Abstract
Introduction
Hip fracture is a major public health problem, annually affecting over 350,000 persons in the United States and 1.6 million worldwide. Consequences include decreased survival, loss of independence, and increased risk of subsequent fractures. A substantial decline in bone mineral density (BMD) also occurs, yet the magnitude of the decline specifically attributable to hip fracture has not been documented.
Methods
To determine the amount of BMD decline attributable to hip fracture, the rate of decline in BMD in a cohort of hip fracture patients was compared with that in a cohort of women of similar age and BMD but without hip fracture. All subjects were community dwelling when enrolled. Hip fracture patients in the Baltimore Hip Studies (BHS) came from two hospitals in Baltimore, Maryland, from 1992 through 1995; comparison subjects came from the Study of Osteoporotic Fracture (SOF) enrolled in four areas of the United States during the same period. Eighty-four white, female hip fracture patients 65 years and older from the BHS were compared with 168 SOF participants matched on age, race, and BMD at baseline. BMD of the femoral neck and total hip was measured by dual-energy x-ray absorptiometry.
Results
Hip fracture patients had a greater decline in BMD during the 12-month postfracture follow-up than that expected on the basis of the nonfracture cohort: 4.9% vs. 0.4% at the femoral neck and 3.5% vs. 0.7% for the total hip. The decline in BMD in hip fracture patients was 11.8 times the amount expected at the femoral neck (matched on age and baseline BMD and adjusted for between-cohort differences in smoking prevalence) and 4.9 times that expected for the total hip at the end of 1 year after the hip fracture.
Conclusion
In this sample of older women, bone loss over the year following hip fracture far exceeded that expected and is an important clinical management concern.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture annually affects over 350,000 persons age 65 and older in the United States and over 1.6 million worldwide [1, 2]. Consequences of hip fracture include increased risk of mortality, loss of independent function, and other adverse health and economic consequences for patients, families, and the health care system [3–12]. Annual direct medical costs of hip fracture in the United States alone are estimated at $10.75 billion [13]. Given the global demographic changes projected by 2050, over 650,000 hip fractures will occur annually in the United States, and more than 6 million are anticipated worldwide [1, 2, 14].
Low bone mineral density (BMD) is common in older persons and is a risk factor for hip fracture [6]; BMD at the hip decreases approximately 0.51% per year, on average, among elderly women who have not fractured a hip [15–20]. In contrast, decline in BMD has been reported to be nonlinear and to range from 4% to 7% in the year following hip fracture [21–23]. This decline in BMD may explain, in part, the fact that hip fracture patients are at higher risk of subsequent fractures [24–26]. To date, however, no studies have directly compared the decline in BMD after hip fracture to that in persons without fracture but who have similar age and BMD, thereby limiting our ability to estimate how much of the decline in BMD can be attributed to the fracture itself.
The current study extends our prior work and directly compares the change in hip BMD during the year following hip fracture in a group of women age 65 and older to the change in BMD seen in similarly aged women with similar BMD at baseline but who had not fractured a hip, in order to distinguish the effects of fracture from those of aging. We also comment on the implications these results have for treatment in this vulnerable population.
Materials and methods
Subjects
Hip fracture patients admitted to one of two community hospitals in Baltimore, Maryland, from 1992 through 1995 as part of the Baltimore Hip Studies (BHS) [23], were female, 65 years and older, white, and community dwelling. Patients with pathological or distal femur fractures and those admitted more than 48 h after fracture were excluded. Of 407 eligible patients, 205 (50%) had baseline measurement of BMD at the contralateral hip by dual-energy x-ray absorptiometry (DXA) within 10 days of hospital admission. Informed consent was obtained for all participating patients. The protocol was approved by the institutional review boards of the University of Maryland Baltimore and the participating study hospitals.
The comparison group was drawn from the Study of Osteoporotic Fractures (SOF). During the baseline examination in 1986–1988, a total of 9,704 community-dwelling women age 65 and older were recruited from population-based listings in four areas of the United States: Baltimore, Maryland; Minneapolis, Minnesota; the Monongahela Valley near Pittsburgh, Pennsylvania; and Portland, Oregon [27]. Women who were nonwhite, had previous bilateral hip replacements, or were unable to walk without assistance were excluded [28]. All subjects provided informed consent; protocols were approved by the institutional review boards at each clinic site. For this analysis, the comparison sample was selected from among 6,279 participants with technically adequate hip BMD measurements made by DXA at SOF follow-up visits numbers two (1988–1989) and four (1993–1994; mean follow-up between visits was 42.3 months) who had not suffered a hip fracture between visits two and four.
Measures
In hip fracture patients, BMD was measured using DXA (QDR-1000 W or QDR-1500, Hologic, Waltham, MA, USA) in the contralateral (unaffected) hip within 10 days of hospitalization and again at 2, 6, and 12 months postfracture. The coefficient of variation for these measurements ranged from 0.30% to 0.35%. The precision of the measurements (percent coefficient of variation based on a sample of healthy subjects) was 2.2% for the femoral neck. Age, weight, and comorbid conditions (such as diabetes, Parkinson’s disease, stroke, and heart disease) were abstracted from medical charts by trained research nurses during the hospitalization for the fracture. Current smoking, estrogen and thyroid medication use, and the ability to perform activities of daily living (ADL) during the week before fracture were derived from interviews with the patient or her proxy by trained interviewers. ADL tasks included getting into/out of a car, bed transfer, dressing, and washing. Patients reporting difficulty or inability to perform an ADL task were considered disabled on that task.
Hip BMD was measured in SOF participants using DXA (Hologic QDR 1000, Hologic, Waltham, MA, USA) at SOF follow-up visits two and four, which were on average 42.3 months apart. The mean coefficient of variation between centers was 1.2% for the proximal femur [29]. Both self-administered and interviewer-administered questionnaires were used to assess age, smoking status, use of estrogen and thyroid medications, and the same ADL tasks and comorbidities as in the hip fracture sample; these measures have been described previously [27, 28].
Matching
Of 205 hip fracture patients who had BMD measured at baseline, 179 provided valid, interpretable DXA scans from which hip total BMD could be derived. Of these, one patient had hip total BMD >0.82 g/cm2 and was excluded from this analysis. Of the remaining patients, 88 provided a 12-month follow-up DXA scan. Two SOF participants were matched to each remaining hip fracture patient on age (within 5-year age categories) and baseline total hip BMD (within BMD quartiles based on the hip fracture sample) following an algorithm used previously in the BHS [30]. No SOF respondents could be matched to four hip fracture patients who were either older than age 93 or had a baseline total hip BMD <0.300 g/cm2; these four patients were therefore excluded from analyses. A 2:1 match was successfully achieved for the remaining 84 hip fracture patients, resulting in 168 SOF comparison subjects. It should be noted that the matching algorithm used was a frequency match and did not provide matched sets of two controls and one case. For this reason, no provision was made for the matching in the analytical models described below.
Statistics
The follow-up time points for the hip fracture cohort were 2, 6, and 12 months postfracture, whereas SOF follow-up data were collected after approximately 3.5 years (range 34–52 months). These differences in follow-up periods precluded direct time-specific comparisons of BMD between the hip fracture and SOF cohorts. Therefore, the SOF cohort was used to estimate the expected BMD level for the hip fracture cohort at 2, 6, and 12 months postfracture, assuming a linear rate of decline in BMD over time [16]. The difference in BMD between the observed level for the hip fracture cohort and the expected level was regarded as the excess loss attributable to hip fracture and was estimated by a longitudinal analysis involving both cohorts. The time-specific excess losses are presented in units of g/cm2 and in percentage points (obtained by dividing the excess loss by the SOF baseline mean and multiplying by 100).
A mixed model was fitted using maximum likelihood using PROC MIXED in PC-SAS. Random effects were accounted for by specifying an exchangeable covariance matrix. Fixed effects were modeled according to the following:
where Yt is subject BMD at a specific time; b0 is the intercept (representing the predicted BMD for the SOF cohort at baseline); X is the cohort indicator variable (0=SOF cohort, 1=hip fracture cohort); t2, t6, t12, and t>12 are indicator variables for the time corresponding to follow-up at 2, 6, 12, and more than 12 months, respectively; and m is months of follow-up for SOF subjects.
Because of product terms involved, b1, b2, b3, and b4 are fitted with hip fracture data, and b5, the linear rate of change, with SOF data. After parameter estimates were obtained, the excess loss at 2 months was determined as b2-2 b5, that at 6 months as b3-6 b5, and that at 12 months as b4-12 b5.
Each potential confounder was assessed individually as a covariate in the fixed effect model. The model was then refitted to obtain excess losses adjusted for that variable. Variables were deemed confounders when one or more adjusted effects (for 2, 6, and 12 months) differed by 10% or more from the corresponding unadjusted effects. A final model was fitted with the inclusion of all identified confounders to determine the adjusted time-specific effects.
Results
Characteristics of hip fracture patients and SOF participants are shown in Table 1. The groups had, by virtue of matching, similar age, total hip BMD [0.595 g/cm2 (±0.102) for fracture patients and 0.610 g/cm2 (±0.095) for SOF participants] and femoral neck BMD [0.548 g/cm2 (±0.084) for fracture patients and 0.536 g/cm2 (±0.083) for SOF participants] at baseline. Hip fracture patients reported more disability in each ADL task and a higher prevalence of diabetes, stroke, and heart problems.
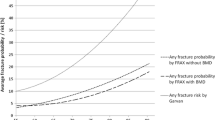
Hip fracture patients had a greater decline in BMD during the 12-month follow-up than expected in both bone regions: 3.5% vs. 0.7% at the total hip and 4.9% vs. 0.4% at the femoral neck. These results are shown graphically in Fig. 1. Each variable in Table 1 was evaluated as a potential confounder of the association between hip fracture and BMD change; only smoking at the time of fracture met criteria for a confounder. The difference between observed and expected decline in BMD, adjusted for smoking (Table 2), showed the excess losses for total hip BMD to be 1.5 percentage points at 2 months, 2.2 percentage points at 6 months, and 2.8 percentage points at 12 months. Even greater differences were seen for femoral neck BMD: excess loss of 2.7, 3.0, and 4.6 percentage points at 2, 6, and 12 months postfracture, respectively.
Expected and observed change in total hip bone mineral density (panel A) and femoral neck bone mineral density (panel B) during the 12 months following fracture. Legend for both panels: • with solid line, hip fracture (observed mean and standard error); broken line, Study of Osteoporotic Fractures (SOF; expected mean based on interpolated data obtained over a 42.3-month period). Observed change based on hip fracture patients; expected change based on SOF
Because the groups had significantly different frequency of ADL disability, additional sensitivity analyses were performed to determine to what degree the reported excess BMD loss was due to greater preexisting functional disability in the hip fracture patients. The 40 hip fracture patients with no prefracture ADL disability were compared with the entire SOF group; results were similar to those reported for the complete hip fracture group (Table 2), suggesting that losses may be more rapid and greater at the femoral neck in this unimpaired group.
Discussion
During the year after a hip fracture, white women age 65 and older suffered an additional decline of 4.6% in BMD at the contralateral femoral neck and an extra 2.8% in BMD at the contralateral total hip compared with the expected decline among women of similar age and baseline BMD who had not fractured. In this study, these excess losses translate into a decline in BMD 11.8 times greater than that anticipated in the contralateral femoral neck and 4.9 times greater than that anticipated in the contralateral total hip a year after a hip fracture. Coupled with the 6% loss in lean body mass in the first 2 months postfracture [23], the effects of hip fracture on the already compromised and aging musculoskeletal system are highly clinically significant.
Earlier work has shown that, compared with same-aged peers, hip fracture patients experience higher rates of mortality [4, 31], mobility limitations [5], and decline in physical functioning [5]. They also experience declines in muscle mass, strength, and neuromuscular performance [3, 5, 21, 23, 32]. Combined with the excess losses in bone mass that follow a hip fracture, it is not surprising that those who have fractured are at increased risk of falling and having another fracture [24–26, 33–37].
To our knowledge, this is the first study of bone change to quantify the magnitude of the excess decline in BMD associated with hip fracture. The mechanisms underlying the loss of bone after hip fracture are still incompletely understood. Weight bearing is important to maintain bone mass, and loss of hip BMD follows loss of weight bearing in other situations [38–40]. Recovery of ambulation attenuates or reverses bone loss [41, 42]. Vitamin D deficiency and secondary hyperparathyroidism are common among hip fracture patients [43, 44] and are likely to contribute to bone loss, as parathyroid hormone levels increase further during the year following fracture [44, 45]. An elevated rate of bone resorption is an independent risk factor for hip fracture [46, 47] but changes relatively little during the year after a hip fracture [44]. In contrast, bone formation increases significantly during the early postfracture period [44], but this activity is likely directed primarily at fracture site repair. Regardless of the exact mechanisms, physiologic reserves in hip fracture patients appear to be inadequate to provide an adaptive skeletal response during the recovery period with typical postfracture care.
It also is notable that when post-hip-fracture changes in BMD are examined in conjunction with changes in physical and neuromuscular function, the changes in BMD are for the most part independent of these other changes [48]. This independence has important implications for care after hip fracture, suggesting that treating bone loss requires strategies that go beyond the usual rehabilitation that emphasizes muscle strengthening, balance, and ADL performance. Thus, in addition to recommending that postfracture care include physical therapy, graded exercise, adoption of fall prevention strategies, and consideration of the use of hip protectors, the National Osteoporosis Foundation treatment guidelines for osteoporosis recommend pharmacologic intervention in addition to calcium and vitamin D supplementation in any patient with a history of either vertebral or hip fracture, regardless of BMD [49, 50].
Despite recommendations, most hip fracture patients do not receive definitive pharmacologic treatment, nor is osteoporosis evaluation generally performed [51–58]. In fact, osteoporosis diagnosis, which increases the likelihood of treatment [52, 59–61], is made in only approximately one-quarter of women who sustain hip fracture, even after the event [52, 54, 58, 61]. General treatment rates under 20% are typical, even as long as 1 year after the fracture [51–58, 62, 63], and calcium and vitamin D supplementation are the most commonly used treatments [51, 63]. Nonetheless, studies do indicate some increases in recent years in pharmacologic treatment after hip fracture [53, 57, 59]. One study reported increases from 6% to 22% from 1995 to 2000 [53]; another reported an increase from 11% to 29% from 1997 to 2000 [57]; and a third, examining change from 1995 to 2000, reported increased use of calcium on hospital discharge from 7% to 17%, as well as increased use of antiresorptive therapy on discharge from 2% to 15% [59].
Thus far, neither orthopedic surgeons nor primary care physicians have made postfracture osteoporosis management a priority. Primary care physicians identify patient age and comorbidities [60, 64], uncertainty about efficacy of drug therapy [65], cost, constraints placed by managed care, and possible adverse reactions to medications as barriers to treating osteoporosis after fragility fracture [66]. In addition, physicians identified inadequacies in their own understanding of osteoporosis as a barrier to treating the postfracture patient [64–66].
This study has several limitations. First, although the characteristics of the overall sample of 205 patients reflect the majority of hip fracture patients (ambulatory white women in urban and suburban communities), results should be generalized with caution. Patients came from only two hospitals in a single metropolitan area, and none were male, nonwhite, or institutionalized at the time of fracture. Second, less than one-half of all patients with a baseline BMD measurement were included in the analysis; these women were slightly younger, had fewer comorbid conditions, had a higher frequency of estrogen and thyroid medication use, and were less likely to be smoking currently than those not included in the analysis (data not shown). Third, this study followed hip fracture patients for only 1 year and assumed a linear rate of decline in BMD over 42 months in the comparison group, based on evidence from prior reports of BMD change [15–20].
The study has several strengths. Results have good internal validity as a consequence of matching to SOF participants on the two particularly important criteria of age and baseline BMD, and there was consideration of a broad spectrum of potential confounding factors. In addition, both cohorts are essentially contemporaneous, so diagnostic and treatment options for osteoporosis are similar. This careful selection of a comparison group has enabled us to extend our understanding of the consequences of hip fracture by demonstrating that although their BMD is very low at the time of fracture, substantial and clinically important further losses of BMD follow during the year after a hip fracture. Furthermore, the magnitude of the observed bone loss in the hip fracture subgroup used in these analyses is very similar to that reported for the whole sample and in two other studies of BMD change after hip fracture [21–23], leaving us reasonably confident that these results are similar to what would be derived from a study of bone loss among a broader population of female hip fracture patients.
Loss of BMD following a hip fracture is clinically significant and is one of the multiple consequences of hip fracture. In a recent position statement from the American Academy of Orthopaedic Surgeons, which was endorsed by 17 professional organizations whose members care for hip fracture patients [67] and was based on several recent descriptions of hip fracture treatment guidelines [68, 69], it is clear that the care of hip fracture patients will require multiple strategies both during and after their acute care stay. The losses in BMD reported here are likely to place these already vulnerable patients at increased risk of subsequent hip and other osteoporotic fractures. Further study of the accelerated loss of BMD observed in this study and its mechanisms are needed. The effectiveness of postfracture osteoporosis treatment also needs further investigation as we develop more complete and validated evidence-based postfracture treatments, management guidelines, and care pathways.
References
Cooper C, Campion G, Melton LJ (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7:407–413
Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M et al (2000) Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 55A:M498–M507
Magaziner J, Lydick E, Hawkes W, Fox KM, Zimmerman SI, Epstein RS et al (1997) Excess mortality attributable to hip fracture in white women aged 70 years and older. Am J Public Health 87:1630–1636
Magaziner J, Fredman L, Hawkes W, Hebel JR, Zimmerman S, Orwig DL et al (2003) Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. Am J Epidemiol 157:1023–1031
Wehren LE, Magaziner J (2003) Hip fracture: risk factors and outcomes. Curr Osteoporos Rep 1:78–85
van Balen R, Steyerberg EW, Polder JJ, Ribbers TLM, Habbema JDF, Cools HJM (2001) Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Ortop 390:232–243
Braithwaite RS, Col NF, Wong JB (2003) Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc 51:364–370
Ray NF, Chan JK, Thamer M, Melton LJ (1997) Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res 12:24–35
Brainsky A, Glick H, Lydick E, Epstein R, Fox KM, Hawkes W et al (1997) The economic cost of hip fractures in community-dwelling older adults: a prospective study. J Am Geriatr Soc 45:281–287
Kashner T, Magaziner J, Pruitt S (1990) Family size and caregiving of aged parents with hip fractures. In: Biegel D, Blum A (eds) Aging and caregiving: theory, research and policy. Sage Publications, Beverly Hills, CA, pp 184–203
Saltz CC, Zimmerman SI, Tompkins C, Harrington D, Magaziner J (1999) Stress among caregivers of hip fracture patients: a longitudinal study. J Gerontol Soc Work 30:167–181
Melton LJ 3rd, Gabriel SE, Crowson CS, Tosteson AN, Johnell O, Kanis JA (2003) Cost-equivalence of different osteoporotic fractures. Osteoporos Int 14(5):383–388
Melton LJI (1993) Hip fractures: a worldwide problem today and tomorrow. Bone 14:S1–S8
Jones G, Nguyen T, Sambrook P, Kelly PJ, Eisman JA (1994) Progressive loss of bone in the femoral neck in elderly people: longitudinal findings from the Dubbo Osteoporosis Epidemiology Study. Br Med J 309:691–695
Ensrud KE, Palermo L, Black DM, Cauley J, Jergas M, Orwoll ES et al (1995) Hip and calcaneal bone loss increase with advancing age: longitudinal results from the Study of Osteoporotic Fractures. J Bone Miner Res 10(11):1778–1787
Burger H, de Laet CEDH, van Daele PLA, Weel AEAM, Witteman JCM, Hofman A et al (1998) Risk factors for increased bone loss in an elderly population: the Rotterdam Study. Am J Epidemiol 147(9):871–879
Dennison E, Eastell R, Fall CHD, Kellingray S, Wood PJ, Cooper C (1999) Determinants of bone loss in elderly men and women: a prospective population-based study. Osteoporos Int 10:384–391
Karlsson MK, Obrant KJ, Nilsson BE, Johnell O (2000) Changes in bone mineral, lean body mass and fat content as measured by dual energy X-ray absorptiometry: a longitudinal study. Calcif Tissue Int 66:97–99
Melton LJ III, Atkinson EJ, O’Connor MK, O’Fallon WM, Riggs BL (2000) Determinants of bone loss from the femoral neck in women of different ages. J Bone Miner Res 15(1):24–31
Karlsson M, Nilsson JA, Sernbo I, Redlund-Johnell I, Johnell O, Obrant KJ (1996) Changes of bone mineral mass and soft tissue composition after hip fracture. Bone 18(1):19–22
Dirschl DR, Henderson RC, Oakley WC (1997) Accelerated bone mineral loss following a hip fracture: a prospective longitudinal study. Bone 21(2):79–82
Fox KM, Magaziner J, Hawkes WG, Yu-Yahiro J, Hebel JR, Zimmerman SI et al (2000) Loss of bone density and lean body mass after hip fracture. Osteoporos Int 11(1):31–35
Colón-Emeric C, Kuchibhatla M, Pieper C, Hawkes W, Fredman L, Magaziner J et al (2003) The contribution of hip fracture to risk of secondary fractures: data from two longitudinal studies. Osteoporos Int 14(11):879–883
Schroder HM, Petersen KK, Erlandsen M (1993) Occurrence and incidence of the second hip fracture. Clin Ortop 289:166–169
Chapurlat RD, Bauer DC, Nevitt M, Stone K, Cummings SR (2003) Incidence and risk factors for a second hip fracture in elderly women. The Study of Osteoporotic Fractures. Osteoporos Int 14(2):130–136
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE et al (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332(12):767–773
Cummings SR, Black DM, Nevitt MC, Browner WS, Cauley JA, Genant HK et al (1990) Appendicular bone density and age predict hip fracture in women. JAMA 263:665–668
Steiger P, Cummings SR, Black DM, Spencer NE, Genant HK (1992) Age-related decrements in bone mineral density in women over 65. J Bone Miner Res 7(6):625–632
Fredman L, Hawkes W, Zimmerman SI, Hebel JR, Magaziner J (2001) Extending gerontological research through linking investigator’s studies to public-use datasets. Gerontologist 41(1):15–22
Wolinsky FD, Fitzgerald JF, Stump TE (1997) The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health 87(3):398–403
Fredman L, Magaziner J, Hawkes W, Hebel JR, Fried LP, Kasper J et al (2005) Female hip fracture patients had poorer performance-based functioning than community-dwelling peers over 2-year follow-up period. J Clin Epidemiol 58(12):1289–1298
Sherrington C, Lord SR (1998) Increased prevalence of fall risk factors in older people following hip fracture. Gerontology 44:340–344
Nevitt MC, Cummings SR, Hudes ES (1991) Risk factors for injurious falls: a prospective study. J Gerontol 46(5):M164–M170
Tromp AM, Smit JH, Deeg DJH, Bouter LM, Lips P (1998) Predictors for falls and fractures in the Longitudinal Aging Study Amsterdam. J Bone Miner Res 13(12):1932–1939
King MB, Tinetti ME (1995) Falls in community-dwelling older persons. J Am Geriatr Soc 43:1146–1154
Dretakis KE, Dretakis EK, Papakitsou EF, Psarakis S, Steriopoulos K (1998) Possible predisposing factors for the second hip fracture. Calcif Tissue Int 62:366–369
Jorgensen L, Jacobsen BK (2001) Changes in muscle mass, fat mass, and bone mineral content in the legs after stroke: a 1 year prospective study. Bone 28:655–659
Uebelhart D, Bernard J, Hartmann DJ, Moro L, Roth M, Uebelhart B et al (2000) Modifications of bone and connective tissue after orthostatic bedrest. Osteoporos Int 11(1):59–67
LeBlanc A, Schneider V, Shackelford L, West S, Oganov V, Bakulin A et al (2000) Bone mineral and lean tissue loss after long duration space flight. J Musculoskel Neuron Interact 1:157–160
LeBlanc AD, Schneider VS, Evans HJ, Engelbretson DA, Krebs JM (1990) Bone mineral loss and recovery after 17 weeks of bed rest. J Bone Miner Res 5:843–850
Jorgensen L, Jacobsen BK, Wisgaard T, Magnus JH (2000) Walking after stroke: does it matter? Changes in bone mineral density within the first 12 months after stroke. A longitudinal study. Osteoporos Int 11:381–387
LeBoff MS, Kohlmeier L, Hurwitz S, Franklin J, Wright J, Glowacki J (1999) Occult vitamin D deficiency in postmenopausal US women with acute hip fracture. JAMA 281(16):1501–1511
Yu-Yahiro JA, Michael RH, Dubin NH, Fox KM, Sachs M, Hawkes W et al (2001) Serum and urine markers of bone metabolism during the year after hip fracture. J Am Geriatr Soc 49:877–883
Dubin NH, Monahan LK, Yu-Yahiro JA, Michael RH, Zimmerman SI, Hawkes W et al (1999) Serum concentrations of steroids, parathyroid hormone, and calcitonin in postmenopausal women during the year after hip fracture: effect of location of fracture and age. J Gerontol: Med Sci 54A(9):M467–M473
Garnero P, Hausherr E, Chapuy M-C, Marcelli C, Grandjean H, Muller C et al (1996) Markers of bone resorption predict hip fracture in elderly women: the EPIDOS prospective study. J Bone Miner Res 11(10):1531–1538
Akesson K, Vergnaud P, Gineyts E, Delmas PD, Obrant KJ (1993) Impairment of bone turnover in elderly women with hip fracture. Calcif Tissue Int 53:162–169
Wehren LE, Hawkes W, Hebel JR, Orwig D, Zimmerman SI, Fox KM et al (2004) Predictors of bone loss after hip fracture. Osteoporos Int 15:125–131
National Osteoporosis Foundation (2003) Physician’s guide to prevention and treatment of osteoporosis. National Osteoporosis Foundation, Washington, DC
National Osteoporosis Foundation (2003) Health professional’s guide to rehabilitation of the patient with osteoporosis. National Osteoporosis Foundation, Washington, DC
Orwig DL, Wehren LE, Yu-Yahiro JA, Hochberg M, Magaziner J (2001) Treatment of osteoporosis following a hip fracture: sending results of bone densitometry to primary care physicians does not increase use of pharmacologic therapy (Abstract F382). J Bone Miner Res 16(Suppl 1):S220
Juby AG, De Geus-Wenceslau CM (2002) Evaluation of osteoporosis treatment in seniors after hip fracture. Osteoporos Int 13:205–210
Solomon DH, Finkelstein JS, Katz JN, Mogun H, Avorn J (2003) Underuse of osteoporosis medications in elderly patients with fractures. Am J Med 115:398–400
Simonelli C, Chen Y-T, Morancey J, Lewis AF, Abbott TAI (2003) Evaluation and management of osteoporosis following hospitalization for low-impact fracture. J Gen Intern Med 18:17–22
Kamel HK, Duthie EH (2002) The underuse of therapy in the secondary prevention of hip fractures. Drugs Aging 19:1–10
Harrington JT, Broy SB, Derosa AM, Licata AA, Shewmon DA (2002) Hip fracture patients are not treated for osteoporosis: a call to action. Arthritis Rheum 47:651–654
Gardner MJ, Flik K, Mooar PA, Lane JM (2002) Improvement in the undertreatment of osteoporosis following hip fracture. J Bone Joint Surg 84-A:1342–1348
Follin S, Black J, McDermott M (2003) Lack of diagnosis and treatment of osteoporosis in men and women after hip fracture. Pharmacotherapy 23:190–198
Bahl S, Coates PS, Greenspan SL (2003) The management of osteoporosis following hip fracture: have we improved our care? Osteoporos Int 14(11):884–888
Jachna CM, Whittle J, Lukert B, Graves L, Bhargava T (2003) Effect of hospitalist consultation on treatment of osteoporosis in hip fracture patients. Osteoporos Int 14(8):665–671
Black JN, Follin SL (2001) Osteoporosis diagnosis and management following hip fracture [abstract]. J Bone Miner Res 16(Suppl 1):S214
Cree MW, Juby AG, Carriere KC (2003) Mortality and morbidity associated with osteoporosis drug treatment following hip fracture. Osteoporos Int 14(9):722–727
Bellantonio S, Fortinsky RH, Prestwood K (2001) How well are community-living women treated for osteoporosis after hip fractures? J Am Geriatr Soc 49:1197–1204
Kaufman JD, Bolander ME, Bunta AD, Edwards BJ, Fitzpatrick LA, Simonelli C (2003) Barriers and solutions to osteoporosis care in patients with a hip fracture. J Bone Joint Surg Am 85-A(9):1837–1843
Taylor JC, Sterkel B, Utley M, Shipley M, Newman S, Horton M et al (2001) Opinions and experiences in general practice on osteoporosis prevention, diagnosis, and management. Osteoporos Int 12:844–848
Simonelli C, Killeen K, Mehle S, Swanson L (2002) Barriers to osteoporosis identification and treatment among primary care physicians and orthopedic surgeons. Mayo Clinic Proc 77:334–338
Morris AH, Zuckerman JD (2002) National Consensus Conference on Improving the Continuum of Care for Patients with Hip Fracture. J Bone Joint Surg Am 84-A(4):670–674
Chilov MN, Cameron ID, March LM (2003) Evidence-based guidelines for fixing broken hips: an update. Med J Aust 179(9):489–493
Freitag MH, Magaziner J (2006) Post-operative considerations in hip fracture management. Curr Rheumatol Rep 8(1):55–62
Acknowledgements
We would like to acknowledge the Baltimore Hip Studies, funded through Public Health Service Grant R37AG09901; the Study of Osteoporotic Fractures, funded through Public Health Service Grants AG05395, AG05407, AR35582, AR35583, and AR35584; and the Claude D. Pepper Older Americans Independence Center, grant P60-AG12583.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Magaziner, J., Wehren, L., Hawkes, W.G. et al. Women with hip fracture have a greater rate of decline in bone mineral density than expected: another significant consequence of a common geriatric problem. Osteoporos Int 17, 971–977 (2006). https://doi.org/10.1007/s00198-006-0092-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0092-3