Abstract
Summary
The amount and intensity of walking to maintain a healthy skeleton is unknown. This study examined the relationship between habitual walking activity and femoral bone mineral density (BMD) in healthy individuals using a quantitative theory for bone maintenance. Our results suggest a gender, weight, and speed sensitivity of walking interventions.
Introduction
Walking has been extensively promoted for the prevention of osteoporosis. The amount and intensity of walking to maintain a healthy skeleton is unknown and evidence to support a specific target of steps per day is lacking. The goal of our study was to examine the relationship between habitual walking activity and femoral bone mineral density (BMD) in healthy individuals using a quantitative theory for bone maintenance.
Methods
Habitual walking activity and total femur BMD were measured in 105 individuals (49–64 years). An index of cumulative loading (bone density index, BDI) was examined as a predictor of BMD. The BDI–BMD relationship was used to predict the steps per day to maintain healthy BMD values for a range of body weights (BW) and walking speeds.
Results
For females but not for males, BDI was correlated with BMD (r 2 = 0.19, p < 0.001). The total required steps per day to maintain a T-score of −1.0 for a female with the average BW of the study cohort, walking at 1.00 m/s is 4,892 steps/day. Substantially more steps (18,568 steps/day) are required for a female with a BW 20% lighter than the average for our female cohort. For these lighter females, only at a walking speed greater than 1.32 m/s was 10,000 steps/day sufficient to maintain a T-score of −1.0.
Conclusions
Our results suggest a gender, weight, and speed sensitivity of walking interventions for osteoporosis. In persons of low BW, the necessary steps per day to maintain BMD can be substantially greater than the often-quoted 10,000 steps.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major health concern for older adults [1–4]. Activity modifying interventions to increase the cumulative mechanical loading to the skeleton have received significant attention as a potential means for increasing bone mass. Walking is the most common weight-bearing activity in older adults [5]. It has been extensively promoted for the prevention of osteoporosis. However, the amount and intensity of walking to maintain a healthy skeleton is unknown. Thus, in the context of skeletal health, evidence to support a specific target of steps per day is lacking.
Studies that have investigated walking as a sole exercise intervention for preserving or augmenting bone density in postmenopausal women have reported limited benefit or inconsistent results [6–9]. A meta-analysis [9] of studies that examined the effect of walking interventions on bone density in postmenopausal women indicated a strong trend for a relationship between walking and bone mineral density (BMD) but one that did not reach statistical significance. The lack of success of these interventions might be attributable to aspects of study design, such as the choice of walking intensity (speed), walking duration (steps per day), or the total duration of the intervention. In general, those interventions that have prescribed higher intensity weight-bearing activities have resulted in greater gains in BMD [7]. However, evidence to support specific quantitative guidelines for intensities and durations of walking to maintain or enhance skeletal health has not been established. In addition, few investigations of the role of walking in maintaining or increasing bone density have included male participants, despite the fact that osteoporotic fracture is also an important concern for older men. Thus, there is a need to gain a better understanding of the interaction between load history and maintenance of BMD in an aging population.
The Bone Density Index (BDI) [10, 11] offers an opportunity to examine the influence of a daily walking regimen on bone health. With this index, it is possible to investigate the effects and interactions of body weight (BW) and habitual walking activity patterns (number of steps and walking speed). The BDI has been shown to correlate with calcaneus BMD in healthy women [10] and with hip BMD in a group of subjects with chronic stroke [11] using the ground reaction force (GRF) as a surrogate for skeletal loading. These results indicate that the GRF is a reasonable surrogate for the loading at the calcaneus in healthy individuals, perhaps due to the proximity of the applied force to the joint. While the GRF in walking was a reasonable surrogate for the loading of the proximal femur in the group of chronic stroke patients, it is not known if it would also be an adequate surrogate measure of loading in a healthy population, where a greater variety of loading conditions may be experienced. In addition, while highly detailed assessments of single-day activity profiles can be captured [10], this type of data logging over the extended period needed to accurately assess habitual activity patterns [12] is not always feasible. It is therefore of interest to know if a comparable BMD vs BDI correlation for the proximal femur exists using epoch-based speed and step-count data along with GRF data for walking for healthy older individuals.
The purpose of this study was to test for a correlation between the BDI, calculated using epoch-based speed and step-count data along with GRF data for walking and BMD of the proximal hip in healthy older male and female adults. This relationship between BDI and BMD was used to predict, for a range of BWs and walking speeds, the number of steps per day necessary to maintain a range of BMD values. These data were use to test the hypothesis that 10,000 steps/day are sufficient to maintain a healthy BMD for individuals with healthy BWs.
Methods
Subject inclusion/exclusion criteria
Healthy males and females, for whom walking was their primary form of leisure-time physical activity, were recruited from the San Francisco Bay area. Subjects were between the ages of 49 and 65 years with a body mass index of less than or equal to 30 kg/m2. Individuals with a self-reported current or recent (within 5 years) history of regular participation in impact or jumping exercises or sports (i.e., jogging, running, tennis, softball, basketball, volleyball, skiing, etc.), were excluded. A current or recent history of reduced weight-bearing or non-weight bearing exercises, such as bicycling, swimming, etc., was permissible. Individuals with a recent self-reported history (<2 years) of starting, stopping or modifying any osteoporosis treatment, such as hormone replacement therapy, PTH, or bisphosphonates were excluded. Other criteria for exclusion included a history of hip surgery, lower-limb fracture, hip joint replacement, use of an assistive device while walking, obvious limp while walking, chemotherapy, and long-term use of corticosteroids, such as prednisone, or prolonged bed rest. Additionally, those with self-reported medical conditions that could affect the skeletal system, such as diabetes, Paget’s disease, hyperthyroidism, chronic renal failure, rickets, hypocalcemia, hypercalcemia, etc., were excluded. Inclusion of female subjects was limited to those who were postmenopausal. All participants provided informed consent according to an approved IRB protocol prior to participation in the study.
Bone mineral density
BMD was measured using a GE-Lunar iDXA Dual X-ray Absorptiometry (DXA) scanner (GE Healthcare, Madison, WI). The region of interest was the total proximal femur [13] as determined by the manufacturer’s software. The T-scores (BMD normalized by the young adult reference BMD value) were calculated by the scanner software platform. The World Health Organization defines a T-score ≥ −1 as normal, a T-score < –1 and > –2.5 indicates low bone density or osteopenia, and a T-score ≤ –2.5 indicates osteoporosis.
Measurement of free-living walking activity
Habitual walking activity (number of steps per day and walking speed) was collected via an activity monitor (AMP 231/331; Dynastream Innovations Inc., Cochrane, Alberta, Canada). A change to the AMP 231 model was made part way through the study due to durability issues with the battery door on the AMP 331 that became apparent after replacement of the batteries. The AMP device was worn in a sleeve at the ankle for a period of up to 7 days. The AMP monitor allocates each second of monitoring into one of three classes: inactive, active, locomotion. Classification was done using Dynastream proprietary software according to the following definitions (AMP Help & Documentation Manual, Rev 3.3, 2004):
Inactive
“Time spent sitting, lying, or standing still is accumulated into the inactive class. To be classified as inactive, the wearer must not take any steps for at least 20 s.”
Active
“Time spent ‘up and about’ is accumulated into the active class.”
Locomotion
“Time spent ‘walking somewhere’ is accumulated into the locomotion class. The wearer must take at least 20 consecutive steps for the activity to register in the locomotion class”.
Participants were instructed to put on the AMP device in the morning, immediately after waking and continue to wear it throughout the day. The device was attached to the ankle by a Velcro strap and aligned with the Achilles tendon. Days with fewer than 10 h of combined time spent in the active and locomotion classes suggested that a subject was not wearing the device for the entire day in question, and those days were discarded from the analysis. Subjects were only included in the final analysis if they had three or more acceptable days of data [12, 14]. The internal AMP software accumulates second-by-second data and records on its internal memory on an epoch-by-epoch basis. In order to allow for up to 7 days of data logging, a 6-min epoch was chosen for the AMP 331 device. The AMP 231 device used a non-changeable, 10-min epoch. Average walking speed was internally calculated by the AMP and recorded for each epoch that contained any locomotion steps. Locomotion steps were further classified into speed categories based on 25th, 50th, and 75th percentile of maximum detected walking speed. Subjects were instructed not to change their customary physical activities during the 7-day monitoring period. The AMP device counts strides, which are multiplied by two by the device software to determine the total number of steps per day on both right and left legs. The mechanical stimulus for a given leg occurs during the stance phase of the gait cycle for that leg. The loading cycles for a given hip are thus one half of the total step count; therefore, activity monitor data were divided by two to obtain steps per leg per day.
Bone density predictor
To estimate the bone stimulus resulting from each subject’s habitual daily walking activity, we used a previously developed predictor of bone density called the BDI [10, 15]:
In this equation, GRFz i represents the peak vertical GRF for each loading cycle, n i. The exponent m is an empirically determined constant that weights the relative importance of force magnitude and loading cycles, and β is a scaling factor for BW (β = subject BW/mean BW). A mean BW was calculated separately for males and females. The derivation of Eq. 1 based on a more general model of mechanically regulated bone adaptation, details can be found elsewhere [16, 17].
As values of the peak GRFs for free-living walking on a step-by-step basis were not available in the current study, peak GRFs were calculated for the locomotion class steps binned based on the quartiles of locomotion speed. The overall average walking speed for each subject was used to estimate an overall average GRF for all steps in the active (non-locomotion) category. The binned form of Eq. 1 was used to calculate the BDI for each subject:
where n 1 through n 4 are the number of steps per leg per day in the four speed quartile categories, n 5 is the number of steps per leg per day in the active (but non-locomotive) category, and GRF1 through GRF4 and GRFave are the corresponding values of the GRFs. Integer values of m between 3 and 12 were tested to determine which value produced the highest value of the correlation coefficient between BDI and BMD, as has been done previously [10, 17].
Gait measures
GRFs were quantified in the laboratory while subjects walked on an 11-m long walkway with an embedded force plate (Bertec Corp., Worthington, OH, U.S.A) at three self-selected speeds: slow, normal, and fast with multiple trials collected at each speed. The peak vertical GRF was normalized by subject BW (% BW). Walking speed during each trial was quantified by the velocity of a reflective marker placed on the iliac crest using an optoelectronic motion capture system (Qualisys AB, Gothenburg, Sweden).
A linear regression equation for walking velocity and vertical component of the GRF was determined for each subject from the laboratory gait analysis. The regression equation was based on between five and nine trials for each subject. This trials for which the subject did not step within the boundaries of the force platform or where the iliac crest marker was obscured for a large portion of the stance phase, were discarded. The linear regression was used to estimate a GRFz magnitude for each of the four speed quartiles for each subject measured by the activity monitor.
Statistics
Linear regression models were used to investigate the relationship between BDI and BMD, steps/leg/day and BMD and walking speed and BMD for females and males. Pearson’s correlations were used to investigate the relationships between age and BW, age and BMD, age and steps/leg/day, and age and walking speed. Statistical analyses were performed using SPSS Statistics 17.0 (SPSS Inc., Chicago, IL. USA).
Results
A total of 105 subjects completed the study (Table 1). Reasons for exclusion after the initial screening and informed consent process were noncompliance with the AMP use and health issues unrelated to the study or personal situation that occurred during the week between a subject’s first visit (consent signing, DXA measurement) and their second visit (gait analysis).
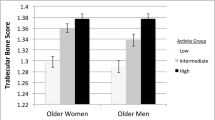
Based on individual T-scores for the total femur region of interest (not shown), 41 females and 28 males were in the normal range (T-score ≥ – 1.0), 25 females and 11 males were osteopenic (T-score < – 1.0 and > –2.5). There were no correlations between age and BMD, age and weight or between age and BMI (p > 0.05) for males or females. There was no correlation between the average number of steps per leg per day and age (females p = 0.841; males p = 0.377) or the average walking speed and age for either the females (p = 0.152) or the males (p = 0.639) (Fig. 1).
Walking characteristics measured under free-living conditions using the AMP activity monitor. No significant correlations with age were found. Steps per leg per day is shown for females, p = 0.841 (A) and males p = 0.377 (B); average walking speed is shown for females, p = 0.152 (C) and males, p = 0.639 (D)
For females, there was a significant correlation between BMD and BDI (p < 0.001; r 2 = 0.19) (Fig. 2). For males, BDI was not correlated with BMD. For the BDI calculations, a value of m = 6 resulted in the highest values of the correlation coefficients for BMD vs. BDI for females. Correlations for the males did not reach significance for any value of m. For consistency, the reported values for BDI for males are based on m = 6.
Using the regression equation for the female group, the number of habitual daily steps was calculated for different values of normalized BW (β) and for different T-score values assuming a habitual walking speed of 1.0 m/s (Fig. 3) for the approximate range of BMD values spanned by the regression data. To maintain a T-score = −1.00, an average weight individual (mass = 65.1 kg, β = 1.00) would require 4,892 steps/day. Substantially more steps per day are required for lighter individuals (18,568 steps/day for mass 52.5 kg; β = 0.8) and less steps per day for a heavier individual, (1,638 steps/day for mass 78.7 kg; β = 1.20)
Total steps per day required to maintain different target T-scores are given as a function of normalized BW (β). For an individual of average BW (β = 1.0, 65.6 kg) 4,892 steps/day are predicted necessary to maintain a T-score = −1.0. For individuals with lower BW (β < 1.0) more steps per day are required; for heavier individuals (β > 1.0) fewer steps per day are required
Habitual daily steps were also calculated for the range of average free-living walking speeds for females (Fig 4). For a lighter weight female (β = 0.8; 52.5 kg) walking slower than the average of this cohort (e.g., 0.9 m/s) 23,672 steps/day are needed to maintain a T-score of −1.0, while walking at a faster speed (e.g., 1.2 m/s) 12,630 steps per day are required.
Discussion
The results demonstrated a significant relationship between the proximal femur BMD and the BDI. Simple walking metrics, such as the average walking speed and the number of steps per day, were not associated with proximal femur BMD. This difference in outcomes suggests that the BDI is a more robust index to evaluate the relationship between a specific physical activity countermeasure for osteoporosis and BMD. The application of the BDI produced an important observation regarding the potential gender, weight, and intensity sensitivity of walking interventions for osteoporosis.
The ability of the BDI as an index to evaluate activity intervention likely comes from the fact that this index specifically relates daily mechanical stimulus to bone adaptation and is based on mechanistic principles, such as fatigue damage accumulation that are thought to influence the bone remodeling process [16]. A previous study [10] reported a significant correlation between calcaneal BMD and BDI in 42 healthy females between the ages of 25 and 74 years, with 19% of the variance in BMD accounted for, identical to that found for the proximal femur females in the present study. Thus, the distance from the loading measure (i.e., GRF) to the region of interest in the lower limb does not seem to influence the predictive strength of the BDI. Explaining only 20% of the variance due to an extrinsic, modifiable factor, such as walking, might seem low. However, the potential contribution from extrinsic factors is ultimately limited by the influence of genetic factors. Estimates of the influence of intrinsic or genetic factors on bone density generally exceed 50%, and in some studies, reported heritability values are substantially greater than 50% for some skeletal regions. In a study of adult monozygotic and dizygotic twins, Pocock et al. [18] reported heritability values for BMD in the proximal femur ranging from 0.57 for the trochanteric region to 0.85 for Ward’s triangle. Block et al. [19] stated that “as much as 80% of the variability in bone density may be genetically determined, allowing for substantially smaller contributions by environmental factors.” The fact that extrinsic factors account for a small percentage of the variation in bone density at certain skeletal sites suggests that a targeted, highly individualized exercise program aimed at mechanical stimulation at the hip and including an analysis of this stimulation are necessary to capture the true contribution of mechanical loading to bone density.
The application of the BDI–BMD relationship highlighted the importance of weight in the potential efficacy of a given walking intervention. For example, a female weighing 20% less (β = 0.80) than the average weight of the middle-age female cohort may have to take nearly four times as many steps per day (18,568 vs. 4,892) as an individual of average weight in order to maintain a T-score value of −1.0 (see Fig. 4), presuming there are no differences in the normalized GRFs between individuals. This (18,568 steps) is an ambitious steps per day goal, and thus, to increase success of an activity-modifying intervention in lower BW females, higher intensity activities or devices to artificially increase BW during walking might be necessary. This analysis suggests that the goal of 10,000 steps/day [20–24], that has been advocated by some as a target for a healthy lifestyle, should be re-examined when used in the context of skeletal health.
Walking speed is one modifiable variable that could potentially be used to increase the loading stimulus and decrease the number of steps/day needed in an intervention. However, for the lighter individuals (BW 20% lower than average), only for average free-living walking speeds greater than 1.32 m/s was 10,000 steps/day sufficient to maintain a T-score = −1.0. Amongst the female cohort, an average free-living walking speed greater that 1.32 m/s was only attained by 2 of the 66 subjects. This suggests that even when controlling for the intensity of a walking intervention, the often quoted goal of 10,000 steps/day [20–24] as a target for skeletal health should be re-examined.
The gender based differences in the ability of BDI to predict BMD may be related to differences between genders in BMD heritability at the proximal femur. In a recent study of monozygotic twins, Tse et al. [25] found that the BMD in the total femur region of interest had a high heritability value in males (87.3%) and a relatively lower value in females (48.8%). This suggests that environmental (extrinsic) factors, such as habitual walking, may have substantially less influence on the BMD at the hip in males as compared to females. Worthen et al. [11] in a study of chronic stroke patients reported a significant correlation between proximal femur BMD and BDI in males. The chronic stroke subjects had persistent walking deficits. By contrast, the subjects in the present study were healthy with no obvious walking deficits and were more likely to experience a larger number of higher loading walking events that may not have been accurately captured by the epoch-based activity monitoring used. The fact that BDI does not account for all of the potential extrinsic variability in females or males suggests that a more accurate measurement of habitual physical activity history may be required in order to detect the underlying relationships between habitual joint loading and BMD.
In contrast to the prevailing literature, a correlation between age and BMD, age and steps per leg per day, and age and walking speed were not found in the cohort tested. For an average aging population, the literature suggests that there is a decrease in BMD of 0.7–0.9% per year [26] along with a decrease in habitual walking activity [27] and walking speed [28]. However, studies have also noted that exercise attenuates losses in functional capacity with age [29, 30], and therefore, the lack of decreases in BMD, walking speed, and steps per day with age might be attributable to the levels of habitual activity in this study. Less than 10% of participants in this study would be classified as sedentary according to the activity classifications proposed by Tudor-Locke [20], which probably reflects some bias in the types of individuals who volunteered to participate in our study.
Our study has several limitations that should be mentioned. First, some limitations were caused by our narrow inclusion/exclusion criteria. Due to the necessity to capture each subject’s free-living physical activity via a device that only recorded steps and walking speed, we were unable to include subjects who participated in high-impact sports whom one would expect to have higher than average bone density. The AMP 231/331 devices cannot accurately record jogging or running steps or speed, and as a result, we could not include subjects who participated in such activities. There are also limitations of the AMP device for measurement of non-level walking activities. The magnitude of hip joint loading during activities, such as stair climbing, trail hiking, step aerobics, etc., may be considerable higher than those experienced in level walking [31]. Many of these non-walking events would be counted by the activity monitor, but they would not be accurately represented by a subject’s gait laboratory testing. The inability to measure and account for the stimulus provided by these activities limits the accuracy of the BDI calculation. There is a need in this field of research for the development and validation of more versatile and robust sensors capable of measuring the stimulus at the hip or ground during a wide range of daily activities. At present, however, we know of no validated device, although several are likely in development that may have the capability and reliability to monitor any relevant bone-stimulus or force parameter for multiple days and that requires minimal user interaction or expertise. Also, based on a value of BMD 2.5 standard deviations or more below the young adult mean, no female or male subjects were classified as having osteoporosis. This is almost certainly lower than the expected rates of female and male osteoporosis in the San Francisco Bay area, even among those under 65 years of age. We do not have any explanation for these low rates in our study, expect that perhaps subjects with osteoporosis are less likely to respond to advertisements for participation in a study of bone density and walking activity. In addition, the exclusion of subjects with BMI greater than 30.0 meant that there were no obese subjects in the study. For any of these excluded or underrepresented groups, we do not know to what extent our results might apply.
In our study, the inclusion/exclusion criteria potentially may have biased participation to include subjects who had not substantially altered their habitual walking activity for the previous 5 years. Thus, the relationship we found between walking activity and femoral BMD cannot be directly compared with the effects of an intervention study consisting of a discrete change in walking activity imposed for a substantially shorter time period. Our results should therefore be interpreted in the context of relatively stable values of bone density with relatively stable levels of walking activity. Due to the cross-sectional nature of our study, it is not possible to estimate the time course of changes in BMD arising from a discrete change in habitual walking activity, typical in a walking intervention study. We also made no attempt to determine each subject’s physical activity history more than 5 years prior to enrolment in our study. Although there is growing evidence that the benefits of physical activity dissipate upon cessation of training [32], the time course of that dissipation is not well understood and remains a focus of current research. Thus, we do not know to what extent there was a close “equilibrium” between a subject’s recent physical activity and their current bone density, although the assumption of such equilibrium is implicit in our theoretical model.
Conclusions
In this study, we have assessed the degree to which habitual daily walking activity is associated with proximal femur BMD in healthy middle-aged males and females. A significant relationship between BDI and BMD was found, but only for females. The application of the BDI suggests a weight and speed sensitivity of walking interventions for osteoporosis. In the context of high-risk persons (e.g., low BW), the necessary steps per day to maintain BMD can be substantially greater than the often quoted value of 10,000 steps/day [3] for most walking speeds and may be an unreasonable goal for some individuals. Future research should explore interventions to safely increase the GRF magnitudes during everyday activities, which may provide significant benefit for healthy skeletal aging.
Reference
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475
Lips P, van Schoor NM (2005) Quality of life in patients with osteoporosis. Osteoporos Int 16:447–455
Curry LC, Hogstel MO, Davis GC (2003) Functional status in older women following hip fracture. J Adv Nurs 42:347–354
Forsen L, Sogaard AJ, Meyer HE, Edna T, Kopjar B (1999) Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int 10:73–78
Centers for Disease Control (CDC) and Prevention (2000) Compliance with physical activity recommendations by walking for exercise. MMWR Morb Mortal Wkly Rep 49(25):560–565
Feskanich D, Willett W, Colditz G (2002) Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA 288:2300–2306
Hatori M, Hasegawa A, Adachi H, Shinozaki A, Hayashi R, Okano H, Mizunuma H, Murata K (1993) The effects of walking at the anaerobic threshold level on vertebral bone loss in postmenopausal women. Calcif Tissue Int 52:411–414
Wu J, Oka J, Tabata I, Higuchi M, Toda T, Fuku N, Ezaki J, Sugiyama F, Uchiyama S, Yamada K, Ishimi Y (2006) Effects of isoflavone and exercise on BMD and fat mass in postmenopausal Japanese women: a 1-year randomized placebo-controlled trial. J Bone Miner Res 21:780–789
Martyn-St James M, Carroll S (2008) Meta-analysis of walking for preservation of bone mineral density in postmenopausal women. Bone 43:521–531
Bowley SM , Whalen RT. Physical activity and bone density in women. Orthop Res Soc 2001; 26-63
Worthen LC, Kim CM, Kautz SA, Lew HL, Kiratli BJ, Beaupre GS (2005) Key characteristics of walking correlate with bone density in individuals with chronic stroke. J Rehabil Res Dev 42:761–768
Tudor-Locke C, Burkett L, Reis JP, Ainsworth BE, Macera CA, Wilson DK (2005) How many days of pedometer monitoring predict weekly physical activity in adults? Prev Med 40:293–298
Lodder MC, Lems WF, Ader HJ, Marthinsen AE, van Coeverden SC, Lips P, Netelenbos JC, Dijkmans BA, Roos JC (2004) Reproducibility of bone mineral density measurement in daily practice. Ann Rheum Dis 63:285–289
Tudor-Locke C, Johnson WD, Katzmarzyk PT (2009) Accelerometer-determined steps per day in US adults. Med Sci Sports Exerc 41:1384–1391
Whalen RT , Breit GA. Method and apparatus for monitoring of daily activity in terms of ground reaction forces. 2001; 08/540,614:
Carter DR, Fyhrie DP, Whalen RT (1987) Trabecular bone density and loading history: regulation of connective tissue biology by mechanical energy. J Biomech 20:785–794
Whalen RT, Carter DR, Steele CR (1988) Influence of physical activity on the regulation of bone density. J Biomech 21:825–837
Pocock NA, Eisman JA, Hopper JL, Yeates MG, Sambrook PN, Eberl S (1987) Genetic determinants of bone mass in adults. A twin study. J Clin Invest 80:706–710
Block JE, Friedlander AL, Brooks GA, Steiger P, Stubbs HA, Genant HK (1989) Determinants of bone density among athletes engaged in weight-bearing and non-weight-bearing activity. J Appl Physiol 67:1100–1105
Tudor-Locke C, Bassett DR Jr (2004) How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med 34:1–8
Tudor-Locke C, Hatano Y, Pangrazi RP, Kang M (2008) Revisiting “how many steps are enough?”. Med Sci Sports Exerc 40:S537–S543
Tudor-Locke C, Ainsworth BE, Whitt MC, Thompson RW, Addy CL, Jones DA (2001) The relationship between pedometer-determined ambulatory activity and body composition variables. Int J Obes Relat Metab Disord 25:1571–1578
Bennett GG, Wolin KY, Viswanath K, Askew S, Puleo E, Emmons KM (2006) Television viewing and pedometer-determined physical activity among multiethnic residents of low-income housing. Am J Public Health 96:1681–1685
Harvey JT, Eime RM, Payne WR (2009) Effectiveness of the 2006 Commonwealth Games 10, 000 Steps Walking Challenge. Med Sci Sports Exerc 41:1673–1680
Tse KY, Macias BR, Meyer RS, Hargens AR (2009) Heritability of bone density: regional and gender differences in monozygotic twins. J Orthop Res 27:150–154
May H, Murphy S, Khaw K (1994) Age-associated bone loss in men and women and its relationship to weight. Age Ageing 23:235–240
Bohannon RW (2007) Number of pedometer-assessed steps taken per day by adults: a descriptive meta-analysis. Phys Ther 87:1642–1650
Bohannon RW (1997) Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing 26:15–19
Visser M, Pluijm SM, Stel VS, Bosscher RJ, Deeg DJ (2002) Physical activity as a determinant of change in mobility performance: the Longitudinal Aging Study Amsterdam. J Am Geriatr Soc 50:1774–1781
Martin PE, Rothstein DE, Larish DD (1992) Effects of age and physical activity status on the speed-aerobic demand relationship of walking. J Appl Physiol 73:200–206
Bergmann G, Deuretzbacher G, Heller M, Graichen F, Rohlmann A, Strauss J, Duda GN (2001) Hip contact forces and gait patterns from routine activities. J Biomech 34:859–871
Englund U, Littbrand H, Sondell A, Bucht G, Pettersson U (2009) The beneficial effects of exercise on BMD are lost after cessation: a 5-year follow-up in older post-menopausal women. Scand J Med Sci Sports 19:381–388
Acknowledgments
This material was based on work supported by the Department of Veterans Affairs, Veterans Health Administration, Rehabilitation Research and Development Service, Merit Review project A2592R. Special thanks to Christy Dairaghi, Barb Elspas, Joe Guerricabeitia, Jonathan Rylander, and Sparkle Williams.
Conflicts of interest
None.
Funding sources
Department of Veterans Affairs, Veterans Health Administration, Rehabilitation Research and Development Service, Merit Review project A2592R.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boyer, K.A., Kiratli, B.J., Andriacchi, T.P. et al. Maintaining femoral bone density in adults: how many steps per day are enough?. Osteoporos Int 22, 2981–2988 (2011). https://doi.org/10.1007/s00198-011-1538-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1538-9