Abstract
Introduction and hypothesis
Uterine conserving re-suspension surgery has become more popular in recent years. Such surgery may allow preservation of fertility in younger women, but may also have the added benefit of augmenting weak connective tissue and possibly providing stronger apical support than the conventional hysterectomy. Our goal was to evaluate the 1- to 4-year outcome of laparoscopic hysteropexy for the surgical management of uterine prolapse.
Methods
This study was a prospective observational study of 182 consecutive women who underwent laparoscopic hysteropexy, with or without additional vaginal repair, from the beginning of 2007 until the end of 2010. Women were invited to attend a dedicated clinic for interview and their prolapse was assessed using the Patient Global Impression of Improvement (PGI-I), the International Consultation on Incontinence Questionnaire for Vaginal Symptoms (ICIQ-VS) and the pelvic organ prolapse quantification (POP-Q) scale. Wilcoxon signed-rank test was used to compare pre-operative with postoperative data. Complications and women’s satisfaction were also noted.
Results
One hundred and forty women agreed to participate; the mean interval from operation was 2.1 years (range 1–4.4). Eighty-nine percent of women felt that their prolapse is “very much” or “much” better using PGI-I subjective outcome measure. There was significant improvement for all parameters of ICIQ-VS and POP-Q scoring post-surgery (p < 0.001). Six women (4 %) had further apical prolapse; of these, 3 underwent further prolapse surgery. None of the participants had any mesh exposure. Ninety two percent of participants would recommend the operation.
Conclusions
Laparoscopic hysteropexy is a safe and effective treatment. The 1- to 4-year outcome suggests high patient satisfaction and low rates of apical prolapse recurrence. Longer term follow-up and randomized controlled studies are required.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse is very common. The lifetime risk of any pelvic floor surgery by 80 years of age is estimated to be 12 % [1]. The risk of recurrence and repeat surgery is high [1, 2]. There is an 8 times higher risk of repeat prolapse surgery in women who underwent hysterectomy for treatment of prolapse grade 2 or higher compared with controls [3].
Traditionally, vaginal hysterectomy has been the treatment of choice for uterine prolapse. However, hysterectomy does not address the underlying pathophysiology of poor connective tissue support, which may explain the high incidence of recurrence and repeat surgery.
Recently, uterine-conserving re-suspension surgery has become more popular. Several techniques, including vaginal, open abdominal and laparoscopic approaches, have been described with varying success rates [4]. These procedures have the potential to improve symptoms of prolapse, psychological wellbeing, sexual function and, in younger women, possibly fertility. In general, laparoscopic pelvic surgery has the potential benefit of shorter postoperative hospital stay and recovery compared with open procedures [5, 6].
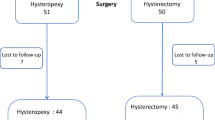
We have previously reported the 10-week outcome of laparoscopic hysteropexy in 51 women [7]. There was one failure, due to cervical elongation. Significant improvement was noted in both the ICIQ-VS questionnaire and POP-Q measurements. We postulate that uterine prolene mesh re-suspension will augment weak connective tissue, provide strong apical support and reduce the risk of recurrent apical prolapse. Since 2006, we have offered this as an alternative to hysterectomy for all women presenting with uterine prolapse who wish to consider surgery and uterine preservation. We now report the longer term outcome for those patients plus additional cases in a larger patient cohort.
Materials and methods
Patient selection
The investigation was designed as an ongoing prospective observational study at a tertiary referral urogynaecology unit in Oxford, UK, over a 4-year period between early January 2007 and the end of December 2010. One hundred and eighty-two consecutive women with symptomatic uterine prolapse, who wished to retain their uterus, underwent laparoscopic hysteropexy. These included women who were previously reported in the shorter term follow-up [7]. The women were invited to attend a dedicated clinic over a period of a year following their operation. Two women who subsequently underwent hysterectomy for non-prolapse-related symptoms were not included in the analysis. Women with previous abnormal cervical cytological examination, abnormal uterine bleeding, significant uterine enlargement (e.g. uterine fibroids) or concomitant medical problems precluding general anaesthesia or the use of a steep Trendelenburg position, were discouraged from having laparoscopic hysteropexy.
All women were informed of the lack of long-term follow-up data with this procedure. Those of childbearing age undergoing hysteropexy were also informed of the lack of data on this procedure with regard to pregnancy and warned that they would require delivery by Caesarean section, if they should subsequently become pregnant. The women who agreed to removal of the uterus were offered a vaginal hysterectomy, instead of hysteropexy.
As this study was part of a surgical audit, approval was obtained from the regional audit committee to measure the outcome of all the women who underwent hysteropexy over the 4-year period.
Prolapse assessment
Prior to surgery, a standardized history and examination were undertaken in the gynaecology clinic. This included questions on the presence or absence of prolapse symptoms (vaginal lump, or dragging sensation or discomfort), urinary symptoms (stress incontinence, urgency, frequency, urge incontinence and voiding dysfunction) and bowel symptoms (constipation, urgency, flatus and faecal incontinence, and difficulties with defecation). A subjective assessment of the prolapse was made using the International Consultation on Incontinence Questionnaire for Vaginal Symptoms (ICIQ-VS) [8]. This is a validated questionnaire measuring vaginal prolapse symptoms and their impact. ICIQ-VS has been shown to effectively measure change in symptoms pre- and post-treatment [8].
Objective assessment of pelvic organ prolapse was performed during a Valsalva manoeuvre, in the left lateral position, using a Sims’ speculum. The pelvic organ prolapse quantification (POP-Q) [9] scale was used to grade the degree of prolapse at all sites. Where indicated, further assessments of pelvic organ (e.g. bladder) function, such as urodynamic studies, were performed.
Surgical technique
Surgery was performed by the senior authors or by the urogynaecology sub-specialty trainee under their direct supervision. With this operation the uterus is suspended from the sacral promontory using a bifurcated polypropylene type-1 monofilament macroporous non-absorbable mesh (ProLiteTM; Atrium Medical Corporation, Hudson, NH, USA), which is transfixed around the cervix. The procedure is fully described and presented in a video article in this issue of the journal [10].
Our surgical technique for laparoscopic hysteropexy evolved during the study period. Initially, we did not completely close the peritoneum over the mesh as previous research suggested that this was unnecessary [11]. However, when performing subsequent laparoscopies on three of our patients, we noted adhesions between the mesh and loops of the small bowel. We therefore amended our technique to include complete peritonisation of the mesh.
Follow-up
Each woman was followed up initially in the clinic for 2–3 months post-surgery. They were then invited to attend a dedicated follow-up clinic, 1–4 years following their initial hysteropexy operation. The second visit was over a 7-month period (one session per week). One researcher performed all the assessments. As the follow-ups were not at a fixed time after the operation and were spread over a 7-month period, the intervals varied from 1 to 4 years post-surgery.
At this clinic women attended with a self-completed validated ICIQ-VS questionnaire and their pelvic organ prolapse was assessed using the POP-Q scale. To reduce the risk of bias, the assessment was performed by one subspecialty trainee who had not performed the operation. Only one individual performed POP-Q; this increased the consistency of measurements.
Operative details and perioperative complication data were obtained from the women and clinical case notes. During the interview further questions were asked regarding any current urinary symptoms and their satisfaction with the operation. Subjective surgical outcome was measured using the Patient Global Impression of Improvement (PGI-I), which is a validated tool as a global index of response to prolapse surgery [12]. The PGI-I is a seven-scale response to women comparing the postoperative condition with the pre-operative state, 1 being very much better and 7 being very much worse [12].
The measure for primary successful subjective outcome was the PGI-I score, as recommended by the IUGA/ICS joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse [13].
The secondary objective outcome measures were the rate of repeat apical surgery and improvement in POP-Q measurement. The secondary measures for successful subjective outcome were significant reductions in the ICIQ-VS questionnaire scores for prolapse symptoms, sexual wellbeing and quality of life.
All method definitions and units conform to the standards jointly recommended by the IUGA and the ICS, except where specifically noted [14, 15].
Statistical analysis
Descriptive statistics were used for the whole population. To compare the difference between the means scores pre- and postoperatively, the Wilcoxon signed-rank test was used. The significance level was set at p < 0.05. Statistical analysis was performed using the Statistical package for the Social Science (SPSS) 16.0 for Windows.
Results
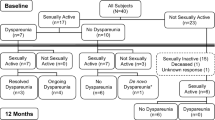
Of the total of 182 women undergoing laparoscopic hysteropexy, 140 women agreed to participate with follow-up. Their demographics are summarized in Table 1. At the time of review 70 % were sexually active and none was actively trying to conceive.
Pre-operatively, all women had a significant symptomatic uterine descent with at least point C below −2 cm using POP-Q scoring. The range of pre-operative point C on POP-Q scoring is summarised in Table 1. In addition, 113 of the women (81 %) had a moderate to severe anterior vaginal wall prolapse, and 127 (90 %) had a posterior vaginal wall prolapse with deficient perineal body. Thirteen of the women (9 %) had a history of previous anterior or posterior vaginal wall repair. As well as undergoing laparoscopic hysteropexy, 91 % of the women underwent at least one additional concomitant procedure (Table 1). Assessment for additional vaginal repair was performed once apical support was achieved with hysteropexy by the surgeon. Although high numbers of patients were noted to have anterior prolapse prior to hysteropexy, the majority did not require repair post-apical support. The mean duration of the hysteropexy operation was 55 min (range 40–75 min), measured from the first incision, and excluding the time required to perform any concomitant procedures. The median duration of the postoperative inpatient stay was 2 nights (range 1–6).
The Patient Global Impression of Improvement (PGI-I) in prolapse was obtained for all 140 women. In this study the prolapse was mostly improved, apart from 2 women who felt there was no change. In 89 % the PGI-I score was “very much” or “much” better. There were no patients reporting worsening of prolapse symptoms (Fig. 1).
Objective changes in POP-Q scoring are shown in Table 2. The Wilcoxon signed-rank test showed that the differences between the postoperative and pre-operative scores for all parameters were statistically significant, with improvement in women postoperatively (p < 0.001; Table 2).
Of the 140 participants, 76 had completed both pre- and postoperative ICIQ-VS questionnaires at the time of interview. Significant subjective improvements in vaginal (prolapse) symptoms, sexual wellbeing and related quality of life were observed (Table 3).
At the time of review women were asked about their incontinence symptoms. Women who had symptoms of stress (n = 63) and urge incontinence (n = 81) pre-operatively and did not undergo concomitant continence surgery, reported subjective improvement or cure of their stress and urge incontinence in 57 % and 54 % of cases respectively. Of the 140 women, 5 (4 %) had new onset of urinary stress incontinence and 9 (6 %) developed urinary urge incontinence. The interval between new symptoms and the operation was not determined in this audit. The urinary question was asked postoperatively at review and not verified with a pre- and postoperative validated questionnaire. Patient satisfaction from the operation was also analysed by asking women if they would recommend the operation to other women; 129 women (92 %) said they would.
Two women had a recurrent symptomatic uterine prolapse at the introitus that was treated successfully with repeat laparoscopy and plication of the mesh with non-absorbable polyester 2–0 sutures (Ethibond ExcelTM; Ethicon, Somerville, NJ, USA). These operations were performed 5 and 11 months following hysteropexy. Another two women had asymptomatic uterine prolapse with point C at 0 cm on POPQ scoring and did not wish further surgical intervention. A further two women were symptomatic owing to a very elongated cervix. Of these one required amputation of the cervix 10 months post-hysteropexy operation, the other did not wish to undergo surgery that might affect future fertility. The 3 women who had repeat apical surgery were subsequently asymptomatic of prolapse. In addition, 10 women (7 %) had persistent anterior vaginal wall prolapse, and subsequently underwent anterior colporrhaphy or laparoscopic paravaginal repair prior to review. The mean time interval from hysteropexy until anterior compartment repair was 1.5 years (range 3 month to 2.5 years). Two women required posterior colpoperineorrhaphy 1.2 and 2 years post-hysteropexy operation. A further 35 (25 %) had anterior prolapse at or beyond the hymenal ring at the time of the review. Of these, 21 women (15 % of the total) were symptomatic.
Of the 182 women in this observational study, 2 women underwent subsequent hysterectomy. One had persistent bowel symptoms post-adhesiolysis (non-reperitonised mesh) and underwent hysterectomy 3 years after the initial hysteropexy. The other woman who had a concomitant myomectomy at the time of the hysteropexy and a persistent menstrual problem underwent hysterectomy 1.5 years post-hysteropexy. They were not included in the analysis. Hysterectomy was performed by laparoscopic-assisted vaginal hysterectomy, but first the mesh was separated from the pelvic sidewall at the level of the right uterosacral ligament and then laparoscopic assisted vaginal hysterectomy was performed without increased difficulty. None of the women who did not attend the invited follow up had a further prolapse operation according to our records from the Theatre Information Management System (TIMS). A total of 17 women (9 %) had further prolapse surgery or hysterectomy by the time of the review.
There was one intraoperative complication of broad ligament vascular injury requiring laparotomy. Her operation was completed and she had an uneventful recovery. Three patients developed lower abdominal discomfort, with occasional colicky pain, 4–8 months postoperatively, and underwent subsequent laparoscopies. Adhesions were noted between the bowel and non-peritonised mesh, which were carefully divided. Other complications reported by women included perineal infection, voiding difficulty, superficial dyspareunia and constipation which were most likely related to concomitant vaginal procedures performed at the time of hysteropexy operation. Complications and their frequency and percentage is summarized in Table 4. Codes for each type of complication is stated as per recommendation of IUGA/ICS joint terminology and classification of the complications [15]. No vaginal mesh exposure was observed on any of the women seen. None of the women have, so far, become pregnant in this cohort.
Discussion
We previously reported a very early outcome in 51 women, 10 weeks post-surgery [7]. We now report intermediate to late outcome on a 140 patients presenting with uterine prolapse, undergoing laparoscopic reconstructive uterine-sparing surgery, 1–4 years post-operatively (mean 2.1 years). It is, to our knowledge, the largest such study reported. One hundred and thirty-eight (99 %) felt that their prolapse was better using the PGI-I subjective assessment, while 125 (89 %) reported their prolapse to be “very much” or “much” better (see Fig. 1). Objective assessment using POP-Q scoring showed significant improvement in all parameters, the point C was elevated by a mean of 6.5 cm.
This technique of laparoscopic hysteropexy appears to have a low rate of serious complications (4 %). The risk of apical prolapse recurrence is also very low (4 %). There is high patient satisfaction as is evident in the PGI-I and recommendation of the operation to others in 92 % of women.
For some women in our study, restoration of uterine (apical) level I support led to a significant reduction in anterior vaginal wall prolapse and avoided the need for anterior repair at the time of hysteropexy. However, 26 women (19 %) required a concurrent anterior repair at the time of laparoscopic hysteropexy operation, and 10 women (7 %) subsequently had an anterior repair for cystocele. A further 35 women (25 %) had an anterior prolapse beyond the hymenal ring on examination at the 1- to 4-year follow-up, 60 % of these (21 women) were symptomatic and further surgery or physiotherapy treatment was offered.
Although some of the women were of reproductive age, none was actively trying to conceive at the time of review. The majority had completed their family and the few considering future conception had been explicitly informed that the effect of hysteropexy on pregnancy was unknown. They were also informed that delivery would require Caesarean section as the mesh completely encircled the cervix and would prevent cervical dilatation during labour.
The initial methods of uterine-sparing surgeries were described using a vaginal or open abdominal approach with variation in success [4]. Many previous papers have reported low numbers of cases with short-term follow up and selection bias.
The vaginal technique for uterine preservation most extensively reported has been sacrospinous hysteropexy. In the largest study 99 women were followed up for 23 months and reported an 84 % high satisfaction rate with recurrence of uterine prolapse in only 2 % of cases [16]. Cystocele recurrence was reported in 35 % of women; thus, the results are similar to those of our study.
In recent years advances in surgical techniques have allowed the option of laparoscopic pelvic floor reconstruction. Hysteropexy, as described in this report, is a laparoscopic variation of an open procedure, involving suspension of the uterus from the sacral promontory using bifurcated polypropylene mesh, originally described by Leron and Stanton in 2001 [17] using synthetic Teflon mesh. The laparoscopic approach allows superior visualisation of the anatomy with laparoscopic magnification, decreased hospital stay, reduced postoperative pain, rapid recovery and better cosmesis. One patient in our study required laparotomy for a haemorrhage and the senior author found completing hysteropexy via laparotomy a much more difficult technique; accessing the deep pelvis behind the uterus was problematic.
In other studies, apical support procedures such as sacrocolpopexy appear to improve the success of anterior repair [18, 19]. However, patients undergoing sacrocolpopexy, with or without paravaginal repair, still had a risk of anterior prolapse recurrence of 23 % [19]. Laparoscopic hysteropexy appears to play an important role in providing both apical (level I) support and reducing anterior prolapse, but a significant number of women required concomitant or subsequent surgery for vaginal prolapse. This is also consistent with other uterine- sparing operations [16, 20]. The anterior defect is probably explained by weakness in both level II as well as level I pelvic floor support, as described by DeLancey [21], and is therefore not always corrected with repair of the level I alone.
At the time of this study, only 3 women (2 %) had required a further operation for apical support for symptomatic prolapse. This appears to compare favourably with the risk of vault prolapse after vaginal hysterectomy [22]. There were no cases of mesh avulsion from the sacrum or cervix. Two women with recurrent uterine prolapse were treated very simply by plicating the mesh that was too loose, using polyester 2–0 sutures (Ethibond ExcelTM) and another 1 underwent cervical amputation. All these women had a successful outcome post-procedure up to the current time. The women with an elongated cervix were advised that the procedure may have limited success at the pre-operative counselling.
The use of prolene type 1 meshes in pelvic reconstructive surgery is well established for sacrocolpopexy and suburethral sling procedures. The risk of synthetic mesh exposure or extrusion is well recognized in pelvic vaginal prolapse surgery with an overall rate of up to 10 % reported [23]. There is a lower risk of mesh exposure with abdominal surgery compared with vaginal procedures [24]. In our study of laparoscopic hysteropexy, no cases of exposure, infection or rejection of the polypropylene mesh have occurred so far. The likelihood of vaginal mesh exposure should be low, as the mesh does not come into contact with the vaginal wall. So far, 3 women have been identified with adhesions of bowel to mesh, with subsequent development of symptoms and signs of chronic obstruction. These women had their operation in the early years when the mesh was not re-peritonised. Since this observation, our practice has been to peritonise the mesh completely and subsequently we have not had any patients with obstructive symptoms.
We found a significant improvement in urinary urge and stress incontinence in some women undergoing hysteropexy without concomitant continence surgery. This contradicts previous reports of lower urinary tract symptoms deteriorating post-prolapse surgery such as vaginal hysterectomy [25]. Although this study was not designed to assess the effect of prolapse surgery on continence, the improvement in urinary incontinence was detected on direct questioning and not using a validated outcome measure. The favourable outcome has changed our clinical practice. We advise, in patients presenting with concurrent symptoms of prolapse and incontinence, that anatomical defects are corrected initially. If lower urinary tract symptoms persist, we investigate and treat them subsequently.
There are some limitations to our study. First, 40 subjects did not attend the review 1–4 years post-surgery, which resulted in a 78 % follow-up rate. Some of those who did not attend contacted us and submitted their ICIQ-VS questionnaire, which had been sent to them prior to their appointment, confirming they were asymptomatic, thus declining their need for attendance. It is our impression that there was some bias with increased attendance by the women who were symptomatic. Second, pre-operative data, especially ICIQ-VS data, were not available in 63 women in the study. However, the result of change in the ICIQ-VS was significant in the 76 women who had completed both pre- and post-surgery questionnaires.
In our practice, the demand for uterine preservation during surgical management of utero-vaginal prolapse is increasing. However, current medical literature on this subject is inadequate to assist physicians in making an evidence-based decisions regarding uterine preservation vs hysterectomy, and with the former, select the ideal uterus-sparing procedure. At present, the decision is highly influenced by the patient’s preferences and the surgeon’s preference as well as their skill and experience. Well-designed comparative studies of pelvic floor reconstruction, both with and without hysterectomy, are currently not available. Studies involving more patients, appropriate controls and objective assessment techniques are necessary before uterine preservation can be routinely recommended at the time of uterovaginal prolapse surgery. We know from recent reports on sacrocolpopexy [26] that abdominal mesh surgical outcomes can deteriorate with time; thus, longer term follow-up for this procedure is required.
We are currently investigating further with a randomised controlled trial of laparoscopic hysteropexy and vaginal hysterectomy. A randomised, multicentre control trial in the UK is also planned, comparing uterine-preserving surgery with hysterectomy (VUE study) [27].
Conclusion
Our observational study suggests that laparoscopic hysteropexy might be effective in correcting uterine prolapse without recourse to hysterectomy. The operation appears to have a low rate of serious complications and a high satisfaction rate.
A prospective randomized trial comparing laparoscopic hysteropexy with conventional surgery such as vaginal hysterectomy is required to further evaluate and compare this procedure.
References
Abdel-Fattah M, Familusi A, Fielding S, Ford J, Bhattacharya S (2011) Primary and repeat surgical treatment for female pelvic organ prolapse and incontinence in parous women in the UK: a register linkage study. BMJ Open 1(2):e000206. doi:10.1136/bmjopen-2011-000206
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–506. doi:10.1016/S0029-7844(97)00058-6
Dallenbach P, Kaelin-Gambirasio I, Dubuisson JB, Boulvain M (2007) Risk factors for pelvic organ prolapse repair after hysterectomy. Obstet Gynecol 110(3):625–632. doi:10.1097/01.AOG.0000278567.37925.4e
Zucchi A, Lazzeri M, Porena M, Mearini L, Costantini E (2010) Uterus preservation in pelvic organ prolapse surgery. Nat Rev Urol 7(11):626–633. doi:10.1038/nrurol.2010.164
Maher CF, Feiner B, DeCuyper EM, Nichlos CJ, Hickey KV, O’Rourke P (2011) Laparoscopic sacral colpopexy versus total vaginal mesh for vaginal vault prolapse: a randomized trial. Am J Obstet Gynecol 204(4):360.e1–360.e7. doi:10.1016/j.ajog.2010.11.016
Smith SR, Solomon M (2010) Functional comparisons between open and laparoscopic rectopexy. Gastroenterol Clin Biol 34(10):505–507. doi:10.1016/j.gcb.2010.08.003
Price N, Slack A, Jackson SR (2010) Laparoscopic hysteropexy: the initial results of a uterine suspension procedure for uterovaginal prolapse. BJOG Int J Obstet Gynecol 117(1):62–68. doi:10.1111/j.1471-0528.2009.02396.x
Price N, Jackson SR, Avery K, Brookes ST, Abrams P (2006) Development and psychometric evaluation of the ICIQ vaginal symptoms questionnaire: the ICIQ-VS. BJOG Int J Obstet Gynecol 113(6):700–712. doi:10.1111/j.1471-0528.2006.00938.x
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175(1):10–17
Rahmanou P, Price N, Jackson S (2013) Laparoscopic Hysteropexy- A novel technique for uterine preservation surgery. Int Urogynecol J. doi:10.1007/s00192-013-2129-4
Elneil S, Cutner AS, Remy M, Leather AT, Toozs-Hobson P, Wise B (2005) Abdominal sacrocolpopexy for vault prolapse without burial of mesh: a case series. BJOG Int J Obstet Gynecol 112(4):486–489. doi:10.1111/j.1471-0528.2004.00426.x
Srikrishna S, Robinson D, Cardozo L (2010) Validation of the Patient Global Impression of Improvement (PGI-I) for urogenital prolapse. Int Urogynecol J 21(5):523–528. doi:10.1007/s00192-009-1069-5
Toozs-Hobson P, Freeman R, Barber M, Maher C, Haylen B, Athanasiou S, Swift S, Whitmore K, Ghoniem G, de Ridder D (2012) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse. Int Urogynecol J 23(5):527–535. doi:10.1007/s00192-012-1726-y
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21(1):5–26. doi:10.1007/s00192-009-0976-9
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, Dwyer PL, Fatton B, Kocjancic E, Lee J, Maher C, Petri E, Rizk DE, Sand PK, Schaer GN, Webb RJ (2011) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) & grafts in female pelvic floor surgery. Int Urogynecol J 22(1):3–15. doi:10.1007/s00192-010-1324-9
Dietz V, de Jong J, Huisman M, Schraffordt Koops S, Heintz P, van der Vaart H (2007) The effectiveness of the sacrospinous hysteropexy for the primary treatment of uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct 18(11):1271–1276. doi:10.1007/s00192-007-0336-6
Leron E, Stanton SL (2001) Sacrohysteropexy with synthetic mesh for the management of uterovaginal prolapse. BJOG Int J Obstet Gynecol 108(6):629–633
Stanford EJ, Cassidenti A, Moen MD (2012) Traditional native tissue versus mesh-augmented pelvic organ prolapse repairs: providing an accurate interpretation of current literature. Int Urogynecol J 23(1):19–28. doi:10.1007/s00192-011-1584-z
Shippey SH, Quiroz LH, Sanses TV, Knoepp LR, Cundiff GW, Handa VL (2010) Anatomic outcomes of abdominal sacrocolpopexy with or without paravaginal repair. Int Urogynecol J 21(3):279–283. doi:10.1007/s00192-009-1013-8
De Boer TA, Milani AL, Kluivers KB, Withagen MI, Vierhout ME (2009) The effectiveness of surgical correction of uterine prolapse: cervical amputation with uterosacral ligament plication (modified Manchester) versus vaginal hysterectomy with high uterosacral ligament plication. Int Urogynecol J Pelvic Floor Dysfunct 20(11):1313–1319. doi:10.1007/s00192-009-0945-3
DeLancey JO (1992) Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166(6 Pt 1):1717–1724; discussion 1724–1718
Prodigalidad LT, Peled Y, Stanton SL, Krissi H (2013) Long-term results of prolapse recurrence and functional outcome after vaginal hysterectomy. Int J Gynecol Obstet Off Organ Int Fed Gynaecol Obstet 120(1):57–60. doi:10.1016/j.ijgo.2012.07.022
Maher CM, Feiner B, Baessler K, Glazener CM (2011) Surgical management of pelvic organ prolapse in women: the updated summary version Cochrane review. Int Urogynecol J 22(11):1445–1457. doi:10.1007/s00192-011-1542-9
Visco AG, Weidner AC, Barber MD, Myers ER, Cundiff GW, Bump RC, Addison WA (2001) Vaginal mesh erosion after abdominal sacral colpopexy. Am J Obstet Gynecol 184(3):297–302. doi:10.1067/mob.2001.109654
Pakbaz M, Mogren I, Lofgren M (2009) Outcomes of vaginal hysterectomy for uterovaginal prolapse: a population-based, retrospective, cross-sectional study of patient perceptions of results including sexual activity, urinary symptoms, and provided care. BMC Womens Health 9:9. doi:10.1186/1472-6874-9-9
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, Fine P, Menefee S, Ridgeway B, Visco A, Warren LK, Zhang M, Meikle S (2013) Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA 309(19):2016–2024. doi:10.1001/jama.2013.4919
Glazener C (2013) Vault or uterine prolapse surgery evaluation: The VUE study. http://isrctn.org/ISRCTN86784244
Conflicts of interest
None.
Details of ethics approval
No ethical approval was required for this investigation as it was a simple observational study (clinical audit). Approval was obtained from the regional audit committee.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
A related video article can be found at 10.1007/s00192-013-2129-4.
Rights and permissions
About this article
Cite this article
Rahmanou, P., White, B., Price, N. et al. Laparoscopic hysteropexy: 1- to 4-year follow-up of women postoperatively. Int Urogynecol J 25, 131–138 (2014). https://doi.org/10.1007/s00192-013-2209-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2209-5