Abstract
Introduction and hypothesis
The aim of this study was to investigate the use of a generic and globally accessible instrument for assessing health-related quality of life (HR-QoL) in pelvic organ prolapse (POP) surgery.
Methods
In a prospective multicenter setting, 207 women underwent surgery for apical prolapse [stage ≥2, Pelvic Organ Prolapse Quantificcation (POP-Q) system] with or without anterior wall defect. Demographic and surgical characteristics were collected before surgery. Results of the 15-dimensional (15D) instrument and condition-specific pelvic floor symptoms as assessed using the Pelvic Floor Distress Inventory questionnaire (PFDI-20), including its subscales Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6), Colorectal–Anal Distress Inventory-8 (CRADI-8), and Urinary Distress Inventory-6 (UDI-6), were assessed preoperatively and 2 months and 1 year after surgery.
Results
HR-QoL as estimated by 15D was improved 1 year after surgery (p < 0.001). Prolapse-related 15D profile-index measures (excretion, discomfort, sexual activity, distress, and mobility) were significantly improved after surgery (p < 0.05–0.001). Significant inverse associations were detected between increased 15D scores and a decrease in PFDI-20 and subscale scores (p < 0.001), indicating improvements on both instruments.
Conclusions
Generic HR-QoL as estimated by 15D improved significantly after apical POP surgery and correlated with improvements of condition-specific outcome measures. These results suggest that a comprehensive evaluation of global HR-QoL is valid in assessing pelvic reconstructive surgery and may provide novel and important insights into previously understudied areas, such as cost–utility and cost-effectiveness analysis after urogynecological surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Health-related quality of life (HR-QoL) is widely recognized as an important outcome measure following urogynecological surgery [1]. For this purpose, several validated condition-specific questionnaires were developed [2,3,4] to reflect changes related to the condition of the disease being studied, but often, they do not indicate how an intervention has influenced general QoL. Furthermore, condition-specific assessments of postoperative QoL do not allow comparison with other surgical fields and make comparison of the effects of surgery across surgical disciplines impossible. For that reason, a generic and global QoL measurement is valuable.
The 15-dimensional (15D) instrument is a generic, comprehensive, self-administered, preference-based questionnaire used as a single and profile-index score measure [5,6,7,8,9,10]. Many studies in different surgical fields have investigated HR-QoL after surgery using the 15D [7,8,9,10,11,12,13,14]. For pelvic reconstructive surgery, however, most attention has been placed on condition-specific assessments of QoL with little focus on a generic and global QoL measure in relation to surgery. Use of the 15D may provide novel and important insights into previously understudied areas, such as cost–utility and cost-effectiveness analyses, in urogynecological surgery. The aim of this study was to investigate how changes in condition-specific QoL domains relate to changes in generic and global 15D when evaluating reconstructive surgery for apical prolapse.
Materials and methods
Study design
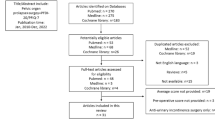
We used prospectively collected data from a multicenter study performed throughout 24 centers in Sweden, Finland, Denmark, and Norway of 207 patients operated for apical prolapse (POP-Q stage ≥2) with or without anterior wall defect [15]. All patients were operated on by a standard procedure using the Uphold™ Lite Vaginal Support System, and all surgeons received pretrial, hands-on training. The study was approved by The Stockholm Regional Board of Ethics at Karolinska Institutet, Stockholm, Sweden and ethic review committees in the participating countries. Patients were screened at baseline for apical (uterine or vaginal vault) prolapse stage II with or without concomitant anterior or vaginal wall prolapse stage ≥ 2 according to the Pelvic Organ Prolapse Quantification (POP-Q) system [16]. A standardized procedure using the Uphold™ vaginal support system was used in all patients, as previously described [15, 17, 18]. In short, a capturing device was used to place a monofilament macroporous and uncoated polypropylene mesh to suspend the apical vaginal segment. Clinical follow-up was performed at 2 months (n = 172, 83%) and 1 year (n = 164, 79%) after surgery.
Outcome measures
At baseline, demographic data was collected, and patients completed the Pelvic Floor Distress Inventory (PFDI-20) that comprises 20 items with three subscales: the Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6), the Colorectal–Anal Distress Inventory-8 (CRADI-8), and the Urinary Distress Inventory-6 (UDI-6). Each Inventory is scored from 0 to 100, and total PFDI-20 score (0–300) is gained by summation of all subscales [3, 19]. Postoperatively, the PFDI-20 was assessed at the 2-months and 1-year follow-up visit.
The 15D comprises mobility, vision, hearing, breathing, sleeping, eating, speech (communication), excretion, usual activity, mental function, discomfort, depression, distress, vitality, and sexual function [5, 6]. Each dimension has five descriptive levels to choose from. The 15D can be used as a profile and a single-index score measure. The valuation system is based on the application of multiattribute utility theory. The single index or utility score represents the generic HR-QoL with a maximum value of 1 (full health) to lower bound of 0 (dead). It also reports scores separately for each dimension to identify where changes in QoL take place [5, 6, 20]. The generic minimal important change (MIC) of ±0.015 in the 15D score, if statistically significant, was considered as the generic MIC threshold for improvement or deterioration in HR-QoL [21]. The quality-adjusted life-year (QALY) was evaluated using estimated 15D values preoperatively and at 2 months and 1 year after surgery [22].
Statistical analysis
We used the 15D score as a profile-index measure of HR-QoL. Five of the 15 dimensions were considered relevant for POP, including excretion, discomfort, sexual activity, distress, and mobility. Levels of 15D as a profile- or single-index measure were estimated preoperatively, 2 months, and 1 year after surgery. Statistical analyses were conducted using the predictive analysis software (PASW) (IBM@SPSS© Statistics, Version 22, Inc., Chicago, IL, USA). A p value <0.05 was considered statistically significant. Changes in 15D and PFDI-20 and its subscales over the study period were analyzed using one-way analysis of variance (ANOVA) for repeated measures. Unadjusted and adjusted models were used to test the correlation between preoperative and surgical characteristics with changes in 15D and PFDI-20 over time using analysis of covariance (ANCOVA) as a general linear model, which blends ANOVA and regression, as were comparisons between changes in 15D and PFDI-20 and subscales. Student’s t test was used for statistically significant differences between data before and one year after surgery. Cronbach’s coefficient alpha test was used to validate the reliability of the 15D for QoL measurement [23], with values of >0.7 considered as satisfactory [23]. There was no imputation of missing data. The study was registered at www.clinicaltrials.gov: NCT01823055.
Results
Complete information on the 15D and PFDI-20 was provided by 205/207 (99%) of patients preoperatively, 188/ 207 (91%) at 2 months, and 169/207 (82%) at 1 year. The 15D single-index score, used to measure HR-QoL, was significantly improved when its total preoperative score (0.888 ± 0.104) was compared with that 1 year after surgery (0.915 ± 0.081; p < 0.001). Thus, the generic MIC was +0.027, indicating significant improvement in HR-QoL. Cronbach’s coefficient alpha was used to test the reliability of 15D instrument and values were 0.81 preoperatively and 0.7 2 months and 0.82 1 year postoperatively and were considered satisfactory. Using ANOVA for repeated measurements, we analyzed 15D changes over time (Table 1 and Fig. 1). The single-index score was 0.888 ± 0.104 preoperatively, and 0.903 ± 0.108 2 months and 0.915 ± 0.081 1 year after surgery and was significantly improved (p = 0.029).
Seven of the 15D profile-index score measures were significantly improved p < 0.05–< 0.001 (Table 1) and those related to POP symptoms (mobility, excretion, discomfort, distress, and sexual activity) were significantly improved (p = 0.022 –< 0.001) between baseline and 1 year after surgery; two other dimensions (depression and sleeping) were also significantly improved (p = 0.037 and p = 0.018, respectively); all changes in descriptive dimensions are shown in Fig. 1. QALY measured using single-index score values before and up to 1 year after surgery was estimated as 0.97 of 1, indicating good health status. The increase in the single-index score after surgery suggested an improved global QoL (p = 0.029 ANOVA for repeated measures; Tables 1 and 2); similarly, PFDI-20 and subscale scores decreased (improved) significantly (p < 0.001) over time (Table 2). These changes indicate simultaneous improvements in global HR-QoL and pelvic organ function. We did multivariate regression analysis by ANCOVA to compare changes in 15D vs PFDI-20 and subscale scores to determine the association between the two instruments (Table 2). Results indicate an inverse correlation between changes in 15D single-index score compared with changes in PFDI-20 and subscales over time: decreased PFDI-20 scores consistently paralleled increased 15D scores: p < 0.001, ANCOVA (Table 2 and Fig. 2).
Increase of 15-dimensional (15D) instrument single-index score (improvement in quality of life) and drop in Pelvic Floor Distress Index-20 (PFDI-20) and subscales (POPDI-6 Pelvic Organ Prolapse Distress Inventory-6, CRADI-8 Colorectal–Anal Distress Inventory-8, UDI-6 Urinary Distress Inventory-6) at follow-up indicating improvement in condition-specific outcomes (% of total points for each scale)
Patient characteristics and surgical data were statistically tested against changes in 15D and PFDI-20 and subscales over time to investigate whether there was a correlation with improvement in generic HR-QoL and pelvic organ function (Table 3). Hysterectomy prior to prolapse reconstructive surgery and shorter hospital stay (≤ 1 day) were the only variables showing a significant correlation to improved 15D single-index score (p < 0.05).
We also investigated whether patient characteristics or surgical data were correlated with 15D profile-index scores. Seven of 15 dimensions—mobility, excretion, discomfort, distress, sexual activity, depression, and sleeping—improved over time after reconstructive surgery for apical POP. A higher level of education was correlated with improved 15D profile-index score for sleeping (p = 0.018), and sexual activity was significantly improved in patients with lower levels of physical training (p = 0.017). There were no other significant associations between preoperative patient characteristics or surgical data and any 15D profile-index score changes.
Discussion
In this prospective multicenter study, we found that generic HR-QoL (as estimated by the 15D instrument) improved significantly after apical POP reconstructive surgery. More importantly, improvements in condition-specific questionnaires were associated with corresponding improvements on the 15D. Furthermore, the estimated QALY (1-year measurement) indicates a good health status and corroborates the condition-specific outcome measures. These results suggest that a comprehensive evaluation of generic HR-QoL is valid in assessing pelvic reconstructive surgery and may provide novel and important insights into previously understudied areas of urogynecological surgery.
The 15D instrument has been widely used to investigate HR-QoL in several medical specialties [5,6,7,8,9,10] but has been scarcely used in pelvic floor surgery. In this study, the estimated 15D mean generic MIC, as measured preoperatively and 1 year after surgery, was +0.027, indicating improvement in HR-QoL [21]. Using multivariate regression analysis by ANCOVA, we found that changes in the total PFDI-20 score were significantly correlated with changes in 15D scores. Similar significant correlations were detected when each subscale was tested against the 15D in a multivariate analysis. Thus, an increase in 15D single-index score is inversely correlated with decreased PFDI-20 scores (total and subscales) after surgery: i.e., a parallel improvement in both instruments. Thus, our results suggest that postoperative improvements in condition-specific symptoms also improves global QoL and that the 15D reflects these changes.
Given its importance for preoperative counseling and goal setting, subjective and objective predictors of surgical outcomes have been the focus of investigation in number of surgical studies [5,6,7,8,9,10,11, 24]. A worsened postoperative QoL is predicted after the age of 35 years in patients with ulcerative colitis and ileal pouch/anal anastomosis [11]. After surgery for nonfunctioning pituitary adenomas (NFPAs), age, body mass index (BMI), depression, and diabetes are independent predictors of impaired overall HR-QoL [24]. Postural instability, high BMI, and worse baseline motor scores are the greatest predictors of poor functional and HR-QoL outcomes after deep brain stimulation surgery in Parkinson’s disease patients [10]. In urogynecological surgery, several factors—such as smoking, previous hysterectomy, age, and BMI—have been shown to influence QoL-related outcomes [25,26,27]. However, these studies were related to condition-specific outcomes and have largely disregarded global effects on generic HR-QoL.
In search of possible predictors for improvements in generic HR-QoL and condition-specific symptoms, we investigated the association between preoperative and surgical characteristics and changes in the 15D and the PFDI-20. Having had a hysterectomy prior to apical prolapse reconstructive surgery and a shorter hospital stay (≤ 1 day) were significantly correlated with an improvement in the 15D single-index score over the short term. However, no other preoperative or surgery-related parameters were correlated with changes in 15D. Higher educational level was significantly correlated with improvements in total PFDI-20 score. This concurs with other studies showing that a higher educational level is associated with better HR-QoL [13]. On a related note, stoma education has been shown to improve QoL and reduce length of hospital stay in colorectal surgery [9]. How patient education relates to improved QoL after urogynecological surgery is unknown, but it is possible that patients with a higher educational level are more prone to independently seek and process information on postoperative outcomes.
Among the strengths of our study are its uniform surgical technique, validated outcome measures, multicenter setting, and prospective data collection. Satisfactory compliance during follow-up strengthens our results by minimizing selection and reporting bias. We recognize that an independent control group would have added valuable information to the interpretation of our results and, similarly, that a longer duration of follow-up would have provided important information.
To summarize, we found that improvements in condition-specific symptoms after apical POP surgery are associated with a corresponding improvement in generic HR-QoL. Use of the 15D instrument may provide additional information on subjective outcomes in the field of urogynecological surgery and further broaden the perspective on assessing subjective outcomes. In addition, the 15D instrument can be used for health economic studies to calculate QALYs [22], which is a generic measure of disease burden that, together with information on medical expenditures associated with an intervention, can be used for cost–utility and cost-effectiveness analyses. As such, the 15D may become a useful tool for decision making based on economic evaluations in urogynecological surgery of the future.
References
Barber MD, Maher C. Apical prolapse. Int Urogynecol J. 2013;24(11):1815–33.
Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA. Health-related quality of life measures for women with urinary incontinence: the incontinence impact questionnaire and the Urogenital distress inventory. Continence program in women (CPW) research group. Qual Life Res. 1994;3(5):291–306.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13.
Rogers RG, Kammerer-Doak D, Villarreal A, Coates K, Qualls C. A new instrument to measure sexual function in women with urinary incontinence or pelvic organ prolapse. Am J Obstet Gynecol. 2001;184(4):552–8.
Sintonen H. The 15-D measure of health related quality of life: reliability, validity and sensitivity of its health state descriptive system. 1994. ISSN 1038–9547. ISBN 1 875677 36 4.
Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med. 2001;33(5):328–36.
Vainiola T, Roine RP, Suojaranta-Ylinen R, Vento A, Sintonen H. Can factors related to mortality be used to predict the follow-up health-related quality of life (HRQoL) in cardiac surgery patients? Intensive Crit Care Nurs. 2013;29(6):337–43.
Loponen P, Luther M, Nissinen J, Wistbacka JO, Biancari F, Laurikka J, et al. EuroSCORE predicts health-related quality of life after coronary artery bypass grafting. Interact Cardiovasc Thorac Surg. 2008;7(4):564–8.
Forsmo HM, Pfeffer F, Rasdal A, Sintonen H, Körner H, Erichsen C. Pre- and postoperative stoma education and guidance within an enhanced recovery after surgery (ERAS) programme reduces length of hospital stay in colorectal surgery. Int J Surg. 2016;36(Pt A):121–6.
Abboud H, Genc G, Thompson NR, Oravivattanakul S, Alsallom F, Reyes D, et al. Predictors of functional and quality of life outcomes following deep brain stimulation surgery in Parkinson’s disease patients: disease, patient, and surgical factors. Park Dis. 2017;2017:5609163. https://doi.org/10.1155/2017/5609163.
Abolfotouh S, Rautio T, Klintrup K, Helavirta I, Mäkelä J. Predictors of quality-of-life after ileal pouch-anal anastomosis in patients with ulcerative colitis. Scand J Gastroenterol. 2017;52(10):1078–85.
Ryhänen EM, Heiskanen I, Sintonen H, Välimäki MJ, Roine RP, Schalin-Jäntti C. Health-related quality of life is impaired in primary hyperparathyroidism and significantly improves after surgery: a prospective study using the 15D instrument. Endocr Connect. 2015;4(3):179–86.
Torvinen S, Färkkilä N, Sintonen H, Saarto T, Roine RP, Taari K. Health-related quality of life in prostate cancer. Acta Oncol. 2013;52(6):1094–101.
Ortiz F, Aronen P, Koskinen PK, Malmström RK, Finne P, Honkanen EO, et al. Health-related quality of life after kidney transplantation: who benefits the most? Transpl Int. 2014;27(11):1143–51.
Altman D, Mikkola TS, Bek KM, Rahkola-Soisalo P, Gunnarsson J, Engh ME, et al. Pelvic organ prolapse repair using the uphold™ vaginal support system: a 1-year multicenter study. Int Urogynecol J. 2016;27(9):1337–45.
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Vu MK, Letko J, Jirschele K, Gafni-Kane A, Nguyen A, Du H, et al. Minimal mesh repair for apical and anterior prolapse: initial anatomical and subjective outcomes. Int Urogynecol J. 2012;23(12):1753–61.
Gutman RE, Rardin CR, Sokol ER, Matthews C, Park AJ, Iglesia CB, et al. Vaginal and laparoscopic mesh hysteropexy for uterovaginal prolapse: a parallel cohort study. Am J Obstet Gynecol. 2017;216(1):38.e1–38.e11.
Elmér C, Altman D, Engh ME, Axelsen S, Väyrynen T, Falconer C, et al. Trocar-guided transvaginal mesh repair of pelvic organ prolapse. Obstet Gynecol. 2009;113(1):117–26.
http://www.15d-instrument.net/15d/. The health-related quality of life (HRQoL) instrument. Copyright: 15D©/Harri Sintonen (www.15d-instrument.net).
Alanne S, Roine RP, Räsänen P, Vainiola T, Sintonen H. Estimating the minimum important change in the 15D scores. Qual Life Res. 2015;24(3):599–606.
Weinstein MC, Torrance G, McGuire A. QALYs: the basics. Value Health. 2009;12(1):5–9.
Dagklis IE, Aletras VH, Tsantaki E, Orologas A, Niakas D. Multiple sclerosis patients valuing their own health status: valuation and psychometric properties of the 15D. Neurol Int. 2016;8(3):6416–28.
Karppinen A, Ritvonen E, Roine R, Sintonen H, Vehkavaara S, Kivipelto L, et al. Health-related quality of life in patients treated for nonfunctioning pituitary adenomas during the years 2000-2010. Clin Endocrinol. 2016;84(4):532–9.
Gagnon LH, Tang S, Brennand E. Predictors of length of stay after urogynecological surgery at a tertiary referral center. Int Urogynecol J. 2017;28(2):267–73.
Gerten KA, Markland AD, Lloyd LK, Richter HE. Prolapse and incontinence surgery in older women. J Urol. 2008;179(6):2111–8.
Ulrich D, Bjelic-Radisic V, Grabner K, Avian A, Trutnovsky G, Tamussino K, et al. Objective outcome and quality-of-life assessment in women with repeat incontinence surgery. Neurourol Urodyn. 2017;36(6):1543–9.
Funding
The study was supported by an investigator-initiated grant from Boston Scientific, grants from the Finnish Medical Foundation, and the Swedish Research Council.
Statistical analysis was performed in collaboration with statistician Fredrik Johansson, M.Sc, Department of Clinical Sciences, Medical Library, Karolinska Institutet Danderyd Hospital, Stockholm, Sweden.
The multicenter study was supported by an investigator-initiated grant from Boston Scientific, grants from the Finnish Medical Foundation, and the Swedish Research Council.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Stockholm Regional Ethical Review Board of Ethics at Karolinska Institutet, Stockholm, Sweden, and ethic review committees in the participating countries as appropriate.
Conflicts of interest
E. Morcos reports no conflicts of interest. K. Geale provides consulting services as an employee of Quantify Research, although this work was done independently. D. Altman has received speaking and advisory honoraria from Gedeon Richter, Pfizer, Astellas, Invent Medic, and Gynecare. C. Falconer has received speaking and advisory honoraria from Boston Scientific and Johnson & Johnson.
Rights and permissions
About this article
Cite this article
Altman, D., Geale, K., Falconer, C. et al. A generic health-related quality of life instrument for assessing pelvic organ prolapse surgery: correlation with condition-specific outcome measures. Int Urogynecol J 29, 1093–1099 (2018). https://doi.org/10.1007/s00192-018-3587-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3587-5