone mineral density (BMD) as assessed by dual-energy X-ray absorptiometry (DXA) in adults with galactosemia is more than one standard deviation (SD) below the mean, and even about 25–30% of patients have a BMD more than 2 SD below the mean (Waisbren et al. 2012; Batey et al. 2013), whereas in pediatric patients with galactosemia, the average is between 0 and −1 SD (Rubio-Gozalbo et al. 2002; Panis et al. 2004). Fracture rates in adult patients with classic galactosemia have been reported between 31 and 63% (Waisbren et al. 2012; Batey et al. 2013), which is slightly higher than in the general population in which rates between 21 and 53% have been reported for this age category (van Staa et al. 2001). Only one study addresses the fracture rates in pediatric patients (Waisbren et al. 2012), and the reported prevalence of 18% is not higher than in the healthy pediatric population (Landin 1997).
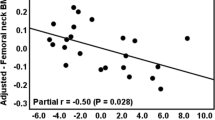
Although the pathophysiological mechanism is still not fully understood, several factors could negatively affect bone metabolism in this disease. Due to the galactose-restricted diet, patients are at risk of developing nutritional deficiencies. The primary ovarian insufficiency (POI) with low estradiol levels in females with galactosemia predisposes affected females to decreased bone mass. A disease-specific intrinsic abnormality such as abnormal glycosylation of collagen or other glycoproteins involved in bone metabolism has also been suggested (Kaufman et al. 1993). Furthermore, the decreased IGF-I and IGFBP-3 concentrations that are found in galactosemia patients might be involved (Panis et al. 2007a).
For classic galactosemia, optimization of exogenous factors influencing the bone mass is considered the most important intervention. The latest recommendations regarding follow-up and treatment of reduced bone mass in this disease date from 2007 (Panis et al. 2007b). Since then, insights regarding different aspects of bone health have increased, and there is a need to update and expand the previous recommendations based on our experience and the current literature. This proposal shortly reviews the diagnostic procedure and recommendations for follow-up including DXA, dietary evaluation, biochemical markers, physical activity, and in females supplementation of estrogen.
Diagnostic Procedures
Dietary Evaluation and Bone Metabolism Markers
A balanced diet sufficient in energy, protein, and micronutrients is a criterion for achieving and maintaining a high bone mass. Recently, it has been shown that body weight and body mass index (BMI) correlate with bone mass in patients with classic galactosemia, emphasizing the need for monitoring caloric intake in this group (Batey et al. 2013). Evaluation of food records or food frequency questionnaires, preferably by a nutritionist, can be used to determine a patient’s general nutrition status and to assess the completeness of a patient’s diet.
The galactose-restricted diet predisposes patients to nutritional deficiencies, including a calcium deficiency. Dietary calcium intake therefore needs to be monitored, as is also recommended for other metabolic diseases in which the bone health is often affected. The recommended daily dietary calcium intake, which varies slightly per country, can be used as reference (Table 1).
Adequate vitamin D status, assessed by dietary and laboratory evaluation, is also required for optimal bone health. The preferred marker for vitamin D status is the total 25-hydroxyvitamin D (25(OH)D) serum concentration. Measurement of 1,25(OH)2D is not recommended, since these concentrations do not reflect vitamin D reserves and can even be normal or elevated in patients with vitamin D deficiency due to secondary hyperparathyroidism (Holick et al. 2011). It is advised to aim for a total 25(OH)D serum concentration higher than 30 ng/mL (75 nmol/L) in patients at risk of developing osteoporosis, and this requires a vitamin D intake of at least 400–1,000 IU/day (Holick et al. 2011) (Table 1).
The importance of vitamin K in acquiring adequate bone mass remains controversial. Several studies, including one study in patients with classic galactosemia, have reported that supplementation positively affects bone mass when combined with calcium and vitamin D. Panis et al. (2006) showed that supplementation of vitamin K increased the concentration of carboxylated osteocalcin, which is required for the incorporation of calcium and hydroxyapatite in the bone. Braam et al. (2003) found a slower bone loss in postmenopausal women receiving vitamin K in combination with calcium and vitamin D. However, there is also evidence that vitamin K does not increase bone mass (Guralp and Erel 2014).
Other nutrients that might be important for bone metabolism include zinc, phosphorus, and magnesium. There have been concerns that soy formula might have a negative effect on bone metabolism and growth due to its high phytate content, which causes reduced absorption of zinc. However, in a recent meta-analysis, zinc serum concentrations were found to be similar in children who were fed soy infant formula during infancy compared to children fed human milk or cows’ milk-based formula during infancy (Vandenplas et al. 2014). Therefore, soy-feeding-related zinc deficiency is unlikely and measuring zinc concentrations is not recommended. Deficiencies of phosphorus and magnesium are unlikely in a balanced diet, and therefore, routine monitoring is not advised for patients at risk of developing low bone mass. However, serum phosphate and serum magnesium require special attention when dietary assessment indicates an insufficient diet. Furthermore, there is some evidence that a high phosphorus intake, resulting from food additives, combined with a low or normal calcium intake may have adverse effects on bone metabolism due to a disturbed ratio of calcium-to-phosphorus intake (Calvo and Tucker 2013). However, further research in this field is required to define adequate phosphate concentrations.
Other biochemical markers for bone metabolism, including carboxylated and uncarboxylated osteocalcin (cOC, ucOC), bone-specific alkaline phosphatase (BAP), amino terminal telopeptide (NTX), and carboxy terminal telopeptide (CTX), are at this point only recommended in research settings.
Estrogen Supplementation
In females, hypergonadotropic hypogonadism needs to be assessed by measuring FSH, LH, and beta-estradiol concentrations. Estrogen is a powerful inhibitor of bone resorption via the alpha and beta estrogen receptors on osteoblasts and osteoclasts, and low levels negatively influence bone metabolism. Evaluation of these hormones and referral to a pediatric endocrinologist should start from the age of 10–12 years (Fridovich-Keil et al. 2011).
Physical Activity Evaluation
Sufficient physical activity is required to achieve optimal bone mass. The World Health Organization (WHO) recommends 60 min of moderate- to vigorous-intensity physical activity per day for children and 150 min/week for adults. However, this is often not achieved. Furthermore, patients with classic galactosemia might be less physically active due to motor dysfunction (Rubio-Agusti et al. 2013) and less participative in social activities (Gubbels et al. 2011). Regular evaluation of physical activity in patients with this disease is therefore important, and a standardized questionnaire, for instance, the Physical Activity Questionnaire for Children and Adolescents (PAQ-C/A), can be used for this (Janz et al. 2008).
Assessment of Spinal Deformities
Scoliosis and hyperkyphosis are seen in 1–5% of all children in the general population and seem to be partly related to reduced bone mass and neurological abnormalities (Altaf et al. 2013). Scoliosis is defined as a lateral curvature of the spine that is more than 10° on a conventional X-ray in standing position. A hyperkyphosis is defined as a kyphosis of more than 45°. We observed a prevalence of 29% of these spinal deformities in a cohort of patients with classic galactosemia (n = 24, 14 females and 10 males; age range 13–48 years with a mean of 22 years), which is surprisingly higher than reported in the general population (unpublished results). A relationship between galactosemia and deformities of the spine has not been reported. It is questionable whether the observation in our cohort represents a real phenotypical characteristic or whether it is a coincidental finding. Yet, we advise to perform physical examination of the spine.
Dual-Energy X-Ray Absorptiometry
The method of choice to evaluate the bone mass is with dual-energy X-ray absorptiometry (DXA) scans, since this is a safe and relatively easy method with low exposure to radiation and low costs. Recently, the 2013 recommendations of the International Society for Clinical Densitometry have been published (Schousboe et al. 2013; Gordon et al. 2014). For postmenopausal women and men aged 50 years or older, DXA scans of the lumbar spine, femoral neck, and total hip are advised and T-scores are preferred to express the decrease in BMD. However, in premenopausal women and men younger than 50 years of age, Z-scores taking into account age, gender, and ethnicity are preferred. Also for children Z-scores are preferred and the results should be adjusted in children with short stature or growth delay. Measurements of the BMD of the lumbar spine and the total body less head (TBLH) are recommended in children, since they yield the most reliable results. DXA scans of the femur have been proven to be unreliable in children, and total body scans with the head might give false-positive outcomes due to the relative large size of the head during childhood.
In postmenopausal women and men aged 50 years or older, a BMD T-score ≤ −1.0 standard deviation (SD) is diagnostic of low bone mass (formerly called osteopenia), while a T-score ≤ −2.5 SD is diagnostic of osteoporosis. A BMD Z-score ≤ −2.0 SD in premenopausal women or males younger than 50 years of age is defined as a BMD below the expected range for age, whereas a Z-score > −2.0 SD represents a BMD within the expected range for age (Schousboe et al. 2013). In children the diagnosis of osteoporosis requires either the finding of one or more vertebral compression fractures or the presence of both a BMD Z-score ≤ −2.0 SD and a clinically significant fracture history, meaning two or more long bone fractures by age 10 years or three or more long bone fractures at any age up to 19 years. A Z-score ≤ −2.0 SD without a clinically significant fracture is classified as a low BMD (Gordon et al. 2014).
Follow-Up and Therapeutic Interventions
Dietary Evaluation and Bone Metabolism Markers
Batey et al. (2013) found that most adults with galactosemia do not routinely visit a nutritionist, which might have implications for their bone health. Since a balanced diet is important for maximizing bone accrual during adolescence as well as for maintaining bone mass during adulthood, regular dietary evaluation throughout life is desirable. We recommend yearly dietary assessment, preferably by a nutritionist, with special focus on energy, protein, and micronutrient requirements. In case a patient’s diet is suboptimal, enhanced nutritional counseling is essential to optimize a patient’s general diet taking into account limitations deriving from galactose restriction. Special focus on vitamin D and calcium intake is suggested, including yearly evaluation of total 25(OH)D serum concentrations. We recommend supplementation of calcium and vitamin D when intake is lower than the recommended daily intake and does not normalize despite dietary optimization. When vitamin D supplementation has been initiated, more frequent monitoring of 25(OH)D serum concentrations might be helpful in determining the optimal dosage. Supplementation of vitamin K might be beneficial when combined with an adequate intake of calcium and vitamin D, but currently there is not enough evidence to recommend the routine use of vitamin K supplements.
Estrogen Supplementation
If evaluation of hormone status indicates hypergonadotropic hypogonadism, initiation of hormonal replacement therapy (HRT) needs to be considered. The decision to start supplementation during adolescence will have to take into consideration growth, psychological factors, and bone measurements. Duration of HRT throughout adult life will depend on an individual assessment of the possible risks and benefits.
Physical Activity Evaluation
We advise physicians to assess a patient’s physical activity and to encourage exercise when evaluation suggests that the patient does not meet the recommendations. Implementation of a regular routine of weight-bearing exercise is recommended, taking into consideration possible physical limitations.
Assessment of Spinal Deformities
For now, we recommend physicians to evaluate for possible spinal deformities during routine physical examination. In case of clinical suspicion, an X-ray of the entire spine with a Cobb angle is recommended, and subsequent referral to an orthopedist for extensive evaluation may be considered (Hresko 2013).
Dual-Energy X-Ray Absorptiometry
It is advised to assess BMD from an early age to ensure that optimal bone mass is reached in early adolescence. We recommend the first DXA to be performed at the age of 4 years, or as soon as the child is able to lie still, since a decreased bone mass can already be present at this early age. In children the minimum time interval between subsequent DXA scans is 6–12 months (Gordon et al. 2014). We suggest yearly DXA scanning when BMD is ≤ −2.0 SD and one DXA scan per 2 years when BMD is higher. In adults it is advised to repeat a DXA scan one year after initiation or change of therapy (Schousboe et al. 2013). The interval can be increasingly elongated once the BMD is stable.
Furthermore, we recommend regular assessment of fracture history in order to determine whether a pediatric patient meets osteoporosis criteria and to evaluate the clinical relevance of a patient’s reduced bone mass. In patients with frequent clinically relevant fractures, additional pharmacological therapy needs to be considered.
Conclusion
Our recommendations regarding assessment and follow-up of decreased bone mass in patients with classic galactosemia (Fig. 1):
-
Dietary evaluation to assess adequacy of a patient’s diet.
-
Optimization of calcium intake, either improvement of dietary intake (preferably) or supplements.
-
Monitoring of vitamin D status by dietary assessment and laboratory measurement of total 25(OH)D concentrations. If total 25(OH)D serum concentrations are <30 ng/mL (<75 nmol/L), intake should be improved through diet or supplements.
-
Hormonal status evaluation in females, in case of hypergonadotropic hypogonadism HRT, should be considered. Initiation and duration of treatment should take into consideration potential harms and benefits.
-
Assessment of physical activity using standardized questionnaires. In case the WHO recommendations are not met, exercise needs to be encouraged.
-
Evaluate for spinal deformities, since these might be more prevalent in this patient group, and fracture rate estimation.
-
DXA as the tool to monitor BMD. DXA scans of the lumbar spine and TBLH are advised in children, whereas for adults DXA scans of the lumbar spine, femoral neck, and total hip are preferred.
Abbreviations
- 1,25(OH)2D:
-
Calcitriol
- 25(OH)D:
-
25-Hydroxyvitamin D
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- DXA:
-
Dual-energy X-ray absorptiometry
- HRT:
-
Hormonal replacement therapy
- IGF-1:
-
Insulin-like growth factor 1
- IGFBP-3:
-
Insulin-like growth factor binding protein 3
- POI:
-
Primary ovarian insufficiency
- SD:
-
Standard deviation
- TBLH:
-
Total body less head
- WHO:
-
World Health Organization
References
Altaf F, Gibson A, Dannawi Z, Noordeen H (2013) Adolescent idiopathic scoliosis. Br Med J 346:f2508
Batey LA, Welt CK, Rohr F et al (2013) Skeletal health in adult patients with classic galactosemia. Osteoporos Int 24(2):501–509
Braam LA, Knapen MH, Geusens P et al (2003) Vitamin K1 supplementation retards bone loss in postmenopausal women between 50 and 60 years of age. Calcif Tissue Int 73(1):21–26
Calvo MS, Tucker KL (2013) Is phosphorus intake that exceeds dietary requirements a risk factor in bone health? Ann N Y Acad Sci 1301:29–35
Coss KP, Doran PP, Owoeye C et al (2013) Classical Galactosaemia in Ireland: incidence, complications and outcomes of treatment. J Inherit Metab Dis 36(1):21–27
Eisman JA (1999) Genetics of osteoporosis. Endocr Rev 20(6):788–804
Fridovich-Keil JL, Gubbels CS, Spencer JB, Sanders RD, Land JA, Rubio-Gozalbo E (2011) Ovarian function in girls and women with GALT-deficiency galactosemia. J Inherit Metab Dis 34(2):357–366
Gordon CM, Leonard MB, Zemel BS (2014) 2013 Pediatric position development conference: executive summary and reflections. J Clin Densitom 17:219–224
Gubbels CS, Maurice-Stam H, Berry GT et al (2011) Psychosocial developmental milestones in men with classic galactosemia. J Inherit Metab Dis 34(2):415–419
Guralp O, Erel CT (2014) Effects of vitamin K in postmenopausal women: mini review. Maturitas 77(3):294–299
Holick MF, Binkley NC, Bischoff-Ferrari HA et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96(7):1911–1930
Hresko MT (2013) Clinical practice. Idiopathic scoliosis in adolescents. New Engl J Med 368(9):834–841
Janz KF, Lutuchy EM, Wenthe P, Levy SM (2008) Measuring activity in children and adolescents using self-report: PAQ-C and PAQ-A. Med Sci Sports Exerc 40(4):767–772
Jumbo-Lucioni PP, Garber K, Kiel J et al (2012) Diversity of approaches to classic galactosemia around the world: a comparison of diagnosis, intervention, and outcomes. J Inherit Metab Dis 35(6):1037–1049
Kaufman FR, Loro ML, Azen C, Wenz E, Gilsanz V (1993) Effect of hypogonadism and deficient calcium intake on bone density in patients with galactosemia. J Pediatr 123(3):365–370
Landin LA (1997) Epidemiology of children’s fractures. J Pediatr Orthop B 6(2):79–83
Panis B, Forget PP, van Kroonenburgh MJ et al (2004) Bone metabolism in galactosemia. Bone 35(4):982–987
Panis B, Vermeer C, Marinus JPG et al (2006) Effect of calcium, vitamins K1 and D3 on bone in galactosemia. Bone 39(5):1123–1129
Panis B, Gerver WJ, Rubio-Gozalbo ME (2007a) Growth in treated classical galactosemia patients. Eur J Pediatr 166(5):443–446
Panis B, van Kroonenburgh MJ, Rubio-Gozalbo ME (2007b) Proposal for the prevention of osteoporosis in paediatric patients with classical galactosaemia. J Inherit Metab Dis 30(6):982
Rubio-Agusti I, Carecchio M, Bhatia KP et al (2013) Movement disorders in adult patients with classical galactosemia. Mov Disord 28(6):804–810
Rubio-Gozalbo ME, Hamming S, van Kroonenburgh MJ, Bakker JA, Vermeer C, Forget PP (2002) Bone mineral density in patients with classic galactosaemia. Arch Dis Child 87(1):57–60
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive summary of the 2013 ISCD position development conference on bone densitometry. J Clin Densitom 16(4):455–466
van Staa TP, Dennison EM, Leufkens HG, Cooper C (2001) Epidemiology of fractures in England and Wales. Bone 29(6):517–522
Vandenplas Y, Castrellon PG, Rivas R et al (2014) Safety of soya-based infant formulas in children. Br J Nutr 111:1340–1360
Waisbren SE, Potter NL, Gordon CM et al (2012) The adult galactosemic phenotype. J Inherit Metab Dis 35(2):279–286
Acknowledgment
The authors thank Sarah Bogovic, research student, for her help with the figure.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Communicated by: Gerard T. Berry, MD
Appendices
Synopsis
Bone health assessment in patients with classic galactosemia includes dietary evaluation, biochemical monitoring (vitamin D and estrogen status), assessment of physical activity, skeletal deformities and fractures, and serial DXA scans.
Compliance with Ethics Guidelines
Conflict of Interest
Britt van Erven, Myrna M.M. Römers, and M. Estela Rubio-Gozalbo declare that they have no conflict of interest.
Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Details of the Contributions of Individual Authors
BvE, PhD on galactosemia, performed the study and drafted the manuscript. MR searched for relevant literature and helped to draft the manuscript. ER, PhD supervisor and lead of the galactosemia research group in Maastricht, designed, supervised, and coordinated the study and the final version of this manuscript. All authors have read and approved the final manuscript.
Rights and permissions
Copyright information
© 2014 SSIEM and Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
van Erven, B., Römers, M.M.M., Rubio-Gozalbo, M.E. (2014). Revised Proposal for the Prevention of Low Bone Mass in Patients with Classic Galactosemia. In: Zschocke, J., Gibson, K., Brown, G., Morava, E., Peters, V. (eds) JIMD Reports, Volume 17. JIMD Reports, vol 17. Springer, Berlin, Heidelberg. https://doi.org/10.1007/8904_2014_331
Download citation
DOI: https://doi.org/10.1007/8904_2014_331
Received:
Revised:
Accepted:
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-44577-8
Online ISBN: 978-3-662-44578-5
eBook Packages: MedicineMedicine (R0)