Abstract
Summary
The bone metabolic abnormalities in patients with obstructive sleep apnea (OSA) were examined. Severity-dependent increases in the serum/urinary levels of bone resorption markers and their attenuation following continuous positive airway pressure therapy in subjects with OSA provide the first evidence of a link between OSA and abnormal bone metabolism.
Introduction
Hypoxia, microinflammation and oxidative stress, well-known pathophysiological features of obstructive sleep apnea (OSA), are also known to affect bone metabolism. We examined the bone metabolic abnormalities in patients with OSA and also the effects of continuous positive airway pressure (CPAP) therapy on these abnormalities.
Methods
A cross-sectional and prospective study was conducted in 50 consecutive male subjects visiting a sleep clinic and 15 age-matched control subjects without OSA. Plasma concentrations of IL-1β, IL-6, TNF-alfa, 3-nitrotyrosine, osteocalcin, bone-specific alkaline phosphatase (BAP), and urinary concentrations of cross-linked C-terminal telopeptide of type I collagen (CTX) were examined before and after 3 months’ CPAP in subjects with OSA.
Results
The plasma levels of the cytokines as well as the urinary CTX levels were higher in subjects with severe OSA than in those with mild OSA or control subjects. Significant decrease of the urinary excretion of CTX (before: 211 ± 107 vs. after: 128 ± 59 μg/mmol/creatinine; p < 0.01) as well as of the plasma levels of the cytokines was observed following 3 months’ CPAP.
Conclusions
Severity-dependent increases in the serum/urinary levels of bone resorption markers and their reversal following CPAP in subjects with OSA provide the first evidence of a link between OSA and abnormal bone metabolism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a disorder of increasing prevalence that is characterized by repetitive episodes of upper airway collapse or narrowing causing intermittent oxygen desaturation during sleep. Accumulating evidence has implicated OSA in the pathogenesis of cardiovascular diseases, such as hypertension, ischemic heart disease and congestive heart failure [1–3]. Although the mechanisms linking OSA to systemic cardiovascular diseases are not yet completely understood, recent studies have suggested the involvement of multiple factors, including oxidative stress, inflammation, endothelial dysfunction, increased sympathetic activity and metabolic abnormalities [2–4]. Continuous positive airway pressure (CPAP) therapy has been shown to partially prevent the systemic adverse events associated with the intermittent hypercapnea, hypoxia and subsequent reoxygenation in OSA patients, and to, thereby, decrease the cardiovascular morbidity and mortality in these patients [5–9].
Given the high prevalence of OSA [10] and its association with multiple systemic pathological changes, it was considered likely that OSA may also have a substantial impact on other metabolic disorders. The fact that inflammatory cytokines and oxidative stress, as well as hypoxia itself, are known to affect bone cell function and may be considered as risk factors for osteoporosis [11–15] led us to hypothesize that OSA may also predispose to or exacerbate osteoporosis by causing abnormalities of bone metabolism.
As an initial step to test our hypothesis, in the present study, we examined the association between the severity of OSA and the biochemical markers of bone metabolism in consecutive male subjects visiting a sleep clinic for the evaluation of sleep disorders, and also tested the effect of CPAP therapy in a prospective manner. The results demonstrated that severe OSA was associated with increased bone resorption, which was reversed by CPAP therapy. To the best of our knowledge, this is the first clinical indication of the adverse effects of OSA on bone metabolism.
Methods
Subjects
Fifty-three consecutive male subjects were admitted to the Tokyo Medical University Hospital between November 2005 and June 2006 for diagnostic assessment of sleep disorders. Most of them were suspected to have a sleep disorder based on assessment by a portable sleep monitor at the outpatient department of the hospital before the admission. In the assessment of sleep disorders, apnea was defined as a continuous cessation of airflow for ≥10 seconds, and hypopnea as a ≥50% reduction in airflow for more than 10 seconds with an oxygen desaturation of ≥3%. Obstructive apnea/hypopnea was defined as apnea/hypopnea in the presence of thoraco-abdominal effort, and central apnea/hypopnea was defined as apnea/hypopnea in the absence of oronasal air flow or thoraco-abdominal effort [16, 17]. The apnea/hypopnea index (AHI) was defined as the number of episodes of apnea/hypopnea per hour. The diagnosis of OSA in all the cases was made according to the established criteria (AHI ≥5) [16, 17]. The following patients were excluded from the study: subjects with central sleep apnea/hypopnea and subjects who required steroids or medications other than those for atherosclerotic risk factors, such as hypertension, dyslipidemia and diabetes mellitus {i.e., coronary heart disease, stroke, heart failure, renal insufficiency (serum creatinine > 2.0 mg/dl), bronchial asthma, collagen diseases, etc}. Out of the 53 patients admitted for the evaluation, none had central sleep apnea/hypopnea, and three who had a history of medical treatment for coronary heart disease were excluded. Finally, 50 male subjects were enrolled in this study (51 ± 13 years old; range, 27 to 80 years old). The study protocol was approved by the Ethics Committee of the Tokyo Medical University, and the study was performed in accordance with the guidelines of the latest version of the Declaration of Helsinki. The study participants were divided into three groups according to the severity of OSA, as follows: mild OSA: 5 ≤ AHI < 15, n = 10; moderate OSA: 15 ≤ AHI < 30, n = 12; severe OSA: AHI ≥ 30, n = 28. Among these participants, 29 consecutive male subjects who were diagnosed to have moderate to severe OSA (which is considered as an indication for CPAP therapy; AHI ≥ 15) were followed up at the Tokyo Medical University Hospital [16, 17, 18]. After 3 months of CPAP therapy, fasting blood and urine samples were collected again from the patients for examination of the same parameters. During this 3-month treatment period, no changes were made in the prescribed medications.
As control subjects, 15 age-matched male subjects with hypertension, who showed good control of the blood pressure (blood pressure < 140/90 mmHg) with antihypertensive medication for at least 6 months were enrolled. Two of these subjects were on statins for hypercholesterolemia and none were receiving treatment for diabetes, including oral hypoglycemic agents or insulin. All of these subjects who showed no evidence of a sleep disorder on a portable sleep monitor were enrolled.
Nocturnal sleep studies
All the subjects underwent polysomnography (Alice 4; RESPIRONICS, Murrysville, PA, USA) at a hospital sleep laboratory, which has been described in detail elsewhere [16–18]. Ventilatory flow at the nose and mouth was measured with a thermistor, and chest and abdominal movements were also recorded. The arterial oxygen saturation was measured transcutaneously at the fingertip by pulse oximetry. Apnea was defined as a continuous cessation of airflow for ≥10 seconds, and hypopnea as a ≥50% reduction in the airflow for more than 10 seconds with an oxygen desaturation of ≥3%. OSA was defined as the apnea/hypopnea in the presence of thoraco-abdominal effort, and central apnea/hypopnea was defined as apnea/hypopnea in the absence of oronasal air flow or thoraco-abdominal effort [16, 17]. AHI was calculated as the total number of episodes of apnea and hypopnea per hour of sleep. The lowest oxygen saturation during the estimated sleep time as determined by pulse oximetry (LoSO2) was used as an index of nocturnal hypoxia [19].
Laboratory measurements
Routine blood examinations were performed by enzymatic methods adapted to an autoanalyzer (Hitachi 7470; Hitachi, Tokyo, Japan). The plasma concentrations of IL-1β_(Quantikine, R and D System, Minneapolis, USA), IL-6 (Bender Med Systems Diagnostics, Vienna, Austria), TNF-α (Quantikine, R and D System, Minneapolis, USA), 3-nitrotyrosine (Cayman Chemical, Ann Arbor, USA); a marker of oxidative stress [20], osteocalcin (OC)(BGP IRMA, Mitsubishi, Tokyo, Japan), osteoprotegerin (OPG)(Immundiagnostik AG, Bensheim, Germany), and soluble receptor activator of nuclear factor-кB ligand (sRANKL)(Immundiagnostik AG, Bensheim, Germany), and the urinary concentrations of cross-linked C-terminal telopeptide of type I collagen (CTX)(Nordic Bioscience, Copenhagen, Denmark) were measured by solid-phase sandwich enzyme-linked immunosorbent assay using commercially available kits. The urinary excretion of CTX was adjusted for the urinary concentration of creatinine. Bone-specific alkaline phosphatase (BAP) was determined by enzyme immunoassay (QUIDEL, San Francisco, USA). The inter-assay coefficients variation were as follows; IL-1β = 10.1%, Il-6 = 3.2%, TNF-α = 8.0%, nitrotyrosine = 12.3%, OC = 5.5%, OPG = 9.9%, sRANKL = 11.1%, CTX = 9.3%, and BAP = 6.2%.
Statistical analysis
All the data, including those presented in the figures, are expressed as the mean ± SD. Correlations between the severity of OSA and the parameters of bone metabolism, inflammation and oxidative stress were assessed by both univariate linear regression analysis and multivariate linear regression analyses. The differences in each variable among the four study groups (i.e., three groups classified the severity of OSA and the control group) were evaluated using ANOVA for continuous variables and the chi-square test for categorical variables. The differences in the urinary excretion of CTX and plasma levels of OC and BAP were compared among the four study groups by a general linear model (GLM) multivariate analysis with control for age, gender, body mass index (BMI), systolic and diastolic blood pressure (SBP and DBP), serum total cholesterol (TC), serum triglycerides (TG), serum high-density lipoprotein cholesterol (HDL-C), fasting plasma glucose (FPG), and categorical variables (smoking status and medication status for hypertension, diabetes mellitus and/or dyslipidemia). The significances of the differences in the variables measured between the start of the study and after 3 months’ CPAP therapy were determined by a paired t-test. The relationships between the parameters of bone metabolism and the plasma levels of cytokines and 3-nitrotyrosine in all the participants were assessed by linear regression analysis. The differences in the values of the variables measured between the start of the study and after 3 months’ CPAP therapy were calculated as the delta changes: values obtained after 3 months’ CPAP therapy minus those obtained at the start of the study. The significance of the relationships among the delta changes in the variables was also assessed by linear regression analysis and multivariate linear regression analysis. P values of less than 0.05 were considered to denote statistically significant differences. The statistical analyses were performed using the SPSS software package (SPSS Inc., Chicago, IL).
Results
Baseline clinical characteristics
Table 1 shows the baseline clinical characteristics of the control subjects and the three groups of subjects categorized according to the AHI. Severe OSA was associated with higher values of BMI, blood pressure and TG.
Evidence of inflammation in OSA
We measured the parameters of inflammation and oxidative stress to verify the known consequences of OSA (Table 1). Consistent with previous reports, we found significantly increased plasma levels of IL-6 and TNF-α in the subject group with severe OSA as compared with those in the other three groups. Interestingly, the circulating levels of sRANKL also showed a severity-dependent decrease in the OSA patients, while no differences were observed in the plasma levels of OPG (Table 1).
Enhanced bone resorption in OSA
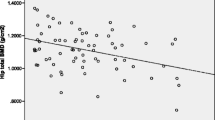
The univariate linear regression analysis revealed that AHI was significantly positively correlated with the creatinine-adjusted urinary excretion of CTX (r = 0.32, p < 0.05), but not with LoSO2 (r = -0.13, p = 0.37), suggesting an association between OSA and increased bone resorption (Fig. 1). While the AHI showed a positive correlation with the plasma levels of IL-6 (r = 0.29, p < 0.05) and TNF-α (r = 0.53, p < 0.01), and a negative correlation with the plasma levels of sRANKL (r = -0.42, p < 0.01), no significant correlations between the AHI and the plasma levels of OC, BAP, IL-1β,_3-nitrotyrosine or OPG were observed. The results of multivariate linear regression analysis indicated a significant association between the AHI and the urinary excretion of CTX (R-square = 0.52, beta = 0.27, t-value = 2.01, p < 0.05), independent of the age, BMI, SBP, DBP, TC, TG, HDL-C, FPG or the categorical variables examined, including the smoking status and medication status for hypertension, diabetes mellitus and/or dyslipidemia. Similarly, the results of the GLM multivariate analysis revealed that the creatinine-adjusted urinary CTX remained significantly higher in the group with severe OSA than in the other 3 groups, even after adjustment for all of the aforementioned variables (Fig. 2).
Baseline levels of the bone metabolic markers in the groups with control or with mild, moderate and severe obstructive sleep apnea. Abbreviations: cont: control subjects; mildOSA: mild obstructive sleep apnea; modeOSA: moderate obstructive sleep apnea; seveOSA: severe obstructive sleep apnea; CTX = creatinine-adjusted urinary excretion of cross-linked C-terminal telopepide of type I collagen; OC: osteocalcin; BAP: bone-specific alkaline phosphatase; *: p < 0.05 vs. control; †: p < 0.05 vs. patients with mild OSA, ‡: p < 0.05 vs. patients with moderate OSA
CPAP therapy decreased the serum levels of inflammatory cytokines and oxidative stress, with suppression of bone resorption
Twenty-nine out of the 40 patients with moderate to severe OSA received continuous positive airway pressure (CPAP) therapy, and were followed up for at least 3 months. Among the three bone metabolic markers tested, only the creatinine-adjusted urinary CTX level showed a significant decrease after 3 months’ CPAP therapy (Fig. 3), consistent with the results of the initial cross-sectional analysis described above. Significant decrease in the plasma levels of IL-1β, IL-6 and TNF-α, and increase in the plasma levels of OPG were also observed in the subjects with moderate to severe OSA after 3 months’ CPAP therapy, in the absence of any change of the body weight of the patients (from 78 ± 16 to 78 ± 15 kg) (Fig. 4).
Bone metabolic markers at the start of the study and after 3 months’ continuous positive airway pressure therapy. Abbreviations: The data are expressed as mean+/-SD; Start = before the start of continuous positive airway pressure therapy; 3 month = at the end of 3 months’ continuous positive airway pressure therapy; CTX: creatinine-adjusted urinary excretion of cross-linked C-terminal telopeptide of type I collagen; OC: osteocalcin; BAP: bone-specific alkaline phosphatase; † = p < 0.01 vs. before the start of continuous positive airway pressure therapy
Parameters of inflammation and oxidative stress at the start of the study and after 3 months’ continuous positive airway pressure therapy. Abbreviations: The data are expressed as mean+/-SD; Start = before the start of continuous positive airway pressure therapy; 3 month = at the end of 3 months’ continuous positive airway pressure therapy; IL-1β: interleukin-1 beta; IL-6: interleukin-6; TNFα = tumor necrosis factor α; OPG: osteoprotegerin; sRANKL: soluble receptor activator of nuclear factor-κB ligand; * = p < 0.05 vs. before the start of continuous positive airway pressure therapy; † = p < 0.01 vs. before the start of continuous positive airway pressure therapy
Relationship between the metabolic bone markers and cytokines
We then searched for a possible etiological link between the various parameters measured and the bone metabolism. At the baseline, a univariate linear regression analysis across the bone metabolic markers and the cytokine levels in all the study participants indicated virtually no association, except for significant negative correlations between plasma levels of IL-1β and OC and a significant positive correlation between the plasma levels of OPG and BAP and plasma levels of TNF-α and BAP (Table 2). The results of the multivariate linear regression analysis demonstrated that the plasma levels of TNF-α showed no significant association with the creatinine-adjusted urinary excretion of CTX after adjustment for age, gender and the presence of atherosclerotic risk factors (i.e., smoking, hypertension, hypercholesterolemia and diabetes mellitus). In addition, none of the delta changes of LoSO2 or the plasma levels of IL-1β, IL-6, TNF-α, nitrotyrosine, sRANKL and OPG measured after 3 months’ CPAP therapy showed any significant correlation with the CPAP-associated decrease in the creatinine-adjusted urinary CTX excretion. Therefore, although OSA was associated with increases in both the urinary CTX level and serum levels of inflammatory cytokines, and CPAP treatment reversed these abnormalities, the changes in the plasma levels of inflammatory cytokines and markers of oxidative stress did not account for the changes in the urinary CTX excretion.
Discussion
In the present study, we demonstrated that the AHI, an indicator of the severity of OSA, was significantly positively associated with the urinary excretion of CTX, independent of the age, BMI or the presence of atherosclerotic risk factors. We showed further that the urinary CTX excretion decreased towards normal after 3 months’ CPAP therapy in the subjects with moderate to severe OSA. There are at least three mechanisms that may potentially mediate abnormal bone metabolism in OSA: hypoxia, increased oxidative stress and inflammation.
Hypoxia, a major pathophysoiological change associated with OSA [1–3], can directly affect bone cell function [12, 21], and hypoxia-related diseases, such as anemia and chronic respiratory disorders are frequently associated with osteopenia [11, 22]. Moreover, in patients with severe emphysema [11, 23], improvement of the pulmonary function by lung volume reduction surgery has been shown to result in improved bone metabolism [24]. Thus, hypoxia associated with chronic respiratory dysfunction can cause reversible abnormalities of bone metabolism. The reports that hypoxia induces osteoclast differentiation [12] and suppresses the functions of osteoblasts [21] are consistent with our current observation of elevation of only a bone resorption marker (urinary CTX), but not of bone formation markers (BAP and OC) [25–27] in our OSA patients. These results may suggest that the abnormal bone metabolism in OSA is characterized by “an uncoupled state” between increased bone resorption and relatively suppressed bone formation.
OSA is, however, quite different from chronic hypoxia-related diseases, such as emphysema, in that the hypoxia is intermittent and that the frequent episodes of hypoxia followed by reoxygenation cause oxidative stress and inflammation [28], both of which have been etiologically implicated in the increased risk of cardiovascular diseases in patients with OSA. The importance of the intermittent nature of hypoxia in OSA is probably reflected by the fact that the urinary CTX levels were weakly, but significantly, correlated with the AHI rather than the LoSO2. While elevation of the plasma levels of inflammatory cytokines is also noted in obese subjects [29], we were able to successfully demonstrate that the parameters of inflammation increased in our OSA patients in a severity-dependent manner in our OSA patients and that CPAP therapy attenuated these abnormalities, in the absence of any significant change of the body weight of the patients. However, the urinary CTX levels showed no significant correlations with the plasma levels of any of the inflammatory cytokines or of a marker of oxidative stress after adjustment for other variables, either at the baseline or after 3 months’ CPAP therapy. There were also no significant correlations among the delta changes in the urinary CTX levels and those of any of the above parameters. Therefore, it seems likely that OSA affects bone metabolism via multiple mechanisms in a manner that varies among individuals and that may be partially but not strongly dependent on the associated inflammation or oxidative stress. Alternatively, abnormal bone metabolism in OSA could be caused by entirely different and as yet unknown mechanisms.
A plausible mechanism to explain the aforementioned “uncoupled state” between bone formation and bone resorption is the influence of cortisol. Elevation of the plasma level of cortisol in OSA patients and its return to normal range after CPAP therapy have been reported [30]. Excessive cortisol levels may suppress bone formation, but not resorption [31]. The next logical step would, therefore, be to clarify the relationship among OSA, bone metabolism and the serum levels of cortisol.
The (RANK)/RANKL/OPG system is crucially involved in the regulation of osteoclast formation and function, and thereby, of bone resorption [14, 15, 32, 33]. Inflammatory cytokines, including IL-1β, IL-6 and TNF-α, are known regulators of the RANK/RANKL/OPG system [14, 22], and induce osteoclast differentiation and/or activation [14, 15, 32, 34]. In the present study, a significant negative correlation was observed between the plasma levels of sRANKL and the AHI. However, CPAP therapy had no effect on the plasma levels of sRANKL, and the plasma levels of OPG indeed increased after CPAP therapy. These inconsistent observations may be attributed to the fact that circulating OPG and sRANKL in the plasma originate mostly from non-skeletal sources and that their plasma levels do not directly reflect their activities in the bone microenvironment [35]. Thus, although our results imply that RANKL may somehow be involved in the abnormal bone metabolism in OSA patients, further studies are needed to clarify and establish the role of the RANK/RANKL/OPG system in OSA-induced bone resorption.
There were three major limitations of this study. First, there were no controls for CPAP therapy, i.e., there was no inclusion of a group of subjects with moderate to severe OSA not undergoing CPAP therapy. In addition, this study also did not include any BMI-matched control subjects.
Secondly, bone mineral density was not assessed in the current study. The clinical significance of our finding of increase in the levels of bone resorption markers in OSA patients cannot be established until the bone mineral density and, ultimately, the fracture risk, is also evaluated. Thus, confirmatory evidence that OSA is indeed an independent risk factor for osteoporosis must await further clinical studies.
Thirdly, we measured the plasma levels of IL-1β, IL-6 and TNF-α only twice (i.e., before and after CPAP therapy), and the time-course of their variations were not examined. Although omission of the assessment of such variations was one of our study limitations, some studies have already reported elevation of the plasma levels of inflammatory cytokines in subjects with OSA and their return to the normal range after CPAP therapy [36, 37].
Because we were not able to find strong determinants of increased bone resorption in the current study, there are still other factors potentially involved in both OSA and bone metabolic abnormalities, including cortisol excess [38] and reduced physical activity that need to be addressed [39]. Future studies focusing on such factors may be helpful for elucidating the pathophysiological link between OSA and osteoporosis.
In conclusion, the present study was the first to demonstrate abnormalities in the markers of bone metabolism in patients with severe OSA, and reversal of these abnormalities following 3 months’ CPAP therapy. Reduced inflammation and oxidative stress along with improvement in the arterial oxygen saturation associated with CPAP therapy may contribute, at least in part, to the observed beneficial effects. Larger-scale clinical studies with bone mineral density and/or fracture incidence as endpoints will be needed to clarify whether or not OSA is indeed an independent risk factor for osteoporosis and whether CPAP therapy might truly have beneficial effects on the bone mass and quality and prevent fractures in subjects with OSA.
References
Collop NA (2005) Obstructive sleep apnea syndromes. Semin Respir Crit Care Med 26:13–24
Caples SM, Gami AS, Somers VK (2005) Obstructive sleep apnea. Ann Intern Med 142:187–97
Shamsuzzaman AS, Gersh BJ, Somers VK (2003) Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA 290:1906–1914
Hatipoglu U, Rubinstein I (2003) Inflammation and obstructive sleep apnea syndrome pathogenesis: a working hypothesis. Respiration 70:665–671
Schulz R, Mahmoudi S, Hattar K et al (2000) Enhanced release of superoxide from polymorphonuclear neutrophils in obstructive sleep apnea. Impact of continuous positive airway pressure therapy. Am J Respir Crit Care Med 162:566–570
Becker HF, Jerrentrup A, Ploch T et al (2003) Effect of nasal continuous positive airway pressure treatment on blood pressure in patients with obstructive sleep apnea. Circulation 107:68–73
Pepperell JC, Ramdassingh-Dow S, Crosthwaite N et al (2002) Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnea: a randomised parallel trial. Lancet 359:204–210
Marin JM, Carrizo SJ, Vicente E et al (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnea-hypopnea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Doherty LS, Kiely JL, Swan V et al (2005) Long-term effects of nasal continuous positive airway pressure therapy on cardiovascular outcomes in sleep apnea syndrome. Chest 127:2076–2084
Young T, Palta M, Dempsey J et al (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Papaioannou A, Parkinson W, Ferko N et al (2003) Prevalence of vertebral fractures among patients with chronic obstructive pulmonary disease in Canada. Osteoporos Int 14:913–917
Arnett TR, Gibbons DC, Utting JC et al (2003) Hypoxia is a major stimulator of osteoclast formation and bone resorption. J Cell Physiol 196:2–8
Basu S, Michaelsson K, Olofsson H et al (2001) Association between oxidative stress and bone mineral density. Biochem Biophys Res Commun 288:275–279
Clowes JA, Riggs BL, Khosla S (2005) The role of the immune system in the pathophysiology of osteoporosis. Immunol Rev 208:207–227
Raisz LG (2005) Pathogenesis of osteoporosis: concepts, conflicts, and prospects. J Clin Invest 115:3318–3325
Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22:667–689
Shiina K, Tomiyama H, Takata Y et al (2006) Concurrent presence of metabolic syndrome in obstructive sleep apnea syndrome exacerbates the cardiovascular risk: a sleep clinic cohort study. Hypertens Res 29:433–441
Rechtshaffen AK, A (ed) 1968 A Manual of Standardized Terminology: Techniques and Scoring System for Sleep Stages of Human Subjects. UCLA Brain Information Service/Brain Research Institute, Los Angeles
Chaudhary B, Dasti S, Park Y et al (1998) Hour-to-hour variability of oxygen saturation in sleep apnea. Chest 113:719–722
Sun YC, Chang PY, Tsao KC et al (2007) Establishment of a sandwich ELISA using commercial antibody for plasma or serum 3-nitrotyrosine (3NT). Elevation in inflammatory diseases and complementary between 3NT and myeloperoxidase. Clin Chim Acta 378:175–180
Utting JC, Robins SP, Brandao-Burch A et al (2006) Hypoxia inhibits the growth, differentiation and bone-forming capacity of rat osteoblasts. Exp Cell Res 312:1693–1702
Miller RG, Segal JB, Ashar BH et al (2006) High prevalence and correlates of low bone mineral density in young adults with sickle cell disease. Am J Hematol 81:236–241
Ionescu AA, Schoon E (2003) Osteoporosis in chronic obstructive pulmonary disease. Eur Respir J Suppl 46:64s–75s
Mineo TC, Ambrogi V, Mineo D et al (2005) Bone mineral density improvement after lung volume reduction surgery for severe emphysema. Chest 127:1960–1966
Bonnick SL, Shulman L (2006) Monitoring osteoporosis therapy: bone mineral density, bone turnover markers, or both. Am J Med 119:S25–31
Szulc P, Seeman E, Delmas PD (2000) Biochemical measurements of bone turnover in children and adolescents. Osteoporos Int 11:281–294
Ueda M, Inaba M, Okuno S et al (2005) Serum BAP as the clinically useful marker for predicting BMD reduction in diabetic hemodialysis patients with low PTH. Life Sci 77:1130–1139
Ryan S, Taylor CT, McNicholas WT (2005) Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation 112:2660–2667
Alam I, Lewis K, Stephens JW, Baxter JN (2007) Obesity, metabolic syndrome and sleep apnea: all pro-inflammatory states. Obes Rev 8:119–127
Vgontzas AN, Pejovic S, Zoumakis E et al (2007) Hypothalamic-pituitary-adrenal axis activity in obese men with and without sleep apnea: effects of continuous positive airway pressure therapy. J Clin Endocrinol Metab 92:4199–4207
Manelli F, Giustina A (2000) Glucocorticoid-induced osteoporosis. Trends Endocrinol Metab. 11:79–85
Tanaka S, Nakamura K, Takahasi N et al (2005) Role of RANKL in physiological and pathological bone resorption and therapeutics targeting the RANKL-RANK signaling system. Immunol Rev 208:30–49
Sambrook P, Cooper C (2006) Osteoporosis. Lancet 367:2010–2018
Boyle WJ, Simonet WS, Lacey DL (2003) Osteoclast differentiation and activation. Nature 423:337–342
Rogers A, Eastell R (2005) Circulating osteoprotegerin and receptor activator for nuclear factor kappaB ligand: clinical utility in metabolic bone disease assessment. J Clin Endocrinol Metab 90:6323–6331
Bravo Mde L, Serpero LD, Barcelo A, Barbe F, Agusti A, Gozal D (2007) Inflammatory proteins in patients with obstructive sleep apnea with and without daytime sleepiness. Sleep Breath 11:177–185
Yokoe T, Minoguchi K, Matsuo H et al (2003) Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation 107:1129–1134
Tomlinson JW, Bujalska I, Stewart PM, Cooper MS (2000) The role of 11 beta-hydroxysteroid dehydrogenase in central obesity and osteoporosis. Endocr Res 26:711–722
Fulkerson JA, Himes JH, French SA et al (2004) Bone outcomes and technical measurement issues of bone health among children and adolescents: considerations for nutrition and physical activity intervention trials. Osteoporos Int 15:929–941
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tomiyama, H., Okazaki, R., Inoue, D. et al. Link between obstructive sleep apnea and increased bone resorption in men. Osteoporos Int 19, 1185–1192 (2008). https://doi.org/10.1007/s00198-007-0556-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-007-0556-0