Abstract
Introduction and hypothesis
The aim was to compare objective and subjective cure rates between Uphold™ hysteropexy (HP) and vaginal hysterectomy (VH) with uterosacral suspension.
Methods
A sample size of 49 in each arm would be required to detect a clinical difference of 20% between the groups. Owing to delayed recruitment, this originally planned randomised controlled trial was changed to a patient preference study after randomising initial 6 participants. Women with symptomatic stage ≥2 uterine descent wishing a surgical solution were included. Routine follow-up was scheduled at 6 weeks, 6 months, 12 months, and annually thereafter. Primary outcome was absence of stage ≥2 apical prolapse. Secondary outcomes included a composite cure of no leading edge beyond the hymen, absence of bulge symptoms and no retreatment; patient-reported outcomes were based on quality-of-life questionnaires (PFDI-20, PFIQ-7, PISQ-12, PGI-I, EQ5D and a health score).
Results
We recruited 50 patients undergoing VH between 2011 and 2013 and 51 patients undergoing HP between 2011 and 2016. Participants were followed up for a median of 25 months (23–96). Five women from the VH (10%) and 7 from the HP (14%) group were lost to follow-up. Combined anatomical and symptomatic outcomes were available for 41 (82%) VH and 39 (76%) in the HP group. There was no difference in objective apical outcomes; the incidence of stage 2 prolapse was 0% in the VH group and 2% in HP group (p = 0.50). We found no difference in the composite cure rate (78% VH vs 85% HP, 0.45) between the groups. There was no significant difference in surgical complications (p = 0.33), assessed using Clavien–Dindo classification. There was a 2% surgery rate for mesh exposure in the HP group.
Conclusions
Uphold™ uterine suspension and VH appear to have similar objective and subjective cure at 25 months, with no significant difference in surgical complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is increasing recognition that women may wish to avoid hysterectomy at the time of pelvic organ prolapse (POP) surgery. Assuming equal outcomes between hysterectomy and uterine preservation surgery for POP, 36% of women preferred uterine preservation compared with 20% preference for hysterectomy [1]. Reasons quoted by women for uterine preservation vary from an impact on mood, relationships, sex drive and desire to maintain fertility [2]. Systematic review and retrospective studies have shown that uterine-preserving surgery is associated with reduced operating time, lower blood loss and faster recovery compared with POP surgery with hysterectomy [3].
Uterine-preserving surgeries can be performed by suture techniques or with mesh augmentation. Results from several retrospective comparative studies suggest that uterine conservation (using native tissue) did not appear to affect the risk of POP recurrence [4,5,6]. RCTs comparing sacrospinous hysteropexy against vaginal hysterectomy for uterine descent showed a reduced apical recurrence rate favouring hysterectomy at 12 months’ follow-up; however, there was no difference in functional outcome [7]. Mesh hysteropexy kits were developed with the view of improving long-term recurrence rates for POP. Systematic reviews had demonstrated a reduction in the recurrence rate of the anterior compartment when a synthetic mesh is utilised for POP repair [8]. The Cochrane review on transvaginal mesh concluded that mesh is associated with a higher re-operation rate and a lower rate of prolapse awareness and recurrence rates. Most studies had small patient numbers, a variety of mesh techniques and variable follow up. There are limited data comparing native tissue with mesh hysteropexy and results are not conclusive [3, 9].
The development of new products continues with the aim of having safe, effective alternatives to current treatment options for uterine conservation. The Uphold™ procedure was a minimally invasive vaginal approach to treating anterior/apical prolapse, utilising a well-established anterior approach to the sacrospinous ligament [10]. Non-comparative data showed a high success rate, low recurrence rate and mesh exposure rates between two and 7 % [11].
The primary aim of our study was to compare the safety and effectiveness of transvaginal mesh hysteropexy (HP) with vaginal hysterectomy (VH) and ipsilateral uterosacral suspension performed on both sides.
The hypothesis of our study is that HP would lead to a lower recurrence rate compared with VH (10% versus 30%).
Materials and methods
Study design, setting and population
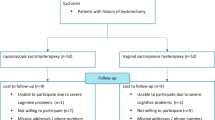
This study was planned and designed as an RCT, but changed to a patient preference study to optimise recruitment. Poor recruitment was due to the explicit desire of patients to choose either hysterectomy or uterine preservation rather than be randomised, and to the US Food & Drug Administration (FDA) warning update in 2011 regarding transvaginal mesh.
Study recruitment was conducted at a tertiary centre in Melbourne, Australia, between August 2011 and June 2016. Ethical approval was obtained from the local ethics committee and all women gave written informed consent (ACTRN12611000633987).
Initially, only 6 participants were randomised with equal probability to HP or VH using computer-generated random allocation in the first 3 months; the study was changed to patient preference for the remainder of the study. Randomisation occurred preoperatively once considered eligible and recruited to the trial.
Eligible participants included all patients with stage ≥2 (point C ≥ −1) symptomatic uterine descent referred for surgery, according to the Pelvic Organ Prolapse Quantification (POP-Q) system [12] and who had an ability to complete questionnaires and follow-up. Routine preoperative assessment including symptom evaluation, clinical examination, preoperative ultrasound and urodynamic assessment for co-existing stress urinary incontinence was performed, together with symptom and quality-of-life questionnaires. Urodynamic assessment was not performed universally; however, women were counselled regarding the risk of occult stress incontinence and temporary voiding dysfunction (VD). Participants who were randomised or chose hysteropexy underwent endometrial assessment using endometrial sampling (pipelle biopsy or hysteroscopy/curettage) at the time of surgery (if not before). Exclusion criteria included unevaluated dysfunctional menstrual (or post-menopausal) bleeding, unevaluated cervical smear abnormality, non-compliant with cervical screening, evidence of endometrial or cervical (including high-grade precancerous lesions) malignancy, incomplete family, previous synthetic mesh used for POP, lower urinary tract anomaly (congenital), neurogenic bladder disorders, previous radiation therapy to pelvis, past history of fistula involving the vagina and allergy to polypropylene or local anaesthetic.
Hysteropexy was initially performed utilising a midline anterior wall incision; however, it was changed to a transverse incision together with anterior repair. Uphold hysteropexy was performed as per the manufacturer’s instructions, together with any concomitant prolapse or continence surgery. Vaginal hysterectomy was performed in standard fashion, together with concomitant ipsilateral uterosacral suspension on both sides using 0 PDS sutures described by Shull et al. and any concomitant prolapse or continence surgery [13, 14]. Closure of the peritoneum was left to the discretion of the surgeon. If clinically indicated, a concomitant continence procedure was performed and a midurethral sling, either retropubic or transobturator, was placed via a separate incision. Cystoscopy was performed at the end of all the procedures. Participants received antibiotics and thromboprophylaxis, and routine postoperative and catheter care.
Demographic data collected included age, body mass index (BMI), parity, menopausal status, use of hormone replacement therapy (HRT) and previous POP or incontinence surgery. Post-operative follow-up was scheduled at 6 weeks, at 6, 12 and 24 months, and annually thereafter. Objective follow-up was performed by assessors independent of the operating surgeon. Each visit involved a POP-Q assessment and questionnaires. Subjective outcomes were assessed using the Pelvic Floor Distress Inventory 20 (PFDI−20) questionnaire [15]. The PFDI−20 includes 20 questions and three scales (the Urinary Distress Inventory-6 [UDI-6], the Pelvic Organ Prolapse Distress Inventory-6 [PDI-6], and the Colorectal–Anal Distress inventory-8 [CRADI-8]), each of which is scored from 0 to 100, and the overall summary score is gained by adding all the scales together. Impact on quality of life by pelvic floor disorders was assessed using the Pelvic Floor Impact Questionnaire (PFIQ -7) [15], sexual function by the Pelvic Organ Prolapse Urinary Incontinence Sexual Function Questionnaire (PISQ-12) [16]. Follow-up also assessed patient impression of improvement with Patient Global Impression of Improvement (PGI-I) [17]. Participants also completed EQ-5D [18] which is a standardised instrument developed by the EuroQol Group as a measure of health-related quality of life that can be used in a wide range of health conditions and treatments. The EQ-5D consists of a descriptive system and the EQ-VAS. The descriptive system comprises five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. The EQ-VAS records the patient’s self-rated health on a vertical visual analogue scale. Women who were physically unable to attend a postoperative visit were invited to complete the questionnaires over the phone. Complications were assessed at each visit and documented as per the Clavien–Dindo surgical complication grading system and the IUGA/ICS joint terminology for complications related to mesh [19, 20]. Prolonged catheterisation was defined as requiring an indwelling catheter (IDC) for more than 24 h. Chronic pelvic pain was defined as pelvic pain persistent for more than 6 weeks. Data were collected annually; however, if subjects missed a visit and subsequently came for follow-up, this was carried out retrospectively.
Outcome measures
The primary outcome was anatomical success defined as the absence of stage ≥2 apical prolapse (C below −1). Secondary outcomes included composite cure, quality-of-life measures (PFDI-20, PFIQ-7, PISQ, PGI-I, EQ5D and a health score) and complications. Composite cure was no leading edge beyond the hymen, absence of bulge symptoms on question 4 of the PDI-6, and no retreatment at 12 and 24 months. Assuming a recurrence rate of 30% for VH, with a power of 80%, a sample size of 49 in each arm would be required to detect a clinical difference of 20% with HP, using a one-sided α of 0.05. IBM SPSS version 20.0.0 (IBM Corp©) and GraphPad software version 8 (La Jolla, CA, USA) were used for statistical analysis. Outcomes were compared using Pearson’s Chi-squared test for categorical data and Student’s t test or Wilcoxon rank-sum for continuous data as appropriate. We attempted to contact all women lost to follow-up by phone and mail. A post-hoc sensitivity analysis was performed to assess the robustness of the findings.
Logistic regression was performed for composite outcome and patient-reported outcomes adjusted for known potential confounders such as age, BMI, parity, severity of POP at inclusion and concomitant incontinence procedure. Crude and adjusted odds ratios obtained by logistic regression analysis are reported with their respected 95% confidence intervals.
Results
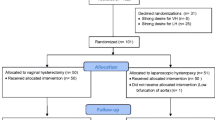
Of the 101 women included in the study, 50 underwent VH between August 2011 and November 2013 and 51 had transvaginal Uphold™ mesh hysteropexy between August 2011 and June 2016. Baseline demographics and POP-Q measurements between groups are displayed in Table 1. The groups were comparable for known confounders and risk factors for POP surgery failure. Seventy-eight percent (n = 39) of enrolled participants in the VH group and 60% (n = 31) in the hysteropexy group had concomitant posterior vaginal repair. Urodynamic assessment was performed in 10 patients; 3 (6%) and 6 (11%) women underwent mid-urethral sling procedures in the VH group and the hysteropexy group respectively. The flow of participants can be seen in Fig. 1. Participants were followed up for a median of 25 months (range 23–96) for both groups. Consecutive women requesting hysterectomy outnumbered those requesting mesh hysteropexy; the time to reach sample size for the hysteropexy group was more than double that of the hysterectomy group. Five women from the VH group (10%) and 7 from the HP (14%) group were lost to follow-up. Combined anatomical and symptomatic outcomes were available for 41 (82%) in the VH group and 39 (76%) in the hysteropexy group. There was no difference in objective apical outcomes; the incidence of stage 2 prolapse was 0% in the VH group and 2% in the hysteropexy group (p = 0.50). We found no difference in the composite cure rate (78% VH vs 85% HP, 0.45) between the groups (Fig. 2). Any compartment stage 2 prolapse in the VH group was 73% (30 out of 41), and 50% (20 out of 40) in the HP group (p = 0.04). Anterior wall recurrence (Ba> −1) occurred in 66% (27 out of 41) of the VH group and in 45% (18 out of 40) of the HP group. Total vaginal length (TVL) on POP-Q was greater in the hysteropexy group (p = 0.003; 9.5 cm vs 9 cm). A calculation assuming all missing data were anatomical failures (C below −1) showed no difference between the two groups (p = 0.62). Similarly, there was no difference between the groups when assuming all missing data to be failures for composite outcome (p = 0.82).
At the 12-month review, 1 participant in each group had recurrent prolapse surgery (VH: anterior repair and midurethral sling, HP: posterior repair). At the medium-term (84 months) follow-up, 1 participant from the HP group was scheduled for recurrent uterine prolapse surgery. A greater proportion of women had re-operation for stress urinary incontinence in the hysteropexy group 5 (13.1%) compared with 1 (2.3%) in the VH group, but this was not statistically significant (p = 0.09).
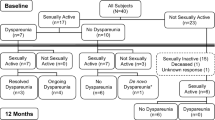
Overall, satisfaction was high for both groups with 80% (VH) and 84% (HP) reporting prolapse symptoms as “very much better” or “much better” on Patient Global Impression of Improvement (PGI-I) Table 2. Wherever there were missing data, these were obtained from the subsequent visit as last observed carried backwards. There was a significant improvement in patient-reported outcomes from baseline to follow-up for both groups in PFDI-20 (p = <0.0001), PFIQ-7 (p = <0.0001). Subscales POPDI-6 (p < 0.0001), CRAD-8 (VH p = 0.0002, HP p = 0.011), UDI-6 (VH p < 0.000, HP p = 0.0005) also showed statistically significant improvement (Fig. 3). Sexual function, which was assessed using PISQ-12, showed statistically significant improvement from baseline to follow-up in the VH group only. A total of 52 women (52%) were sexually active preoperatively and 49 (48%) at the medium-term follow-up. The mean total PISQ-12 score for VH at baseline and follow-up was 28.3 and 33.8 (VH p = 0.02) respectively. In the HP group the mean score was 30.9 at baseline and 32.9 at follow-up (p = 0.34). There was no significant difference in the PISQ-12 score between the groups at follow-up (p = 0.27). Within the VH group 54% (27 out of 50) were sexually active preoperatively and 40% (20 out of 50) postoperatively. For the HP group 49% (25 out of 51) reported being sexually active before surgery and 47% (24 out of 51) after surgery. Question 5 of the PISQ−12 assesses for dyspareunia; “Do you feel pain during sexual intercourse” and the responses can vary from 0 to 4 (never to daily). Figure 4 illustrates sexual function for the two groups pre- and post-surgery [21]. There was no statistical difference between the groups for the score at follow-up (p = 0.68).
Patient-reported outcomes using validated questionnaires. PFDI Pelvic Floor Distress Inventory, PFIQ Pelvic Floor Impact Questionnaire, PISQ-12 Pelvic Organ Prolapse/Incontinence Sexual Questionnaire, EQ5D Euroqol Five Dimensional, PGII Patient Global Impression of Improvement, MCID minimum clinical important difference
Sexual function pre - (top coloured box) and post - (3 outcomes below) intervention. Dyspareunia is defined as a response of “always”, “usually” or “sometimes” to the PISQ-12 question “Do you feel pain during sexual intercourse”. No dyspareunia was a response of “seldom” or “never” to the same question
Between the two groups at follow-up, POPDI-6 score had a statistically significant improvement in VH compared with the hysteropexy group (p = 0.04). There was no other difference in subjective outcomes between the groups.
After adjusting for baseline characteristics, there was no difference in the composite cure for HP vs VH (adjusted odds ratio [OR] 1.09; 95% confidence interval [CI] 0.26–4.47) (Supplementary Table 1). Similarly, there was no significant difference between the groups for patient-reported outcomes, except for POPDI-6 (adjusted OR 7.70; 95%CI, 1.85–13.55) and PFDI20 (adjusted OR 17.56; 95%CI, 1.89–33.23), which were found to be favouring VH (Supplementary Table 2).
There was no significant difference for estimated blood loss (EBL) and inpatient stay between the groups (p = 0.49, 0.82). Surgical complications were assessed using the Clavien–Dindo classification. Complications of grade I and above were compared and there was no significant difference between the two groups (p = 0.33). Mesh complications were low, with 2 cases of mesh exposure in the hysteropexy group (1 excised surgically, 1 conservative resolution). Both cases of mesh exposure were noted early at the 6-week post-operative review. According to the ICS/IUGA joint terminology prosthesis/graft complication classification both cases can be described as 2AT2S1 [22]. No further mesh exposure was noted once the anterior wall incision had been changed from vertical to transverse. There were no cases of mesh exposure or pain from midurethral slings. The majority of the complications were grade I or II, which resolved with prolonged catheterisation or oral antibiotics. Nine participants in the HP group and 1 in the VH group required prolonged catheterisation, of which 3 had a catheter for more than 7 days. All cases of retention resolved within 2 weeks post-operatively.
There were no cases of chronic pelvic pain in either group. The incidence of stress urinary incontinence (SUI) as determined by the UDI-6 question “Do you experience urine leakage related to physical activity, coughing or sneezing?” at the 24-month follow-up was 27% and 37% in the VH and HP groups respectively (p = 0.37). Overall rates of complications were low, with the commonest adverse event being urinary retention requiring prolonged catheterisation (Table 3).
Discussion
Uphold™ uterine suspension and repair and vaginal hysterectomy, suspension and repair appear to have a similar objective and subjective cure in the medium term, with no significant difference in surgical complications. Both procedures are safe and effective options for apical prolapse. Prolapse symptoms improved in 82% of participants (PGI-I) and overall there was an 80% composite cure rate at greater than 2 years.
We found no significant difference in the primary outcome with apical success and composite cure, which is similar to the SUPeR Trial (Study of Uterine Prolapse Procedures–Randomized Trial). The SUPeR study was the first long-term, multicentre, prospective, randomised trial comparing Uphold™ hysteropexy with hysterectomy and native tissue uterosacral ligament suspension [23] and also found no significant difference at 36 months for composite outcome. For anatomical outcomes, SUPeR trial reported better support for the anterior vaginal wall (Ba) in the HP group compared with the VH group. They found no difference in subjective outcomes. Also consistent with the SUPeR study, our cohort study reported a greater total vaginal length (TVL) and a lower rate of any compartment stage 2 or more prolapse, in particular, anterior wall recurrence in the hysteropexy group. If cure is defined as “no prolapse beyond the hymen”, the anterior vaginal wall recurrence rate in our series was 11%, which is consistent with that of other studies [3, 24].
Subjective outcomes were similar to those previously published, with significant improvement from baseline to follow-up, and no difference between the two groups for composite scores. The improvement exceeded the known minimum clinically important difference (MCID) of 45 points or 15% for PFDI−20 and 36 points or 12% for PFIQ-7 [15]. PFDI-20 and the subscale of POPDI−6 were found to be statistically significantly better in the VH group after controlling for confounders. This did not meet the known MCID for PFDI-20. In the absence of an established MCID for POPDI-6, 0.5 of the baseline standard deviation is a conservative estimate of MCID for patient-reported outcome measures [25]. Taking this into consideration, the statistically significant improvement for POPDI-6 in the VH group is unlikely to be of clinical significance. For sexual function assessed by the PISQ-12, there was statistical improvement in the VH group. The MCID for PISQ-12 is considered to be 2.3, which is derived from the MCID for PISQ-IR [26]. The improvement in the PISQ-12 score from baseline to follow-up met the MCID in the VH group but not in the HP group. At follow-up, 14% of participants within the VH group reported post-operative sexual inactivity compared with 2% in the HP group. The reason for sexual inactivity was not reported; this may be attributed to surgery or other factors such as lack or inability of a partner.
For both groups there was a low de novo post-operative dyspareunia rate, which is similar to the SUPeR trial. A recent meta-analysis by Liao et al. comparing female sexual function post-transvaginal mesh versus native tissue repair for prolapse showed no difference in sexual function and de novo dyspareunia [27]. There was no significant difference between the groups for de novo SUI. Lo et al. have previously reported a 20% incidence of de novo USI 12 months post-Uphold™ [28]. We found a slightly higher rate; however, our assessment was limited to questionnaires and was not confirmed on urodynamics.
We found no difference in the mean estimated blood loss (p = 0.49) or inpatient stay (p = 0.82) between groups. This is different to the systematic review comparing hysteropexy with hysterectomy, which reported reduced blood loss in the suture hysteropexy group [29]. The SuPER trial’s findings were more consistent with the systematic review, where they reported reduced blood loss and shorter operating time in the hysteropexy group [29]. The vaginal mesh exposure rate following Uphold hysteropexy has previously been reported to vary from 2 to 7% [11, 30]; our study was consistent with the lower number. The SUPeR trial reported a mesh exposure rate of 8%. Our study was not complicated by mesh exposure for midurethral slings or intraoperative ureteral kinking, in contrast to the latter complication occurring in 7% of the hysterectomy group in the SuPER trial. Ureteral kinking is a known potential complication for uterosacral suspension; it has also been reported following anterior approach sacrospinous hysteropexy either by suture or by mesh. Urinary retention was the commonest adverse event, with more episodes in the HP group than in the VH group. This could be due to a difference in the degree of reflection of the bladder from the cervix or the anterior vaginal wall or any sacrospinous space dissection. One limitation is that universal preoperative urodynamic assessment was not performed. The value of this could be two-fold to assess and predict for VD and occult SUI.
The overall rate of de novo SUI was only 5.7% and post-operative voiding dysfunction between 7 to 14 days was 30 %. It is not known if preoperative urodynamic assessment would have predicted voiding dysfunction. In our opinion this makes it difficult to justify a policy of universal urodynamic assessment prior to POP surgery.
Long-term outcomes for Uphold™ at 5 years were reported to be 97.5% success for apical (C < −TVL/2) and 78% for the anterior wall (Aa, Ba ≤0), by Rahkola-Soisalo et al. [31]. Jirschele et al. conducted a multicentre, prospective study in which they reported a composite outcome of 97.7% (Ba < −1) and 96.6% (C < −TVL/2) at 12 months. Our outcome is similar to the published literature for apical success at 97.8%. However, our success in terms of the anterior wall is lower than in other studies at 55%, which could be due to the definition used (Ba ≤ −1) and longer-term follow-up. Most studies describing the Uphold procedure are retrospective or prospective observational studies, without controls and 12-month follow-up [30]. There are limited data comparing Uphold™ hysteropexy with VH. Most of the hysterectomies performed at the time of uterovaginal prolapse are devoid of any pathology. The rationale for a concomitant hysterectomy at the time of prolapse repair has been better visualisation and access to apical support ligaments and prevention of future cervical elongation or uterocervical pathology. In studies other than ours, this approach is associated with a longer operating time, increased blood loss and longer hospital stay. There is also an increased risk of accelerated ovarian failure [32].
The strengths of this study include a prospective comparison of two procedures for uterine prolapse, use of composite outcomes, comparable demographic groups, validated quality-of-life questionnaires for subjective outcomes and post-operative objective outcomes assessed by independent examiners.
Limitations include a lack of randomisation due to poor recruitment post-FDA mesh notification and update, one-sided difference test and the lack of blinding of patients or assessors. The majority of the trial was not randomised, and this may lead to bias introduced by unmeasured confounders. If power analysis was based on a two-sided difference test, our study is underpowered to detect the primary outcome. The participants were unblinded and they may have a bias towards the procedure they chose. Although the postoperative outcome was assessed by a clinician other than the operating surgeon, the examiner would have been able to identify the intervention group based on the presence or absence of the cervix, potentially adding to examiner bias. In addition, there was an approximately 15% loss to follow-up in the medium term. This study was conducted at a tertiary referral centre by certified urogynaecologists and these findings may not be generalisable to all surgeons.
Transvaginal mesh for prolapse repair was reclassified as a class III device by the FDA in 2016. Transvaginal mesh was cancelled from the Therapeutics Goods Administration (TGA) in Australia [33] in January 2018. In April 2019, the FDA announced that transvaginal mesh kits would no longer be available, as their superiority to native tissue repair for anterior and apical prolapse had not been shown [34].
Based on our findings and those of other Uphold series, we would counsel women who prefer uterine conservation surgery for POP that they would have similar outcomes to hysterectomy with minimal difference in surgical complications and a low rate of mesh-related complications.
Conclusion
For women undergoing vaginal surgery for uterovaginal prolapse, there is no significant difference between Uphold™ hysteropexy and vaginal hysterectomy at a median follow-up of 25 months. The Uphold procedure is no longer available and future research with alternative methods of hysteropexy with long-term outcomes is needed.
References
Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470 e471–6. https://doi.org/10.1016/j.ajog.2013.08.003.
Frick AC, Barber MD, Paraiso MF, Ridgeway B, Jelovsek JE, Walters MD. Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female Pelvic Med Reconstr Surg. 2013;19(2):103–9. https://doi.org/10.1097/SPV.0b013e31827d8667.
Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013;24(11):1803–13. https://doi.org/10.1007/s00192-013-2171-2.
Hefni M, El-Toukhy T, Bhaumik J, Katsimanis E. Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obstet Gynecol. 2003;188(3):645–50. https://doi.org/10.1067/mob.2003.75.
Maher CF, Cary MP, Slack MC, Murray CJ, Milligan M, Schluter P. Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(6):381–4 discussion 384–385.
Van Brummen HJ, van de Pol G, Aalders CI, Heintz AP, van der Vaart CH. Sacrospinous hysteropexy compared to vaginal hysterectomy as primary surgical treatment for a descensus uteri: effects on urinary symptoms. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(5):350–5; discussion 355. https://doi.org/10.1007/s00192-003-1084-x.
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J. 2010;21(2):209–16. https://doi.org/10.1007/s00192-009-1014-7.
Jia X, Glazener C, Mowatt G, Jenkinson D, Fraser C, Bain C, et al. Systematic review of the efficacy and safety of using mesh in surgery for uterine or vaginal vault prolapse. Int Urogynecol J. 2010;21(11):1413–31. https://doi.org/10.1007/s00192-010-1156-7.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012079. https://doi.org/10.1002/14651858.CD012079.
Goldberg RP, Tomezsko JE, Winkler HA, Koduri S, Culligan PJ, Sand PK. Anterior or posterior sacrospinous vaginal vault suspension: long-term anatomic and functional evaluation. Obstet Gynecol. 2001;98(2):199–204.
Vu MK, Letko J, Jirschele K, Gafni-Kane A, Nguyen A, Du H, et al. Minimal mesh repair for apical and anterior prolapse: initial anatomical and subjective outcomes. Int Urogynecol J. 2012;23(12):1753–61. https://doi.org/10.1007/s00192-012-1780-5.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7. https://doi.org/10.1016/s0002-9378(96)70243-0.
Shull BL, Bachofen C, Coates KW, Kuehl TJ. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol. 2000;183(6):1365–73; discussion 1373-4. https://doi.org/10.1067/mob.2000.110910.
Joint Writing Group of the American Urogynecologic Society and the International Urogynecological Association. Joint report on terminology for surgical procedures to treat pelvic organ prolapse. Int Urogynecol J. 2020;31(3):429–63. https://doi.org/10.1007/s00192-020-04236-1.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI−20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13. https://doi.org/10.1016/j.ajog.2004.12.025.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(3):164–8; discussion 168. https://doi.org/10.1007/s00192-003-1063-2.
Srikrishna S, Robinson D, Cardozo L. Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–8. https://doi.org/10.1007/s00192-009-1069-5.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36. https://doi.org/10.1007/s11136-011-9903-x.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. https://doi.org/10.1097/SLA.0b013e3181b13ca2.
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Int Urogynecol J. 2011;22(1):3–15. https://doi.org/10.1007/s00192-010-1324-9.
Toozs-Hobson P, Freeman R, Barber M, Maher C, Haylen B, Athanasiou S, et al. An International Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse. Neurourol Urodyn. 2012;31(4):415–21. https://doi.org/10.1002/nau.22238.
Haylen BT, Maher C, Deprest J. IUGA/ICS terminology and classification of complications of prosthesis and graft insertion—rereading will revalidate. Am J Obstet Gynecol. 2013;208(1):e15. https://doi.org/10.1016/j.ajog.2012.08.004.
Nager CW, Visco AG, Richter HE, Rardin CR, Rogers RG, Harvie HS, et al. Effect of vaginal mesh hysteropexy vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: a randomized clinical trial. JAMA. 2019;322(11):1054–65. https://doi.org/10.1001/jama.2019.12812.
Roovers JP, van der Vaart CH, van der Bom JG, van Leeuwen JH, Scholten PC, Heintz AP. A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG. 2004;111(1):50–6.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–92. https://doi.org/10.1097/01.MLR.0000062554.74615.4C.
Pellino G, Ramage L, Simillis C, Warren O, Kontovounisios C, Tan E, et al. Evaluation of sexual dysfunction in female patients presenting with faecal incontinence or defecation disorder. Int J Colorectal Dis. 2017;32(5):667–74. https://doi.org/10.1007/s00384-017-2795-7.
Liao SC, Huang WC, Su TH, Lau HH. Changes in female sexual function after vaginal mesh repair versus native tissue repair for pelvic organ prolapse: a meta-analysis of randomized controlled trials. J Sex Med. 2019;16(5):633–9. https://doi.org/10.1016/j.jsxm.2019.02.016.
Lo TS, Pue LB, Tan YL, Hsieh WC, Kao CC, Uy-Patrimonio MC. Anterior-apical single-incision mesh surgery (uphold): 1-year outcomes on lower urinary tract symptoms, anatomy and ultrasonography. Int Urogynecol J. 2019;30(7):1163–72. https://doi.org/10.1007/s00192-018-3691-6.
Meriwether KV, Antosh DD, Olivera CK, Kim-Fine S, Balk EM, Murphy M, et al. Uterine preservation vs hysterectomy in pelvic organ prolapse surgery: a systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol. 2018;219(2):129–146.e2. https://doi.org/10.1016/j.ajog.2018.01.018.
Jirschele K, Seitz M, Zhou Y, Rosenblatt P, Culligan P, Sand P. A multicenter, prospective trial to evaluate mesh-augmented sacrospinous hysteropexy for uterovaginal prolapse. Int Urogynecol J. 2015;26(5):743–8. https://doi.org/10.1007/s00192-014-2564-x.
Rahkola-Soisalo P, Mikkola TS, Altman D, Falconer C, Nordic TVMG. Pelvic organ prolapse repair using the uphold vaginal support system: 5-year follow-up. Female Pelvic Med Reconstr Surg. 2019;25(3):200–5. https://doi.org/10.1097/SPV.0000000000000530.
Moorman PG, Myers ER, Schildkraut JM, Iversen ES, Wang F, Warren N. Effect of hysterectomy with ovarian preservation on ovarian function. Obstet Gynecol. 2011;118(6):1271–9. https://doi.org/10.1097/AOG.0b013e318236fd12.
Therapeutic Goods Administration (2019) Transvaginal (urogynaecological) surgical mesh. https://www.tga.gov.au/hubs/transvaginal-mesh.
U.S. Food & Drug Administration (2019) Urogynecologic surgical mesh implants. https://www.fda.gov/medical-devices/implants-and-prosthetics/urogynecologic-surgical-mesh-implants.
Authors’ participation
M. Kulkarni: follow-up, database, manuscript preparation; N. Young: study design, recruitment, follow-up, database, manuscript preparation; J. Lee: study design, recruitment, follow-up, database, manuscript preparation; A. Rosamilia: study design, recruitment, follow-up, database, manuscript preparation.
Funding
This study was an investigator-initiated and -led study with financial support from Boston Scientific. These funds were transferred to Monash University fund at arm’s length from the investigators and used to fund a research nurse salary and other costs related to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
M. Kulkarni: none; N. Young: none; J. Lee: this study was an investigator-initiated and -led study with financial support by Boston Scientific. These funds were transferred to Monash University fund at arm’s length from the investigators and used to fund research nurse salary and other costs related to the study; A. Rosamilia: this study was an investigator-initiated and -led study with financial support by Boston Scientific. These funds were transferred to Monash University fund at arm’s length from the investigators and used to fund research nurse salary and other costs related to the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Kulkarni, M., Young, N., Lee, J. et al. Hysterectomy with uterosacral suspension or Uphold™ hysteropexy in women with apical prolapse: a parallel cohort study. Int Urogynecol J 31, 2137–2146 (2020). https://doi.org/10.1007/s00192-020-04328-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04328-y