Abstract
Summary
Relationships between objectively assessed free-living physical activity (PA) and changes in bone health over time are poorly understood in older adults. This study suggests these relationships are sex-specific and that body composition may influence the mechanical loading benefits of PA.
Introduction
To investigate associations of objectively assessed PA and bone health in community-dwelling older adults.
Methods
This secondary analysis of a subset of the Tasmanian Older Adult Cohort study included participants with PA assessed utilising ActiGraph GT1M accelerometers over 7 days (N = 209 participants, 53% female; mean ± SD age 64.5 ± 7.2 years). Steps/day and PA intensity were estimated via established thresholds. Bone mineral content (BMC) was acquired at the total hip, lumbar spine, legs and whole body by DXA at baseline and approximately 2.2 years later. Relationships between PA and BMC were assessed by multivariable linear regression analyses adjusted for age, smoking status, height and total lean mass.
Results
Men with above-median total hip BMC completed significantly less steps per day, but there was no significant difference in PA intensity compared with those with below-median BMC. There were no significant differences in PA in women stratified by median BMC. In women, steps/day were positively associated with leg BMC (B = 0.178; P = 0.017), and sedentary behaviour was negatively associated with leg BMC (− 0.165; 0.016) at baseline. After adjustment for confounders including lean mass and height, higher sedentary behaviour at baseline was associated with declines in femoral neck BMC (− 0.286; 0.011) but also with increases in pelvic BMC (0.246; 0.030) in men and increases in total hip BMC (0.215; 0.032) in women, over 2.2 years. No other significant longitudinal associations were observed after adjustment for body composition.
Conclusions
Associations of accelerometer-determined sedentary behaviour and PA with bone health in older adults differ by sex and anatomical site and are mediated by body composition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lifestyle interventions to reduce osteoporosis prevalence and subsequent fracture risk are of significant public health interest [1]. Studies have indicated a positive effect of regular physical activity (PA) on bone health in children and adolescents [2, 3]. The associations in older adults are inconsistent and may be influenced by a range of other factors such as gender, body composition, or hormonal status [4, 5], but higher levels of PA appear to attenuate, and may even reverse, age-related bone loss at certain sites [4, 6, 7]. The inconsistent findings from older adult populations may be partly explained by sex differences, or potentially heterogeneity in methods of PA quantification.
While self-reported PA questionnaires and diaries are generally reliable measures of intentional PA [8], incidental or free-living PA measurement may be incorrectly estimated [9, 10]. Objective measurement techniques are likely to provide more accurate estimates of incidental PA. Pedometers accurately estimate step counts but are unable to quantify intensity or exertion within ambulatory activity [11]. In contrast, accelerometers are able to quantify intensity of PA via various established cut points. As such, accelerometers are increasingly used as an objective measurement tool capable of assessing PA intensity and sedentary behaviour, which may have differing associations with health outcomes [12].
Exercise interventions indicate that moderate to high impact weight-bearing exercise may be the most effective exercise modality for improving bone health in older adults [13]. As a result, accelerometer-determined estimates of PA performed at higher intensity may serve as a proxy estimate for high-impact exercise. While cross-sectional studies have examined associations of accelerometer-determined PA intensity with bone mineral density (BMD) [14,15,16,17], conflicting observations have been observed and longitudinal associations with bone mineral content (BMC) are largely unknown [18]. We hypothesised that greater amounts of higher intensity PA would be associated with greater BMC and BMD at weight-bearing sites; however, relationships would vary between men and women due to differences in body composition. As such, we aimed to determine associations between varying intensities of PA and bone mass at a range of sites in community-dwelling older adults.
Methods
Study design and participants
This study was a secondary analysis of a subset of the Tasmanian Older Adult Cohort study, a prospective, population-based study of community-dwelling older adults designed to investigate progression of osteoarthritis and osteoporosis. An equal number of men and women between the ages of 50 and 80 years were randomly selected from the electoral roll in Southern Tasmania (population 229,000), with a response rate of 57%. Electoral rolls represent the most complete population information available in Australia because voting in federal and state elections is compulsory. The sample was stratified by sex to provide equal numbers of men and women, and equal distributions were drawn from urban and rural areas in Southern Tasmania. Exclusion criteria included contraindication for magnetic resonance imaging (required to examine osteoarthritis progression) and institutionalisation. The study was approved by the Southern Tasmanian Health and Medical Human Research Ethics committee, and written informed consent was obtained from all participants.
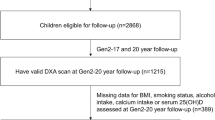
One thousand one hundred participants were enrolled in the study, and 1099 attended a baseline clinic between March 2002 and September 2004. Follow-up data was collected for 875 participants approximately 2.6 years later (phase 2) and for 767 participants approximately 5 years after baseline (phase 3).
Accelerometers were not available at baseline during this study and were incorporated into the experimental protocol midway through phase 2. Therefore, for the present analysis, phase 2 was considered as baseline, and participants were included if they had complete accelerometer data at phase 2 and dual-energy x-ray absorptiometry (DXA) at both phase 2 and phase 3 (mean ± SD; 2.2 ± 0.9 years later). A total of 871 participants had completed DXA assessment at phase 2 but only 210 completed accelerometer assessments. One of these participants did not complete DXA assessment at phase 3, and so a total of 209 participants were included in this analysis.
Descriptive variables
Height was measured to the nearest 1 mm (shoes and socks removed) using a stadiometer (Invicta, Leicester, UK). Weight was measured to the nearest 0.1 kg (shoes and bulky clothing removed) using electronic scales (Heine, Dover, NH, USA). Participant’s body mass index (BMI [kg/m2]) was subsequently calculated. Data was also collected on smoking status via self-reported questionnaires.
Accelerometer-determined physical activity
Accelerometer-determined PA was assessed for 7 days following the participant’s clinic visit at baseline. Participants also utilised an activity diary to record start and end wear times, any reason the accelerometer may have been removed, such as swimming, showering or any circumstances when the participants felt that they may have produced inaccurate accelerometer estimates, such as driving on uneven ground. Participants were excluded from analysis if they did not wear the device for at least five valid days during the 7-day monitoring period. A valid day was considered as having worn the device for more than 10 h, as based on previous accelerometer studies [19, 20].
Accelerometer data (ActiGraph GT1M, ActiGraph, Pensacola, FL) was initially recorded as ‘counts’, generated via proprietary algorithms. Using count data, intensity of activity time periods and step counts per day were generated. The Freedson equation and cut points proposed by Matthews were utilised to define PA intensity and sedentary behaviour respectively [21]. Four categories of PA intensity were determined according to metabolic equivalent (MET) values; sedentary behaviour (< 1.5METs), light PA (1.5–2.9METs), moderate PA (3.0–5.9METs) and vigorous (> 6METs) [22].
Body composition and bone parameters
Body composition, BMC (g), and BMD (g/cm2) were determined by whole-body, total hip and lumbar spine scans performed on a Hologic Delphi densitometer (Hologic, Waltham, MA. Apex v2.0) at baseline and follow-up. BMC and BMD values were recorded at the trochanter, femoral neck, total hip, lumbar spine, pelvis, arms, legs and whole body. The same densitometer was used throughout the study and quality control was performed using a spine phantom prior to testing. The longitudinal coefficient of variation for this spine phantom using our machine between 2002 and 2007 was 0.39% [23]. Change in both BMC and BMD at each site was calculated as values at phase 3 less phase 2.
Statistical analysis
All variables were tested for normality and non-parametric analyses were performed where required. Due to low amounts of vigorous intensity activity, moderate intensity and vigorous intensity PA were combined (MVPA). Spearman correlations assessed relationships between age and total hip BMC. Independent samples t tests compared means for continuous variables including descriptive statistics, accelerometer data and BMC between groups stratified as greater than or equal to versus less than median sex-specific total hip BMC. Categorical variables were compared using chi-square tests. Standardised beta coefficients from sex-stratified multivariable linear regression analyses were obtained to examine the relationship of PA intensities with BMC and BMD, along with changes in BMC and BMD from baseline to 2.2 years. Model 1 was adjusted for age and smoking status. Model 2 included covariates in model 1 and additionally, height and total lean mass. All statistical analyses were performed using SPSS Version 23 (IBM, USA), and a P value less than 0.05 was considered statistically significant.
Results
Two hundred and nine participants (53% female; mean ± SD age 64.5 ± 7.2 years) were included in this analysis. Total hip BMC was significantly greater in men than in women (mean ± SD 49.099 ± 8.374 vs 33.292 ± 6.809, P < 0.001), but was not correlated with age.
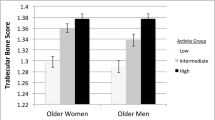
Table 1 presents statistics according to sex-specific median total hip BMC. In men, age, body weight and BMI were significantly greater in individuals with higher hip BMC. Smoking status was not significantly different between groups in men. Steps per day were significantly lower in men with higher total hip BMC. Women who had greater hip BMC were significantly taller and had higher body weight and BMI than those with lower hip BMC. There was no difference in smoking status between groups in women while there was also no difference in levels of PA. There was also no significant difference in the number of participants who met the American College of Sports Medicine (ACSM) guidelines of at least 150 min of MVPA per week between groups (P > 0.05).
Table 2 presents mean changes in BMC in men and women from baseline to follow-up. Total hip decreased significantly in men between assessments, while lumbar spine and arm BMC increased. In women, trochanter BMC decreased significantly, while leg BMC increased.
Table 3 presents cross-sectional multivariable regression coefficients for associations of PA and BMC at various sites between sexes. In men, accelerometer-determined steps per day were negatively associated with BMC at the trochanter, femoral neck, total hip, arms, pelvis and whole-body sites. After adjustment for height and lean mass, all associations became non-significant. No other significant cross-sectional associations were observed in men. In women, there were no significant associations between PA and BMC after adjustment for age and smoking status in model 1. Following further adjustment for height and lean mass in model 2, accelerometer-determined steps per day and MVPA were both positively associated with leg BMC. Sedentary behaviour was also negatively associated with leg, pelvis and whole-body BMC. No other significant cross-sectional associations were observed in women.
Table 4 reports sex-stratified standardised multivariable regression coefficients for prospective associations between baseline PA and change in BMC from baseline to follow-up. In men, sedentary behaviour was negatively associated with change in femoral neck BMC in models 1 and 2. Conversely, sedentary behaviour was positively associated with change in pelvic BMC in men and total hip BMC in women, in both models.
The above analyses were repeated for BMD outcomes, and Table 5 reports sex-stratified standardised multivariable regression coefficients for these analyses. In men, steps per day were positively associated with change in total hip BMD in model 1; however, after further adjustment for height and lean mass in model 2, this relationship was non-significant. Steps per day were also positively associated with change in femoral neck BMD but only in model 2. Sedentary behaviour was negatively associated with change in femoral neck BMD in model 2. No other associations were observed in men. In women, steps per day were positively associated with change in femoral neck BMD, but after adjustment in model 2, the relationship became non-significant. Steps per day were also positively associated with change in pelvic BMD yet only in model 2. Light intensity PA was also positively associated with leg BMD in models 1 and 2. Conversely, sedentary behaviour was positively associated with change in total hip BMD in model 2.
Discussion
This longitudinal study of community-dwelling older adults has demonstrated that sex-specific prospective and cross-sectional associations exist between accelerometer-determined PA, BMC and BMD, and that height and lean mass often mediate these relationships. Our findings highlight links between weight-bearing and the maintenance of skeletal health at clinically relevant sites in older adult populations may be influenced by body composition.
An unexpected finding was that accelerometer-determined steps per day were negatively associated with BMC at several sites in men in cross-sectional analyses, although this relationship was mediated entirely by height and lean mass. Conversely, in women, positive cross-sectional associations for steps per day and MVPA were observed with BMC, while sedentary behaviour appeared to be beneficial for BMC at the total hip. Positive longitudinal associations were also observed between PA and BMD in both men and women at the femoral neck, along with the total hip in men alone, although these relationships were inconsistent. These findings suggest that sex-related body composition differences potentially play an important role in differing effects of PA on BMC and BMD in older adults.
While interventional exercise studies have demonstrated positive benefits of higher intensity PA on skeletal health [5, 24, 25], the efficacy of free-living PA for maintenance of bone health is less clear. Results from cross-sectional studies measuring unstructured daily PA are conflicting [14, 16], and no previous study has examined longitudinal associations of accelerometer-derived PA with change in BMC or BMD in older adults. Indeed, it has been previously acknowledged that bone density in older adults may not be easily influenced by daily PA alone [15]. Gerdhem et al. suggest that reasons for this may be due to the low quantity of total PA undertaken by older adults [15]. Perhaps more specifically, it is possible that amounts of high-intensity or high-impact activity performed by older adults are insufficient for osteogenesis. Given 65% of men and 58% of women in our cohort completed sufficient MVPA as defined by the ACSM, our results suggest this level of activity is inadequate to influence their bone health. Specific PA guidelines for maintaining and improving bone health in older age may therefore need to be developed.
Increased mechanical loading remains important, with the quantity of bone loading determining the scale of osteogenic response and thus adaption of bone [26, 27]. The results from our study suggest that perhaps targeted exercise, rather than daily PA, is most likely to stimulate osteogenesis in older adults. Hinton et al. demonstrated that in an adult population (aged 25–60 years), a 6-month high-impact, weight-bearing exercise intervention improved BMD by 1.3% at the lumbar spine [28], while a 12-month high-impact exercise intervention in older men increased trochanteric BMC by 12.6% [24].
The magnitude of gravitational impact forces experienced during activity is naturally a product of both muscle force generation and body weight, where lower muscle force generation and/or body weight likely produce negligible impact force and therefore, little osteogenic benefit. As such, even individuals with high lean mass may not obtain improvements in skeletal health if they have low physical activity levels.
Our cross-sectional results in particular suggest that benefits of daily PA are largely mediated by an individual’s height and lean mass, and suggest that exercise targeting increases in muscle mass, strength and power, rather than greater gravitational weight-bearing alone, may be most important for driving osteogenesis in older adults. Indeed, Rhodes et al. demonstrated that significant gains in muscle strength occur in parallel with improvement in BMD [29], and the recent LIFTMOR trial demonstrated a 7.7% increase in femoral neck BMC alongside significant improvement in a number of strength and physical function-related assessments in response to 8 months of high-intensity resistance and impact training [30].
The notion that greater lean mass contributes to greater bone loading, further supports our finding of prospective negative associations between sedentary behaviour and both femoral neck BMC and BMD in men. Given the structure of the femoral neck, it and the proximal femur bear significant weight from the upper body, and these sites are subject to significant loading during activity [31, 32]. Equally, greater sedentary behaviour thus reduces total load on the femoral neck and may result in a concomitant decrease in bone mass. Further, Chastin et al. have also previously demonstrated cross-sectional negative associations between sedentary behaviour and femoral neck BMD, although solely in women [33].
While accelerometers may accurately quantify exercise intensity, these data often only approximate impact or loading forces, and as a result, activities with high mechanostatic strains implicated in osteogenesis may be underestimated or mischaracterised. Indeed, accelerometer-derived high-intensity PA may in certain instances very closely approximate high impact, yet there are a number of exercise modalities involving high intensity but minimal impact which therefore likely have little benefit for osteogenesis, such as cycling, swimming or rowing [34]. In an effort to overcome the limitations of quantifying impact by accelerometers, novel mathematical algorithms have been developed [35], and additional wearable devices such as cameras and/or multiple accelerometers have been deployed. These methods may allow for the development of machine learning algorithms in accelerometers [36] and subsequently, the ability to quantify potentially osteogenic exercise more accurately.
A limitation of this study is the relative intensity of PA levels calculated by accelerometry which were based on cut points developed within a healthy young adult population. As a result, PA classified as light or moderate intensity in this study may in fact be considered relatively vigorous amongst older adult populations, potentially influencing the lack of observed associations. In particular, given our study population constituted of relatively healthy community-dwelling older adults, it is likely that these associations are not generalizable to older adults with poorer musculoskeletal health where this potential effect may be more marked. Furthermore, the relatively short period of follow-up between assessments may explain the lack of associations observed, with changes in bone mass at certain sites failing to exceed long-term coefficient of variation of the study. Given no coefficient of variation measures was completed for the arms and leg BMC or BMD, along with substantial longitudinal changes observed at these sites, the precision of DXA measurements at these sites is questionable. Studies with longer follow-up periods and assessment of precision at specific sites are required to clarify associations of PA with changes in bone health. Additionally, 7-day accelerometer assessments may not accurately reflect long-term habitual physical activity. While it is challenging to deploy accelerometers over longer periods, future studies with prolonged or repeated usage of accelerometers may improve our understanding of the relationship between changes in PA and bone health during ageing. Finally, we did not include data on menopause status or hormone replacement therapy in older women in this study. The median age of menopause in Australia is 51 [37], and the median age of women in the present study was 63 years, suggesting the majority of our women were post-menopausal. Furthermore, roughly 11% of Australian women were using hormone replacement therapy during the study period, suggesting this would have limited influence on our results [38]. Nevertheless, menopause status and hormone replacement therapy may have been a confounder in the observed sex-specific associations between PA and BMC and should be assessed in future studies.
In conclusion, height and lean mass mediate sex-specific associations between accelerometer-determined PA and bone health in community-dwelling older adults. Positive cross-sectional associations for steps per day and MVPA were observed in women only, while negative prospective associations for sedentary behaviour were observed in men at clinically relevant fracture sites. These findings suggest that body composition differences may influence mechanical loading benefits of PA in older adults.
References
Australian Institute of Health and Welfare (2014) Estimating the prevalence of osteoporosis in Australia [Internet]. Canberra. Available from: http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129548481
Hannam KJ, Deere KC, Hartley A, Al-Sari UA, Clark EM, Fraser WD et al (2016) Habitual levels of higher, but not medium or low, impact physical activity are positively related to lower limb bone strength in older women: findings from a population-based study using accelerometers to classify impact magnitude. Osteoporos Int [Internet]. 28(10):2813–2822. Available from. https://doi.org/10.1007/s00198-016-3863-5
Warburton DER, Nicol CW, Bredin SSD (2006) Health benefits of physical activity: the evidence. CMAJ [Internet] 174(6):801–809. Available from: http://www.cmaj.ca/content/174/6/801
Goh VHH, Hart WG (2016) Aging, lifestyle factors, hormones and bone health in Singaporean men. Bone Reports [Internet] 5:110–116. Available from. https://doi.org/10.1016/j.bonr.2016.05.003
Lacombe J, Cairns BJ, Green J, Reeves GK, Beral V, Armstrong MEG (2016) The effects of age, adiposity, and physical activity on the risk of seven site-specific fractures in postmenopausal women. J Bone Miner Res 31(8):1559–1568
Adami S, Gatti D, Braga V, Bianchini D, Rossini M (1999) Site-specific effects of strength training on bone structure and geometry of ultradistal radius in postmenopausal women. J bone Miner Res [Internet] 14(1):120–124. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9893073
Kelley GA, Kelley KS, Kohrt WM (2013) Exercise and bone mineral density in men: a meta-analysis of randomized controlled trials. Bone [Internet]. 53(1):103–111. Available from. https://doi.org/10.1016/j.bone.2012.11.031
James P, Weissman J, Wolf J, Mumford K, Contant CK, Hwang WT, Taylor L, Glanz K (2016) Comparing GPS, log, survey, and accelerometry to measure physical activity. Am J Health Behav 40(1):123–131
Ferguson T, Rowlands AV, Olds T, Maher C (2015) The validity of consumer-level, activity monitors in healthy adults worn in free-living conditions: a cross-sectional study. Int J Behav Nutr Phys Act [Internet] 12:42. Available from: http://apps.webofknowledge.com/full_record.do?product=UA&search_mode=GeneralSearch&qid=1&SID=2BbCoX5WP9gddPXAMX5&page=1&doc=9&cacheurlFromRightClick=no
Case MA, Burwick HA, Volpp KG, Patel MS (2015) Accuracy of smartphone applications and wearable devices for tracking physical activity data. J Am Med Assoc [Internet] 313(6):625. Available from: https://jamanetwork.com/journals/jama/fullarticle/2108876
Tudor-Locke C, McClain JJ, Hart TL, Sisson SB, Washington TL (2009) Pedometry methods for assessing free-living youth. Res Q Exerc Sport [Internet] 80(2):175–184. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19650382
Koster A, Caserotti P, Patel KV, Matthews CE, Berrigan D, van Domelen DR et al (2012) Association of Sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One 7(6):1–7
Gianoudis J, Bailey CA, Ebeling PR, Nowson CA, Sanders KM, Hill K, Daly RM (2014) Effects of a targeted multimodal exercise program incorporating high-speed power training on falls and fracture risk factors in older adults: a community-based randomized controlled trial. J Bone Miner Res 29(1):182–191
Johansson J, Nordstrom A, Nordstrom P (2015) Objectively measured physical activity is associated with parameters of bone in 70-year-old men and women. Bone [Internet] 81:72–79. Available from. https://doi.org/10.1016/j.bone.2015.07.001
Gerdhem P, Dencker M, Ringsberg K, Akesson K (2008) Accelerometer-measured daily physical activity among octogenerians: results and associations to other indices of physical performance and bone density. Eur J Appl Physiol 102(2):173–180
Gába A, Kapuš O, Pelclová J, Riegerová J (2012) The relationship between accelerometer-determined physical activity (PA) and body composition and bone mineral density (BMD) in postmenopausal women. Arch Gerontol Geriatr 54(3):e315–e321
Lee I, Ha C, Kang H (2016) Association of sarcopenia and physical activity with femur bone mineral density in elderly women. J Exerc Nutr Biochem [Internet] 20(1):23–28. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27298809
Stillman R, Lohman T, Slaughter M, Massey B (1986) Physical activity and bone mineral content in women aged 30 to 85 years. Med Sci Sport Exerc 18(5):576–580
Trost SG, Mciver KL, Pate RR (2005) Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc 37(11 SUPPL):S531–S543
Matthews CE, Hagströmer M, Pober DM, Bowles HR (2013) Best practices for using physical activity monitors. Med Sci Sports Exerc 44(18):1–17
Matthews CE (2005) Calibration for accelerometer output for adults. Med Sci Sport Exerc [Internet] S512(Supplement):S512–S522. Available from: http://www.scopus.com/inward/record.url?eid=2-s2.0-20544465741&partnerID=tZOtx3y1
Freedson PS, Melanson E, Sirard J (1998) Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sport Exerc. 30(5):777–781
Foley S, Quinn S, Jones G (2010) Pedometer determined ambulatory activity and bone mass: a population-based longitudinal study in older adults. Osteoporos Int 21(11):1809–1816
Allison SJ, Poole KES, Treece GM, Gee AH, Tonkin C, Rennie WJ, Folland JP, Summers GD, Brooke-Wavell K (2015) The influence of high-impact exercise on cortical and trabecular bone mineral content and 3D distribution across the proximal femur in older men: a randomized controlled unilateral intervention. J Bone Miner Res 30(9):1709–1716
Wallace BA, Cumming RG (2000) Systematic review of randomized trials of the effect of exercise on bone mass in pre- and postmenopausal women. Calcif Tissue Int 67(1):10–18
Lanyon LE, Rubin CT (1984) Static vs dynamic loads as an influences on bone remodelling. J Biomech 17(12):897–905
Vainionpää A, Korpelainen R, Sievänen H, Vihriälä E, Leppäluoto J, Jämsä T (2007) Effect of impact exercise and its intensity on bone geometry at weight-bearing tibia and femur. Bone 40(3):604–611
Hinton PS, Nigh P, Thyfault J (2015) Effectiveness of resistance training or jumping-exercise to increase bone mineral density in men with low bone mass: a 12-month randomized, clinical trial. Bone [Internet]. 79:203–212. Available from: http://linkinghub.elsevier.com/retrieve/pii/S8756328215002446
Rhodes EC, Martin AD, Taunton JE, Donnelly M, Warren J, Elliot J (2000) Effects of one year of resistance training on the relation between muscular strength and bone density in elderly women. Br J Sports Med [Internet] 34(1):18–22. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1724140/
Watson SL, Weeks BK, Weis LJ, Harding AT, Horan SA, Beck BR (2017) High-intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with osteopenia and osteoporosis: the LIFTMOR Randomized Controlled Trial. J Bone Miner Res [Internet]. Available from: http://doi.wiley.com/10.1002/jbmr.3284
Kohrt WM, Barry DW, Schwartz RS (2009) Muscle forces or gravity: what predominates mechanical loading on bone? Med Sci Sport Exerc. 41(11):2050–2055
Popp KL, McDermott W, Hughes JM, Baxter SA, Stovitz SD, Petit MA (2017) Bone strength estimates relative to vertical ground reaction force discriminates women runners with stress fracture history. Bone [Internet] 94:22–28. Available from. https://doi.org/10.1016/j.bone.2016.10.006
Chastin SFM, Mandrichenko O, Helbostadt JL, Skelton DA (2014) Associations between objectively-measured sedentary behaviour and physical activity with bone mineral density in adults and older adults, the NHANES study. Bone [Internet] 64:254–262. Available from. https://doi.org/10.1016/j.bone.2014.04.009
Gómez-Bruton A, González-Agüero A, Gómez-Cabello A, Matute-Llorente A, Casajús JA, Vicente-Rodríguez G (2016) Swimming and bone: is low bone mass due to hypogravity alone or does other physical activity influence it? Osteoporos Int [Internet] 27(5):1785–1793. Available from. https://doi.org/10.1007/s00198-015-3448-8
Deere KC, Hannam KJ, Coulson J, Ireland A, McPhee JS, Moss C et al (2016) Quantifying habitual levels of physical activity according to impact in older people: accelerometry protocol for the VIBE study. J Aging Phys Act 24(2):290–295
Ellis K, Kerr J, Godbole S, Staudenmeyer JW, Lanckriet G (2016) Hip and wrist accelerometer algorithms for free-living behavior classification. Med Sci Sports Exerc 48(5):933–940
Do K, Treloar SA, Pandeya N, Purdie D, Green C, Heath AC et al (1998) Predictive factors of age at menopause in a large Australian twin study. Hum Biol 70(6):1073–1091
Australian Bureau of Statistics (2006) National Health Survey: summary of results [Internet]. Canberra. Available from: http://www.ausstats.abs.gov.au/Ausstats/subscriber.nsf/0/3B1917236618A042CA25711F00185526/$File/43640_2004-05.pdf
Acknowledgements
We gratefully acknowledge the efforts of the TASOAC participants and staff, particularly study coordinator Catrina Boon. DS, GJ and DA wish to acknowledge fellowship support from the National Health and Medical Research Council of Australia. LBM was supported by an Australian Postgraduate Award.
Funding
This work was supported by the National Health and Medical Research Council of Australia, Arthritis Foundation of Australia, Tasmanian Community Fund, and University of Tasmania Institutional Research Grants Scheme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all participants.
Additional information
Graeme Jones and David Scott are joint senior authors.
Rights and permissions
About this article
Cite this article
McMillan, L.B., Aitken, D., Ebeling, P. et al. The relationship between objectively assessed physical activity and bone health in older adults differs by sex and is mediated by lean mass. Osteoporos Int 29, 1379–1388 (2018). https://doi.org/10.1007/s00198-018-4446-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4446-4