Abstract
Summary
This study evaluates cytokines production in bone and bone marrow of patients with an osteoporotic fracture or with osteoarthritis by real time PCR, Western blot and immunohistochemistry. We demonstrate that the cytokine pattern is shifted towards osteoclast activation and osteoblast inhibition in patients with osteoporotic fractures.
Introduction
Fragility fractures are the resultant of low bone mass and poor bone architecture typical of osteoporosis. Cytokines involved in the control of bone cell maturation and function are produced by both bone itself and bone marrow cells, but the roles of these two sources in its control and the amounts they produce are not clear. This study compares their production in patients with an osteoporotic fracture and those with osteoarthritis.
Methods
We evaluated 52 femoral heads from women subjected to hip-joint replacement surgery for femoral neck fractures due to low-energy trauma (37), or for osteoarthritis (15). Total RNA was extracted from both bone and bone marrow, and quantitative PCR was used to identify the receptor activator of nuclear factor kB Ligand (RANKL), osteoprotegerin (OPG), macrophage colony stimulating factor (M-CSF), transforming growth factor β (TGFβ), Dickoppf-1 (DKK-1) and sclerostin (SOST) expression. Immunohistochemistry and Western blot were performed in order to quantify and localize in bone and bone marrow the cytokines.
Results
We found an increase of RANKL/OPG ratio, M-CSF, SOST and DKK-1 in fractured patients, whereas TGFβ was increased in osteoarthritic bone. Bone marrow produced greater amounts of RANKL, M-CSF and TGFβ compared to bone, whereas the production of DKK-1 and SOST was higher in bone.
Conclusions
We show that bone marrow cells produced the greater amount of pro-osteoclastogenic cytokines, whereas bone cells produced higher amount of osteoblast inhibitors in patients with fragility fracture, thus the cytokine pattern is shifted towards osteoclast activation and osteoblast inhibition in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone turnover is due to continuous and cyclic bone resorption followed by apposition owing to the coordinated actions of osteoclasts (OC, which destroy bone) and osteoblasts (OB, which form bone), orchestrated to some extent by osteocytes. In physiological conditions, these actions are balanced and resorption is offset by formation; whereas in pathological conditions or during senescence, resorption exceeds formation. Fragility fractures are the resultant of low bone mass and poor bone architecture due to different pharmacological treatments or pathological conditions, such as glucocorticoid [1], anti-hormonal treatments [2], and osteoporosis [3]. Osteoporotic fractures cause significant morbidity in the middle-age and elderly population: more than two million fragility fractures occur each year, almost 300,000 of them are hip fractures associated with a threefold risk for future fractures, as well as a 15% to 33% mortality rate within the first year of fracture [4]. In fragility fractures, OC activity is up-regulated [5], mainly by the increase in pro-osteoclastogenic cytokines [6, 5, 7]. Cytokines involved in bone cell regulation are produced by both bone itself and bone marrow cells, but the roles of these two sources in pathological condition such as fragility fracture and the amounts they produce are not clear [6]. Those mostly involved in the control of OC differentiation and function are macrophage colony stimulating factor (M-CSF), receptor activator of nuclear factor kB ligand (RANKL) and osteoprotegerin (OPG) [7]. M-CSF induces the proliferation and differentiation of OC precursors, and increases the survival of mature OCs [5, 8]; RANKL promotes the differentiation of OC precursors into mature multinucleated OCs, stimulates their bone resorption, and decreases their apoptosis [9].
OPG is the RANKL neutralizing soluble decoy receptor [10]. Imbalance between RANKL and OPG has been indicated as the pivotal mechanism responsible for bone loss in cases of estrogen deficiency [5, 9], inflammation [11–13] and cancer [14, 15].
Wnts proteins (a family of secreted lipid-modified proteins that bind to a receptor complex: reviewed in Macsai et al. [16]) play an essential role in OB biology, canonical Wnt signaling is a critical determinant in maintaining bone mass, indeed, loss or gain of function mutations in its receptor leads to the osteoporosis-pseudoglioma syndrome [17] or the hereditary high bone mass trait [18], respectively. Several molecules serve as antagonists of Wnt signaling. The two most studied—Dickkopf 1 (DKK-1) and sclerostin (SOST) [16]—are thought to be involved in the pathogenesis of arthritis [19, 20], glucocorticoid-induced osteoporosis [21, 22], and disuse osteoporosis [23].
TGFβ plays a complex role in the regulation of bone turnover. It has wide-ranging effects and may be of substantial importance in the growing skeleton by contributing to the coupling between OB and OC [24], as well as in fracture healing [25–27]. It is produced by bone marrow cells, OBs and stromal cells. Both in vitro and in vivo studies have shown that TGFβ either stimulates or represses OB and OC proliferation or formation, depending on the cell types and culture conditions used.
Here, we demonstrate that in fragility fracture the bone marrow is the main source of cytokines active in the regulation of osteoclastogenesis, whereas the Wnts pathway inhibitors are primarily expressed by bone cells. We also demonstrate that both cytokines that enhance OC activity and those that reduce OB activity are up-regulated in fractured, with respect to osteoarthritis (OA), patients.
Methods
The study was approved by the “Clinical Study Review Committee” of the Hospital San Giovanni Battista of Torino, and all the patients signed an informed consent statement prior to recruitment.
Fifty-two femoral heads were obtained during hip-joint replacement surgery indicated for femoral neck fractures due to low-energy trauma (37 women) or for OA (15 women). None were on calcium and vitamin D, thyroid hormones, corticosteroids, estrogen, bisphosphonates, strontium ranelate, parathyroid hormone or raloxifene. Secondary osteoporosis was ruled out by reference to the medical history and by physical examination and blood tests.
Risk factors for osteoporosis and previous bone density test were evaluated by a questionnaire [28]. When bone density test was available OA patients were included in the study only if the test results in the normal range (>−1.5 SD according to the WHO criteria [29]).
Sample preparation
The femoral heads were immediately processed. Bone was minced manually and washed with PBS and trypsin to remove bone marrow cells. Bone marrow red blood cells were lysed and the remaining cells were frozen at −80°C until RNA extraction.
Bone fragments were treated with RNA later (Ambion, Huntingdon, UK) to preserve RNA from degradation, than decalcified in EDTA for a week. They were then homogenized with a homogenator (Ultra-Turrax T8 IKA Werke GMBH & CO. KG, Staufen, Germany) in TRIzol reagent (Ambion), and frozen at −20°C until RNA extraction.
Real time RT-PCR
Total RNA was isolated by using TRIzol reagent, chloroform extraction, and subsequent isopropanol precipitation according to the manufacturer's protocol, and purified with the RecoverAll Total Nucleic Acid Isolation Kit (Ambion). One microliter was converted up to single-stranded cDNA with the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Warrington, UK). cDNA was stored at −20°C until use. Quantitative RT-PCR (RQ-PCR) analysis was performed by the iCycler iQ™ system (Bio Rad, Hercules, CA, USA). TaqMan probes were designed using Primer Express v2.0 software and synthesized by Applied Biosystems. The sequences of the probes and primers are listed in the on-line supplemental table. The expression of β-Actin was utilized to normalize RT-PCR data. All the probes were labeled at the 5′ end with 6-carboxy fluorescein (FAM) and the 3′ end with 6-carboxy-tetrametil rhodamine (TAMRA). Reactions for gene quantification were performed in a 25-μl final volume with 2 μl of sample cDNA, 1× iQ Supermix (Bio Rad, Hercules, CA, USA), 0.3 μM of each primer and 0.4 μM of the probes. PCR primers were the same used for gene cloning. The amplification conditions for quantization were: 95°C for 15 min, 50 cycles at 95°C for 15 s, 58°C for 1 min.
Immunohistochemistry
To confirm the RQ-PCR data, immunohistochemistry for the analyzed molecules was performed on paraffin sections from five femoral heads. The following antibodies were used: anti-RANKL mouse mAb (AbCam, Cambridge, UK), anti-MCSF rabbit mAb (AbCam), anti-SOST rabbit polyclonal Ab (AbCam), anti-TGFβ mouse mAb (AbCam), anti-OPG mouse mAb (Santa Cruz Biotechnology, Inc, Santa Cruz, CA), and anti-DKK-1 mouse mAb (Abnova, Taipei, Taiwan).
Sections were stained with the primary Abs according to the manufacturer's protocol, and incubated overnight at 4°C in a humidified atmosphere. Reactivity of antibody was detected by ABC method (Santa Cruz). Sections were counterstained with Mayer's hematoxylin for 5–10 s, transferred in tap water, dehydrated, cleared in xylene, and mounted.
Western blot
Contemporary to RNA extraction, protein extraction were performed, briefly TRIzol supernatant was washed in isopropanol and ethanol to separate proteins, the pellet was frozen at −80°C until measurement was done. In order to quantify the immunohistochemistry data on protein expression, we carried on a Western blot analyses on ten patients and ten controls. Briefly, 50 μg of protein were loaded onto each lane, and proteins were resolved by 12% SDS-PAGE. The separated proteins were transferred onto Immobilon-P membranes (Millipore Corp.) by electroblotting overnight. Membranes were incubated in the presence of anti-RANKL mouse mAb (AbCam, Cambridge, UK), or anti-MCSF rabbit mAb (AbCam), or anti-SOST rabbit polyclonal Ab (AbCam), or anti-TGFβ mouse mAb (AbCam), or anti-OPG mouse mAb (Santa Cruz Biotechnology, Inc, Santa Cruz, CA), or anti-DKK-1 mouse mAb (Abnova, Taipei, Taiwan) at 1:1,000 dilution and 5% milk powder for 60 min. The membranes were washed and incubated in proper secondary antibody at 1:4,000 in 5% milk powder for 60 min, washed, and the intensity of the bands enhanced using chemiluminescence mediated by horseradish peroxidase catalysis of luminol (Amersham) followed by exposure to Kodak Biomax-Ml film (Eastman Kodak Co.). Protein concentration was determined by spectrophotometric method (Bio-Rad).
Equal protein loading was confirmed by measuring total actin. The bands were quantified using scanning laser densitometry.
Statistics
Fractured and OA patients’ baseline characteristics were compared by means of one-way ANOVA or chi-square test after Yates correction for non continuous variables. The normal distribution of measured parameter was determined with Kurtosis. Since none of the genes analyzed were normally distributed, fractured and OA patients were compared by means of the Mann–Whitney U test after weight for age, proteins were normally distributed; hence, fractured and OA patients were compared by means of unpaired T test. Age and gene expression were correlated by means of Spearman's test. Genes measured in bone and bone marrow were compared by means of Wilcoxon's test. The SPSS 17.0 software package was used to process the data with p < 0.05 as the significance cut-off.
Results
Patients
Correct classification of fractured patients as osteoporotic and of OA patients as non osteoporotic was ensured by previous bone density test in a majority of subject (79%). The higher prevalence of previous fragility fracture in fractured patients confirm the correct patient's classification (27% vs 13%, p = 0.026).
Fractured patients were significantly older than OA ones (83 ± 9 vs 74 ± 10, p = 0.000), hence a correction for age was carried on in the subsequent analyses.
Body mass index, post menopausal period, calcium intake, smoking and familiar history of fragility fractures were recorded as risk factors for osteoporosis [28]; among these, only familiar history of fragility fractures was more frequent in fractured than in OA patients (24% vs 7%, p = 0.002).
Cytokines and aging
Age was weakly correlated with RANKL expression in bone marrow. (R = 0.38, p = 0.009). This result is in keeping with the well-known effect of aging on bone loss due to a progressive increase in osteoclast formation and activity [5, 9].
Pro-osteoclastogenic cytokines are elevated in fractured patients
The data in Fig. 1a show that RANKL/OPG is significantly higher in the bone marrow of fractured as opposed to OA patients, whereas it is not significantly different in bone (Fig. 1b). Figure 1c and d show that both RANKL and OPG are higher in the bone marrow of fractured patients; whereas in bone, this difference is not significant (data not shown). RANKL/OPG was calculated as the ratio between RANKL and OPG expression.
RANKL/OPG is higher in fractured patients. a Box and whisker plot represent RANKL/OPG measured in bone marrow in fractured compared to OA patients. The p value indicated was calculated with the Mann–Whitney U test after correction for age. b As in a: RANKL/OPG measured in bone. c As in a: RANKL measured in bone marrow. d As in a: OPG measured in bone marrow. Each box represents the 25th to 75th percentiles. Lines outside the boxes represent the minimum and maximum values. Lines inside the boxes represent the medians calculated for all the data set
To determine whether RANKL is mainly produced by bone marrow or bone, we compared these two sources in the same patient. Figure 2a shows that more RANKL is produced by bone marrow. The immunohistochemistry findings are in keeping with the production of RANKL by both bone and bone marrow (Fig. 2b).
Bone marrow produces more RANKL than bone. a Box and whisker plot represent RANKL measured in bone marrow and in bone of all the samples. The p value indicated was calculated by means of Wilcoxon's test. b Micrograph displays immunohistochemistry for RANKL. Arrows indicate positive osteocytes; arrowheads indicate positive bone marrow cells (magnification ×60). c As in a: OPG measured in bone marrow and bone of all the samples. d Micrograph displays immunohistochemistry for OPG. Arrows indicate positive osteocytes; arrowheads indicate positive bone marrow cells (magnification ×60). Each box represents the 25th to 75th percentiles. Lines outside the boxes represent the minimum and maximum values. Lines inside the boxes represent the medians calculated for all the data set
OPG was equally expressed by bone and bone marrow (Fig. 2c, d).
M-CSF is a key molecule in OC formation, even if osteoclastogenesis does not occur in the absence of RANKL. Its expression in bone was not significantly different in fractured and OA patients (Fig. 3c). In bone marrow we found an albeit non significant higher expression of M-CSF in fractured than in OA patients (Fig. 3d). The major expression of M-CSF was found in bone marrow (Fig. 3a, b).
Bone marrow produces more M-CSF than bone. a Box and whisker plot represent M-CSF measured in bone marrow and in bone of all the samples. The p value indicated was calculated by means of Wilcoxon's test. b Micrograph displays immunohistochemistry for M-CSF. Arrows indicate positive osteocytes; arrowheads indicate positive bone marrow cells (magnification ×60). Each box represents the 25th to 75th percentiles. Lines outside the boxes represent the minimum and maximum values. Lines inside the boxes represent the medians calculated for all the data set
Anti-osteoblastogenic cytokines are elevated in fractured patients
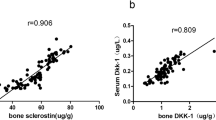
Expression of DKK-1, albeit low, was higher in the fractured patients, both in bone (Fig. 4a) and in bone marrow (Fig. 4b), while its production by bone cells was greater (Fig. 4c, d).
DKK-1 production in bone and bone marrow from fractured and OA patients. a Box and whisker plot represents DKK-1 measured in bone in fractured as respect to OA patients. The p value indicated was calculated by means of Mann–Whitney U test after correction for age. b As in a: DKK-1 measured in bone marrow. c Box and whisker plot represent DKK-1 measured in bone marrow and bone of all the samples. The p value indicated was calculated by means of Wilcoxon's test. d Micrograph displays immunohistochemistry for DKK-1. Arrows indicate positive osteocytes; arrowheads indicate positive bone marrow cells (magnification ×60). Each box represents the 25th to 75th percentiles. Lines outside the boxes represent the minimum and maximum values. Lines inside the boxes represent the medians calculated for all the data set
Production of SOST was similar in both sets of patients (data not shown) and greater in bone (Fig. 5a, b).
Bone produces more SOST than bone marrow. a. Box and whisker plot represent SOST measured in bone marrow and in bone of all the samples. The p value indicated was calculated by means of Wilcoxon's test. b. Micrograph displays immunohistochemistry for SOST. Arrows indicate positive osteocytes; arrowheads indicate positive bone marrow cells (magnification ×60). Each box represents the 25th to 75th percentiles. Lines outside the boxes represent the minimum and maximum values. Lines inside the boxes represent the medians calculated for all the data set
Bone production of TGFβ is higher in OA than in fractured patients
The role of TGFβ in controlling bone turnover is not completely clear. According to literature bone marrow cells were the main source of TGFβ (Fig. 6a, b) with no significant difference between the two sets of patients (data not shown), whereas its production by bone was slightly (about 1.5%) greater in the OA set (Fig. 6c).
TGFβ production in bone and bone marrow from fractured and OA patients. a Box and whisker plot represents TGFβ measured in bone marrow and in bone of all the samples. The p value indicated was calculated by means of Wilcoxon's test. b Micrograph displays immunohistochemistry for TGFβ. Arrows indicate positive osteocytes; arrowheads indicate positive bone marrow cells (magnification ×60). c Box and whisker plot represents TGFβ measured in bone in fractured as compared to OA patients. The p value indicated was calculated by means of the Mann–Whitney U test after correction for age. Each box represents the 25th to 75th percentiles. Lines outside the boxes represent the minimum and maximum values. Lines inside the boxes represent the medians calculated for all the data set.
Protein expression
The Western blot confirms the data obtained by RQ-PCR on the higher expression of RANKL, OPG, and DKK-1 in fractured than in OA patients, and on the higher expression of TGFβ in OA ones (Supplemental material). Moreover, M-CSF and SOST proteins are significantly higher in fractured than in OA patients; this is in keeping with a bone-wasting cytokine profile in patients with fragility fracture as respect to patients with OA.
Discussion
Decreased bone mass and increased fragility are the hallmarks of osteoporosis, and cause a significant morbidity in the affected population. In fragility fractures, OC activity is up-regulated [5], mainly by the increase in pro-osteoclastogenic cytokines [5, 7], but the role of bone marrow and bone in the production of these cytokines is not completely clear.
This study investigates the production of cytokines involved in the control of bone cells in fragility fracture and OA patients. We assessed bone and bone marrow cytokines production and investigate their function in regulating bone cells. Since we could not obtain hip samples from normal individuals, we cannot compare our results with those in a completely normal skeleton, but we used OA patients, previously controlled for the absence of osteoporosis. We observed a positive correlation between bone marrow RANKL and age, this datum confirms previous literature on the role of RANKL in the age-related bone loss [9, 30].
Our data show that bone marrow cells are mainly responsible for the production of osteoclastogenic cytokines (M-CSF and RANKL), whereas OB inhibitors (DKK-1 and SOST) are mainly produced by bone cells. This finding is in keeping with the close relationship between bone and bone marrow in the regulation of bone cells.
We observed a substantial increase in both RANKL and OPG, as well as in the RANKL/OPG ratio in the bone marrow of fractured compared to OA patients, as reported by Eghbali-Fatourechi et al. [9] for the early post-menopause, whereas this parameter was similar in the bone of both sets of patients, showing the minor role of bone in producing these cytokines. The increase in OPG may be interpreted as an attempt to inhibit RANKL, and as a sign of increased bone turnover [7, 31]. Thus our data corroborate the hypothesis that bone marrow cells are the main drivers of OC formation and activity at least in patients with fragility fracture.
The M-CSF expression in bone was low and not different among fractured and OA patients, whereas in bone marrow it was increased in fractured patients. These results mirror the M-CSF activity, mainly active in bone marrow, where it is produced and promotes the survival and proliferation of osteoclast precursors [32]. Moreover, the higher expression in fractured than in OA patients is according to previously published data, which showed a pro-osteoclastogenic cytokine profile in fragility fractures [5, 6].
This pro-osteoclastogenic cytokine profile was accompanied by an increase in the Wnt pathway inhibitors DKK-1 and SOST, which reduce OB activity in fractured patients. This finding corroborates Velasco et al.'s observation of down-regulation of the Wnt pathway in osteoporotic as opposed to OA patients [33]. Thus our data, according to this study [33], suggests that osteoporotic fractures might be regarded not only as a disease caused by an increased OC activity, but also depending on an OB activity reduction. This hypothesis might open perspectives for new osteoporosis treatments (further PTH) addressed to increase or stimulate OB activity instead of acting only on the inhibition of OC activity.
There was a small increase in the bone TGFβ production of our OA patients, whereas bone marrow TGFβ was not different in the two groups, it has been demonstrated that OA chondrocytes produce more TGFβ (reviewed in [34]), and that this increase may be regarded as an important pathogenetic moment of OA. The small TGFβ increase in the bone sample from OA patients in our cohort may be due to a chondrocytes contamination of bone samples.
The main limit of this study is the patients' selection as some patients do not have bone density test performed and serum vitamin D level was not measured, anyway the majority of our subjects had a previous bone densitometry and the incidence of previous fragility fracture confirmed our patients' classification. As regards vitamin D level, it is well known that hypovitaminosis D is highly prevalent among elderly even in the absence of fracture [35, 36], hence it is reasonable to hypothesize an equal low level of vitamin D amongst fractured and OA patients.
Another limit of the study is the use of bone from OA patients and not of healthy controls, it is well known that OA subjects could not be considered as pure controls as their condition is associated with cytokine unbalance [37].
In summary, we demonstrated that bone and bone marrow display a cytokine pattern shifted towards OC activation and OB inhibition in patients with fragility fractures. In particular, bone marrow cells contribute strongly in the regulation of osteoclastogenesis and in the increase of Wnts pathway inhibitors production by bone from fragility fracture patients.
References
Lane NE, Yao W (2010) Glucocorticoid-induced bone fragility. Ann N Y Acad Sci 1192:81–83
Bertoldo F, Pancheri S, Zenari S, Boldini S (2010) Emerging drugs for the management of cancer treatment induced bone loss. Expert Opin Emerg Drugs 15:323–342
National Institutes of Health (1984) Osteoporosis. National Institutes of Health Consensus Development Conference Statement. Natl Inst Health Consens Dev Conf Consens Statement 5(3):1–6
Ekman EF (2010) The role of the orthopaedic surgeon in minimizing mortality and morbidity associated with fragility fractures. J Am Acad Orthop Surg 18:278–285
D'Amelio P, Grimaldi A, Di Bella S, Brianza SZ, Cristofaro MA, Tamone C, Giribaldi G, Ulliers D, Pescarmona GP, Isaia G (2008) Estrogen deficiency increases osteoclastogenesis up-regulating T cells activity: a key mechanism in osteoporosis. Bone 43:92–100
D'Amelio P, Isaia G (2009) Immune system and postmenopausal bone loss. CRBMM 7:261–267
Hofbauer LC, Kuhne CA, Viereck V (2004) The OPG/RANKL/RANK system in metabolic bone diseases. J Musculoskelet Neuronal Interact 4:268–275
Seitz M, Loetscher P, Fey MF, Tobler A (1994) Constitutive mRNA and protein production of macrophage colony-stimulating factor but not of other cytokines by synovial fibroblasts from rheumatoid arthritis and osteoarthritis patients. Br J Rheumatol 33:613–619
Eghbali-Fatourechi G, Khosla S, Sanyal A, Boyle WJ, Lacey DL, Riggs BL (2003) Role of RANK ligand in mediating increased bone resorption in early postmenopausal women. J Clin Invest 111:1221–1230
Grundt A, Grafe IA, Liegibel U, Sommer U, Nawroth P, Kasperk C (2009) Direct effects of osteoprotegerin on human bone cell metabolism. Biochem Biophys Res Commun 389:550–555
Shigeyama Y, Pap T, Kunzler P, Simmen BR, Gay RE, Gay S (2000) Expression of osteoclast differentiation factor in rheumatoid arthritis. Arthritis Rheum 43:2523–2530
Leibbrandt A, Penninger JM (2009) RANKL/RANK as key factors for osteoclast development and bone loss in arthropathies. Adv Exp Med Biol 649:100–113
Appel H, Loddenkemper C, Miossec P (2009) Rheumatoid arthritis and ankylosing spondylitis—pathology of acute inflammation. Clin Exp Rheumatol 27:S15–S19
Roato I, D'Amelio P, Gorassini E, Grimaldi A, Bonello L, Fiori C, Delsedime L, Tizzani A, De Libero A, Isaia G, Ferracini R (2008) Osteoclasts are active in bone forming metastases of prostate cancer patients. PLoS ONE 3:e3627
Roato I, Gorassini E, Buffoni L, Lyberis P, Ruffini E, Bonello L, Baldi I, Ciuffreda L, Mussa A, Ferracini R (2008) Spontaneous osteoclastogenesis is a predictive factor for bone metastases from non-small cell lung cancer. Lung Cancer 61:109–116
Macsai CE, Foster BK, Xian CJ (2008) Roles of Wnt signalling in bone growth, remodelling, skeletal disorders and fracture repair. J Cell Physiol 215:578–587
Marques-Pinheiro A, Levasseur R, Cormier C, Bonneau J, Boileau C, Varret M, Abifadel M, Allanore Y (2010) Novel LRP5 gene mutation in a patient with osteoporosis-pseudoglioma syndrome. Joint Bone Spine 77(2):151–153
Frost M, Andersen TE, Yadav V, Brixen K, Karsenty G, Kassem M (2010) Patients with high bone mass phenotype due to Lrp5-T253I mutation have low plasma levels of serotonin. J Bone Miner Res 25(3):673–675
Appel H, Ruiz-Heiland G, Listing J, Zwerina J, Herrmann M, Mueller R, Haibel H, Baraliakos X, Hempfing A, Rudwaleit M, Sieper J, Schett G (2009) Altered skeletal expression of sclerostin and its link to radiographic progression in ankylosing spondylitis. Arthritis Rheum 60:3257–3262
Diarra D, Stolina M, Polzer K, Zwerina J, Ominsky MS, Dwyer D, Korb A, Smolen J, Hoffmann M, Scheinecker C, van der Heide D, Landewe R, Lacey D, Richards WG, Schett G (2007) Dickkopf-1 is a master regulator of joint remodeling. Nat Med 13:156–163
Ohnaka K, Tanabe M, Kawate H, Nawata H, Takayanagi R (2005) Glucocorticoid suppresses the canonical Wnt signal in cultured human osteoblasts. Biochem Biophys Res Commun 329:177–181
Ohnaka K, Taniguchi H, Kawate H, Nawata H, Takayanagi R (2004) Glucocorticoid enhances the expression of dickkopf-1 in human osteoblasts: novel mechanism of glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun 318:259–264
Lin C, Jiang X, Dai Z, Guo X, Weng T, Wang J, Li Y, Feng G, Gao X, He L (2009) Sclerostin mediates bone response to mechanical unloading through antagonizing Wnt/beta-catenin signaling. J Bone Miner Res 24:1651–1661
Massague J (1990) The transforming growth factor-beta family. Annu Rev Cell Biol 6:597–641
Bostrom MP (1998) Expression of bone morphogenetic proteins in fracture healing. Clin Orthop Relat Res 355:S116–S123
Meyer RA Jr, Meyer MH, Tenholder M, Wondracek S, Wasserman R, Garges P (2003) Gene expression in older rats with delayed union of femoral fractures. J Bone Joint Surg Am 85-A:1243–1254
D'Amelio P, Cristofaro MA, Grimaldi A, Ravazzoli M, Pluviano F, Grosso E, Pescarmona GP, Isaia GC (2010) The role of circulating bone cell precursors in fracture healing. Calcif Tissue Int 86:463–469
D'Amelio P, Tamone C, Pluviano F, Di Stefano M, Isaia G (2005) Effects of lifestyle and risk factors on bone mineral density in a cohort of Italian women: suggestion for a new decision rule. Calcif Tissue Int 77:72–78
National Institutes of Health (2000) Osteoporosis prevention, diagnosis, and therapy. NIH Consens Statement 17:1–45
Leibbrandt A, Penninger JM (2009) RANK(L) as a key target for controlling bone loss. Adv Exp Med Biol 647:130–145
Dobnig H, Hofbauer LC, Viereck V, Obermayer-Pietsch B, Fahrleitner-Pammer A (2006) Changes in the RANK ligand/osteoprotegerin system are correlated to changes in bone mineral density in bisphosphonate-treated osteoporotic patients. Osteoporos Int 17:693–703
Ross FP, Teitelbaum SL (2005) alphavbeta3 and macrophage colony-stimulating factor: partners in osteoclast biology. Immunol Rev 208:88–105
Velasco J, Zarrabeitia MT, Prieto JR, Perez-Castrillon JL, Perez-Aguilar MD, Perez-Nunez MI, Sanudo C, Hernandez-Elena J, Calvo I, Ortiz F, Gonzalez-Macias J, Riancho JA (2009) Wnt pathway genes in osteoporosis and osteoarthritis: differential expression and genetic association study. Osteoporos Int 21:109–118
Pujol JP, Chadjichristos C, Legendre F, Bauge C, Beauchef G, Andriamanalijaona R, Galera P, Boumediene K (2008) Interleukin-1 and transforming growth factor-beta 1 as crucial factors in osteoarthritic cartilage metabolism. Connect Tissue Res 49:293–297
Corino A, D'Amelio P, Gancia R, Del Rizzo P, Gabasio S, Limone P, Isaia G (2007) Hypovitaminosis D in internal medicine inpatients. Calcif Tissue Int 80:76–80
Isaia G, Giorgino R, Rini GB, Bevilacqua M, Maugeri D, Adami S (2003) Prevalence of hypovitaminosis D in elderly women in Italy: clinical consequences and risk factors. Osteoporos Int 14:577–582
Bondeson J, Blom AB, Wainwright S, Hughes C, Caterson B, van den Berg WB (2010) The role of synovial macrophages and macrophage-produced mediators in driving inflammatory and destructive responses in osteoarthritis. Arthritis Rheum 62:647–657
Funding sources
This study was supported by the Stroeder-SIOMMMS Young Investigator Award, by a grant from the Cassa di Risparmio di Torino (CRT) and by a grant from the Ministry for Education, the Universities and Research (MIUR).
PD and FS were supported by a fellowship from the Regione Piemonte.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental figure
Proteins expression in bone and bone marrow from fractured and OA patients. a Western blot analyses display of RANKL, TGFβ, M-CSF, SOST, OPG and DKK-1 expression in samples from fractured (lanes 1 to 5) and OA (lanes 6 to 10). Actin was used as control. The shown blot was obtained in bone marrow samples. b Graph represents the expression of measured cytokines in fractured and OA patients' bone marrow. Bars represent mean and SD expressed as optical density (O.D.). Asterisk is a p value = 0.000 and was calculated by means of Student's T test. c As in b, cytokines measured in bone, Single asterisk is a p value = 0.001. d As in b, cytokines measured in bone compared to those measured in bone marrow, white circle is a p value = 0.03 (PPT 465 kb)
Supplemental table
Gene probe and primer sequences. P, probe; F, forward; R, reverse. All the probes were labeled at the 5′ end with 6-carboxy fluorescein (FAM) and the 3′ end with 6-carboxy-tetramethyl rhodamine (TAMRA), the annealing temperature was always 58°C (DOC 27 kb)
Rights and permissions
About this article
Cite this article
D’Amelio, P., Roato, I., D’Amico, L. et al. Bone and bone marrow pro-osteoclastogenic cytokines are up-regulated in osteoporosis fragility fractures. Osteoporos Int 22, 2869–2877 (2011). https://doi.org/10.1007/s00198-010-1496-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1496-7