Abstract
Introduction and hypothesis
To evaluate the relationship between pelvic organ prolapse (POP) staging and clinical findings, lower urinary tract symptoms (LUTS), sexual dysfunction, and quality of life (QoL) using validated questionnaires.
Methods
Women attending the urogynecology unit with LUTS and/or bulging (n = 388) were grouped according to the POP quantification (POPQ). LUTS, sexual dysfunction, and QoL were evaluated using the Urinary Distress Inventory-6 (UDI-6),the Overactive Bladder Awareness tool (OAB-V8), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), and the Incontinence Impact Questionnaire-7 (IIQ-7). Data regarding baseline characteristics, clinical findings, and scores of questionnaires were compared among the POP stages using the Kruskal–Wallis test. Pearson’s and Spearman’s correlation analyses were used to evaluate the correlation of POP staging with clinical findings, pelvic floor dysfunction related symptom severity, and QoL.
Results
According to the POPQ, patients were classified as: stage 0 (27.8 %), stage 1 (21.4 %), stage 2 (38.9 %), and stages 3 and 4 (11.8 %). Irritative, stress, obstructive subscale scores of UDI-6 and physical, travel, emotional subscale scores of IIQ-7 were significantly different among POPQ stages. Weak correlations between POPQ staging and irritative, stress, obstructive subscale scores of UDI-6 (r = 0.198, r = 0.192, and r = 0.146 respectively), and physical, travel, social, emotional subscale scores of IIQ-7 (r = 0.223, r = 0.154, r = 120 and r = 0.171 respectively) were found (p < 0.05). Clinical findings (Q-tip and stress test positivity, post-void residual volumes) showed moderate to weak correlations with POPQ stages (r = 0.425, r = 0.117, r = 0.163 respectively; p < 0.05).
Conclusions
The correlation of lower urinary tract dysfunction and POP staging was shown to be best represented by UDI-6 and IIQ-7.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) is a very common disorder, observed in 38–75 % of women attending for gynecological care [1]. Women with prolapse may present with a wide range of lower urinary tract symptoms; stress urinary incontinence, urgency, frequency, and urge incontinence have been reported in 40 %, 34 %, 29 %, and 30 % of women with POP respectively [2, 3]. Understanding the relationship between POP and pelvic floor symptoms is a crucial step in the management of patients. The symptoms are largely subjective in nature [4], and contradictory results have been reported regarding the association of POP with lower urinary tract symptoms (LUTS) and sexual dysfunction [5–10]. The lifetime risk of undergoing surgery for prolapse has been reported to be 11 % by the age of 80 and approximately one third of these women undergo repeat surgery [11]. Success of surgical outcome has usually been described as “improvement in anatomical support”. However, pelvic reconstructive surgery does not always provide functional improvement and patient satisfaction. To determine the patients’ needs and expectations correctly, it is important to evaluate their perception of the condition and its reflection on quality of life (QoL) [4]. Thus, in addition to objective and anatomical measures, functional aspects of POP should be assessed with validated questionnaires to make a complete clinical decision plan: addressing the goals of both the patient and the physician. In this respect, various general and disease-specific instruments have evolved for the assessment of the functional aspects of pelvic floor disorders and have been validated in different languages; still, their results may be affected by cultural and religious differences [4].
Two of the most common disease-specific instruments designed specifically for urinary incontinence are the Urinary Distress Inventory (UDI) and the Incontinence Impact Questionnaire (IIQ) [12], which have been shown to be useful and reliable in classifying urinary distress and in measuring associated symptom bother. Short versions of these questionnaires (UDI-6 and IIQ-7) have been developed in order to be more practical, less time-consuming, and easy to interpret; both have been proven to be well-correlated with the longer forms [13] and have been validated in Turkish [14].
The Overactive Bladder Awareness tool (OAB-V8) is a screening instrument derived from the first 8 questions of the 33 item OAB-q questionnaire and was developed to improve the detection of OAB symptoms and their severity; it has been shown to be helpful in identifying patients who may benefit from treatment [15, 16]. A validated Turkish version is available [17, 18].
The Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ) is a validated QOL instrument measuring the impact of POP and/or urinary incontinence on sexual function with 31 items and three domains (behavioral/emotive, physical, and partner related) [19]. A more easily administered validated short form (PISQ-12) has been developed [20] and validated in Turkish [21].
Materials and methods
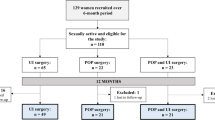
This is a cross-sectional observational study of women with LUTS and/or bulge symptoms attending the urogynecology unit of Ankara University, School of Medicine between January 2009 and April 2012. All women (n = 388) were evaluated by the routine urogynecological examination including simplified Pelvic Organ Prolapse Quantification (POPQ) staging performed in the lithotomy position, as described in the POPQ system by the International Continence Society Committee on Standardization of Terminology [22]. The patients were then grouped according to the POPQ stages; women with prolapse in multiple compartments were assigned to the stage of the most dependent compartment. Available data regarding baseline characteristics, clinical findings and questionnaires measuring pelvic floor dysfunction and QoL were analyzed. Age, body mass index (BMI), parity, and medical and surgical history were recorded as baseline characteristics. Clinical findings included the cough stress test, Q-tip test and post-void residual (PVR) urine, which was measured by catheterization in 5 min after micturition. All women underwent the cough stress test and the Q-tip test, and the PVR was measured in patients accepting this procedure (n = 301). Lower urinary tract symptoms, sexual dysfunction, and QoL were evaluated using the questionnaires, which were self-administered and fulfilled accurately by the patients (UDI-6 n = 305; IIQ-7 n = 262; OAB-V8 n = 214 and PISQ-12 n = 109). The distribution of POPQ stages of patients responding to each questionnaire was analyzed separately. The baseline characteristics of each patient group with related questionnaires were also analyzed separately with the aim of establishing possible biases that may interfere with the overall results of the study. Comparison and correlation analyses among POP stages were performed with data of patients responding to each questionnaire.
The UDI-6 consists of six questions and three subscales; irritative symptoms are represented by questions 1 and 2, stress symptoms are represented by questions 3 and 4, and obstructive/voiding difficulty symptoms are represented by questions 5 and 6. In this study, analysis was performed with the total UDI-6 score and the irritative, stress and obstructive subscales’ scores of UDI-6 separately. For each symptom/question, responses were graded on a four-point scale from 0 (not at all) to 3 (greatly). The scores were converted to a range between 0 and 100. Higher scores indicate more symptoms and increased symptom bother.
Similarly, the IIQ-7 was assessed with the total score and the subscale scores (physical, travel, social and emotional). The response scale is the same as the UDI-6. The scores were converted to a range between 0 and 100. Higher scores indicate greater impact on QoL.
The OAB-V8 comprises eight questions evaluating urinary frequency, nocturia, urgency, and urge incontinence. Reponses are graded on a six-point scale from 0 (not at all) to 5 (a very great deal).
The PISQ-12 comprises 12 questions and three subscales; behavioral/emotive factors are represented by questions 1–4, physical factors by questions 5–9 and partner-related factors by questions 10–12. Responses are graded on a five-point scale from “never” to “always”. Reverse scoring is used for questions 1–4. The maximum total score is 48 and higher scores indicate better sexual functioning.
Statistical analysis was performed with SPSS version 13.0 for Windows (SPSS, Chicago, IL, USA). The comparison of baseline characteristics, clinical findings, LUTS, sexual function, and QoL among POP stages was made using the Kruskal–Wallis test. Pearson’s and Spearman’s correlation analyses were used to evaluate the correlation of POPQ stages with symptom severity, clinical findings and QoL scores. P < 0.05 was considered statistically significant.
Results
A total of 388 women were enrolled and classified according to POPQ stages (stage 0: n = 108, 27.8 %; stage 1: n = 83, 21.4 %; stage 2: n = 151, 38.9 %; stage ≥3: n = 46, 11.8 %). Of these women, 255 had anterior, 84 had apical, and 173 had posterior prolapse (Table 1), with overlap, as most women had prolapse in multiple compartments (n = 179). Baseline characteristics of the whole study population are shown in Table 2. Mean age, menopausal status, and BMI were similar in patients with stage 0 and stage ≥3. Body mass index of patients with stage 2 prolapse was found to be higher than stage 0 (p = 0.006), no significant difference was found among other stages. Postmenopausal women more frequently had stages 0 and 3 and 4 than stages 1 and 2 (p = 0.004). Diabetes was more frequent in women with stage 0 (p = 0.021). Parity, previous pelvic surgery, and chronic obstructive lung disease were similar among all stages of POP.
Clinical findings showed significant differences among POP stages (p < 0.05; Table 3). Among 388 patients, the Q-tip test was positive in 201 (51.8 %) and the stress test was positive in 167 patients (43 %). Q-tip test positivity was highest in patients with stage ≥3 (p = 0.00) and stress test positivity was highest in stages 1 and 2 (p = 0.00). The PVR measurements were available for 301 patients (stage 0: n = 57, 18.9 %; stage 1: n = 74, 24.6 %; stage 2: n = 129, 42.9 %; stages 3 and 4: n = 41, 13.6 %). The PVR volumes were higher in patients with stage ≥2 (p = 0.047). The significant difference between stages in terms of age, menopausal status, and diabetes disappeared (p > 0.05). Body mass index of patients with stage 2 prolapse was found to be higher than in those with stage 0 (p = 0.007); the baseline characteristics other than the BMI were all similar among POP stages in patients with PVR measurements.
On correlation analysis, the Q-tip test, stress test, and PVR had significantly positive, moderate to weak correlations with POPQ stages (r = 0.425, r = 0.117, r = 0.163 respectively; p < 0.05).
Comparison and correlation analyses among POP stages were performed separately with data of each questionnaire that was fulfilled accurately (UDI-6 n = 305, IIQ-7 n = 262, OAB-V8 n = 214 and PISQ-12 n = 109). Distribution of POP stages for each questionnaire was similar and also showed similarity to the stages of whole study population. Body mass index of patients with stage 2 prolapse was found to be higher than in those with stage 0 (p < 0.02) for all questionnaires except for the PISQ-12, where the BMI was similar among all POP stages. Among women responding to the OAB-V8, more women with stage ≤1 had undergone previous pelvic surgery than women with stages ≥2 (13.6 % vs 3.8 %, p = 0.016). The remaining baseline characteristics were all similar among POP stages of each patient group responding to each questionnaire.
Total scores for the UDI-6, IIQ-7, OAB-V8, and PISQ-12 questionnaires did not differ among the POP stages (Table 4). However, irritative, stress and obstructive subscales of UDI-6, and physical, travel and emotional subscales of IIQ-7 showed significant differences among the stages (Table 5). Irritative and stress symptom scores were significantly higher in patients with stage ≥2 (p = 0.005 and 0.009 respectively); obstructive symptom scores were higher in patients with stage ≥3 (p = 0.05). For IIQ-7 subscales, scores of symptom bother with physical activity were similar in patients with stage 0 and stage 1 prolapse (p = 0.318). Compared with patients with stage 0 and stage 1, patients with stage ≥2 had higher physical activity-related symptom bother scores (p < 0.05). Travel-associated symptom scores were significantly higher in patients with stage ≥3 than patients with stage 0 (p = 0.009). Emotional health was significantly worse in patients with stage ≥3 than in patients with stage 0 (0.001).
Correlation analysis showed a significant positive relationship between POP stages and total scores of UDI-6, and the subscale scores of UDI-6 and IIQ-7 (Table 6). The irritative and stress subscale scores of the UDI-6 were found to correlate with each other (r = 0.688, p = 0.000).
Discussion
Women presenting with POP report a variety of pelvic floor disorder symptoms; LUTS are common in women with POP [2, 3, 23, 24]. However, the relationship between POP severity and LUTS has been evaluated in only a few studies and still remains unclear. In this study, LUTS were found to be more common and bothersome in women with advancing prolapse and were best represented by the subscales of UDI-6 and IIQ-7. Patients with advanced prolapse have been shown to encounter obstructive urinary symptoms [3, 23, 24]. Consistently, in this study, obstructive symptom scores were more prominent (p = 0.05) in patients with stages 3 and 4 and expectedly, irritative symptom scores were found to be higher in these patients (p = 0.005). Accordingly, PVR volumes were significantly higher in patients with stage ≥2 (p = 0.047).
From previous reports, women with advanced prolapse are less likely expected to have stress urinary incontinence [5–7]. However, in our study, stress symptom scores of the UDI-6 were found to increase with advancing prolapse and a weak positive correlation was found between POP stages and both the stress test and stress subscale scores of UDI-6. Hypermobility of the urethra increased with advancing prolapse and was found to be moderately correlated with POP stages. This may in part be explained by the presence of fewer patients with stage 4 prolapse in our population, that is, there were fewer patients with prolapse that might cause kinking and obstruction of the urethra. Additionally, irritative and stress symptom scores of the UDI-6 were interrelated; the stress scores increased as the irritative scores increased. The associated symptom bother and QoL, measured by the IIQ-7, was also significantly worse in these patients with advancing prolapse. Therefore, it can be pointed out that urinary distress due to prolapse may consist of a wide spectrum of symptoms, which may be related to the same etiopathogenesis.
These findings confirm the results of the study by Lowder et al., who showed that mixed urinary incontinence symptoms were the most common urinary symptom type among women with POP. They reported that urge and stress symptoms were associated with each other and bother by one symptom type was predictive of bother by another, and that the UDI appears to be an effective tool in evaluating symptoms in this population [25].
Studies that have investigated the association of POP with LUTS have reported either weak to moderate correlations [5–7] or no association other than bulge symptoms [8–10]. In this study the UDI-6 and IIQ-7 scores were found to be significantly, but weakly correlated with POP stages.
The effect of POP on sexual function is controversial. Decreased sexual function was demonstrated in women with POP compared with unaffected women [26]. However, Lukacz et al. have demonstrated that although women with pelvic floor disorders were less likely to be sexually active, they were found to be equally as sexually active when data were controlled for confounders such as age, menopausal status, and sexual desire. These factors were shown to be the only significant contributors to decreased sexual function [27]. Similarly, Burrows et al. reported that measures of sexual function showed no significant difference between women with or women without POP [6]. We also found no differences in sexual function measured by the PISQ-12 among POP stages.
The strength of the study is that we evaluated the functional aspects of prolapse from the patients’ perspective by using accepted, recommended, and Turkish-validated symptom and QoL questionnaires. The limitation of the study may be its design; data derived from the records of patients attending with lower urinary tract and/or prolapse complaints were analyzed in terms of POP stages. We also included women with POP stages 0 and 1 whose complaints were only LUTS and/or sexual dysfunction. Nevertheless, there were still significant differences in symptom bother among the stages. Although our patient population may lead to selection bias and limit the generalizability of the results to the general population, it is obvious that women with advanced prolapse had more urinary distress than women attending with LUTS and/or sexual dysfunction as their sole complaint. In our opinion, the difference among POP stages in terms of pelvic floor disorder-related symptoms could have been more pronounced if there had been an ideal control group in a well-designed prospective study.
In conclusion, LUTS seems to be more prominent in patients with advanced prolapse and the associated QoL is worse; the UDI-6 and IIQ-7 are useful tools in the evaluation of these patients, supported by and consistent with the clinical findings. Sexual function does not seem to be adversely affected by POP stages measured by the total score of PISQ-12 in this group of patients.
References
Swift S, Woodman P, O’Boyle A, Kahn M, Valley M, Bland D, Wang W, Schaffer J (2005) Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol 192:795–806
Grody MH (1998) Urinary incontinence and concomitant prolapse. Clin Obstet Gynecol 41:777–785
De Boer TA, Slieker-ten Hove MCP, Burger CW, Vierhout ME (2011) The prevalence and risk factors of overactive bladder symptoms and its relation to pelvic organ prolapse symptoms in a general female population. Int Urogynecol J 22:569–575
Ghoniem G, Stanford E, Kenton K, Achtari C, Goldberg R, Mascarenhas T, Parekh M, Tamussino K, Tosson S, Lose G, Petri E (2008) Evaluation and outcome measures in the treatment of female urinary stress incontinence: International Urogynecological Association (IUGA) guidelines for research and clinical practice. Int Urogynecol J 19:5–33
Salvatore S, Serati M, Siesto G, Cattoni E, Zanirato M, Torella M (2011) Correlation between anatomical findings and symptoms in women with pelvic organ prolapse using an artificial neural network analysis. Int Urogynecol J 22:453–459
Burrows LJ, Meyn LA, Walters MD, Weber AM (2004) Pelvic symptoms in women with pelvic organ prolapse. Obstet Gynecol 104:982–988
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE (2001) Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol 185:1332–1338
Broekhuis SR, Hendriks JCM, Futterer JJ, Vierhout ME, Barentsz JO, Kluivers KB (2010) Perineal descent and patients’ symptoms of anorectal dysfunction, pelvic organ prolapse, and urinary incontinence. Int Urogynecol J 21:721–729
Ghetti C, Gregory WT, Edwards SR, Otto LN, Clark AL (2005) Pelvic organ descent and symptoms of pelvic floor disorders. Am J Obstet Gynecol 193:53–57
Gutman RE, Ford DE, Quiroz LH, Shippey SH, Handa VL (2008) Is there a pelvic organ prolapse threshold that predicts pelvic floor symptoms? Am J Obstet Gynecol 199:683.e1–683.e7
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA (1994) Health-related QOL measures for women with urinary incontinence: the incontinence impact questionnaire and urogenital distress inventory. Qual Life Res 3:291–306
Uebersax JS, Wyman JF, Shumaker SA, McClish D, Fantl JA (1995) Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and urogenital distress inventory. Neurourol Urodyn 14:131–139
Cam C, Sakalli M, Ay P, Cam M, Karateke A (2007) Validation of the short forms of the Incontinence Impact Questionnaire (IIQ – 7) and the Urogenital Distress Inventory (UDI – 6) in a Turkish population. Neurourol Urodynamics 26:129–133
Coyne KS, Zyczynski T, Margolis MK, Elinoff V, Roberts RG (2005) Validation of an overactive bladder awareness tool for use in primary care settings. Adv Ther 22:381–394
Basra RK, Cortes E, Khullar V, Kelleher C (2012) A comparison study of two lower urinary tract symptoms screening tools in clinical practice: the B-SAQ and OAB-V8 questionnaires. J Obstet Gynecol 32:666–671
Acquadro C, Kopp Z, Coyne KS, Corcos J, Tubaro A, Choo MS (2006) Translating overactive bladder questionnaires in 14 languages. Urology 67:536–540
Coyne KS, Margolis MK, Thompson C, Kopp Z (2008) Psychometric equivalence of the OAB-q in Danish, German, Polish, Swedish and Turkish. Value Health 11:1096–1101
Rogers RG, Kammerer-Doak D, Villarreal A, Coates K, Qualls C (2001) A new instrument to measure sexual function in women with urinary incontinence or pelvic organ prolapse. Am J Obstet Gynecol 184:552–558
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C (2003) A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct 14:164–168
Cam C, Sancak P, Karahan N, Sancak A, Celik C, Karateke A (2009) Validation of the short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12) in a Turkish population. Eur J Obstet Gynecol Reprod Biol 146:104–107
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
Romanzi LJ, Chaiken DC, Blaivis JG (1999) The effect of genital prolapse on voiding. J Urol 161:581–586
Yalcin OT, Yildirim A, Hassa H (2001) The effects of severe cystocele on urogynecologic symptoms and findings. Acta Obstet Gynecol Scand 80:423–427
Lowder JL, Frankman EA, Ghetti C, Burrows LJ, Krohn MA, Moalli P, Zyczynski H (2010) Lower urinary tract symptoms in women with pelvic organ prolapse. Int Urogynecol J 21:665–672
Novi JM, Jeronis S, Morgan MA, Arya LA (2005) Sexual function in women with pelvic organ prolapse compared to women without pelvic organ prolapse. J Urol 173:1669–1672
Lukacz ES, Whitcomb EL, Lawrence JM, Nager CW, Contreras R, Luber KM (2007) Are sexual activity and satisfaction affected by pelvic floor disorders? Analysis of a community-based survey. Am J Obstet Gynecol 197:88.e1–88.e6
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cetinkaya, S.E., Dokmeci, F. & Dai, O. Correlation of pelvic organ prolapse staging with lower urinary tract symptoms, sexual dysfunction, and quality of life. Int Urogynecol J 24, 1645–1650 (2013). https://doi.org/10.1007/s00192-013-2072-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2072-4