Abstract
Introduction and hypothesis
The aim of the study was to assess the effectiveness of repeat mid-urethral sling after a failed primary sling for stress urinary incontinence.
Methods
A total of 112 women with recurrent stress incontinence after primary mid-urethral sling underwent a repeat procedure between 2000 and 2011. All patients had a preoperative clinical and urodynamic evaluation. Outcomes were divided into three groups: cured (no more leaks), improved (decrease of leaks), or failed.
Results
All patients had urethral hypermobility and 12.9 % had intrinsic sphincter deficiency [maximum urethral closure pressure (MUCP) ≤ 20 cmH2O]. Median MUCP was 41 cmH20. Overactive bladder was found in 5.7 % of women. The second sling placed was one of the following: retropubic Tension-free Vaginal Tape (49 %), transobturator tape (48 %), or mini-sling (3 %). No intraoperative morbidity was reported. After the second sling was placed, 68 (60.7 %) patients were subjectively cured and 18 (16.1 %) improved (76.8 % success overall) with a mean follow-up of 21 months. Success rates were 72.2 and 81.8 % for transobturator and retropubic slings, respectively, with no significant difference. Multivariable analysis showed higher odds of cure and improvement with the retropubic approach after adjusting for MUCP. Late complication rates were comparable to those observed after a first sling. Urodynamic parameters were not associated with postoperative success.
Conclusions
Repeat mid-urethral sling for recurrent female stress urinary incontinence is nearly 77 % successful in a group of patients with persistent urethral hypermobility. A retropubic approach might be preferred for patients with low urethral closure pressures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 1996 Ulmsten et al. (Tension-free Vaginal Tape®, TVT) [1] and in 2001 Delorme (Transobturator Tape®, TOT) [2] developed the concept of mid-urethral support based on the hammock hypothesis proposed by DeLancey [3]. Mid-urethral slings (MUS) drastically changed stress urinary incontinence (SUI) surgery in the mid-1990s, with excellent outcomes and a mini-invasive approach.
Although MUS are the reference treatment of SUI due to their high success rates, 5–20 % of women still experience surgery failure [4]. Several options have been proposed: second MUS, tape shortening, bulking agents, Adjustable Continence Therapy®, and artificial urinary sphincter. To date, there is no consensus on the management of MUS failure. Repeat sling might be an appropriate solution for women showing persistent urethral hypermobility but few studies have demonstrated their effectiveness. The aim of this study was to determine the outcomes of a repeat MUS after a failed primary sling for SUI and if there are any differences in outcome with respect to MUS used.
Materials and methods
Study population
We retrospectively included 112 female patients who received a second sling for recurrent SUI. Patients were operated on in two university hospitals based in Paris (Bichat and Tenon) between 2000 and 2011. Inclusion criteria were failure or recurrence after a first MUS and urethral hypermobility (visually determined by physical examination). Any type of MUS was allowed for the first procedure.
Data for this study were obtained from usual procedures. Biological material and clinical measures were obtained only for standard diagnosis following physicians’ orders (no specific sampling, no modification of the sampling protocol, no supplementary question to the national standardized questionnaire). Data analyses were carried out using an anonymized database. According to the French Law of Public Health (CSP Art L 1121–1.1), such a protocol is exempt from written informed consent.
Evaluation
Preoperative assessment consisted of complete medical history, evaluation of lower urinary tract symptoms, physical examination, and urodynamic evaluation. Intrinsic sphincter deficiency was defined as maximum urethral closure pressure (MUCP) of 20 cmH2O or less. In 24 cases (21.4 %) urodynamic evaluation had been performed outside of the hospital and was summarized in medical records but was not available for statistical analyses.
Patients were postoperatively scheduled for evaluation by their surgeon including interview and physical examination at 1 month, 6 months, and 1 year or more. Patients who did not attend the clinic after 6 months were contacted for a phone interview. They were submitted to a structured questionnaire based upon the Urinary Symptom Profile® [5] and the International Consultation on Incontinence Questionnaire Short Form® (ICIQ-SF) question 3 [6], evaluating stress, urge, frequency, obstructive symptoms, and quality of life. Patients who attended the clinic once within 6 months but could not be contacted afterwards were considered as lost to follow-up.
During follow-up, patients were then classified into three independent groups: (1) subjective cure, defined by the absence of leaks within the last month; (2) improvement, defined as the decrease in number of leaks and better quality of life; or (3) failure. Overall success was defined by the combination of cure and improvement.
Methods, definitions, and units conform to the standards jointly recommended by the International Urogynecological Association (IUGA) and the International Continence Society (ICS) [7, 8].
Statistical analysis
Baseline characteristics were summarized by means (SD) for continuous variables or counts (%) for discrete variables and then compared across MUS types using a Kruskal–Wallis, Pearson χ2, or Fisher’s exact test. Analysis of urodynamic findings was performed on patients whose data was available. Using either success (cure and improvement) or cure after surgery as an endpoint, a multiple logistic regression model was used to estimate odds ratios (OR) between MUS types, while adjusting for MUCP. To address the question of whether any bias was introduced due to patients with short-term follow-up, we performed sensitivity analyses examining the distribution of endpoints while only including patients with information for a minimum of 6, 12, and 24 months after intervention. Additionally, discrete follow-up time was also included in the multiple logistic regression model. All analyses were performed using Stata (v11.0, StataCorp, College Station, TX, USA) and p < 0.05 was considered significant.
Results
Description of the study population
Clinical and urodynamic preoperative characteristics are displayed in Table 1 and show typical values for this type of population. The previous sling was not removed except for 33 patients in whom it was removed or cut due to vaginal or urethral mesh exposure (20), voiding dysfunction (10), or de novo urgency (3).
The second MUS was one of the following: retropubic tape (49 %), transobturator tape (48 %), or a single-incision mini-sling (3 %). The sling type was chosen according to the surgeon’s preference. Among the 12.9 % of patients with sphincter deficiency, there was 67 % of retropubic tapes, 25 % of transobturator tapes, and 8 % of mini-slings. Details pertaining to the initial and second sling types are given in Table 2.
The population was divided in two groups: retropubic slings (n = 54) and transobturator slings (n = 55). There was no significant difference between retropubic and transobturator groups, except for proportion of patients with hysterectomy (22.9 vs 42.2 %, respectively, p = 0.047) and detrusor overactivity (0 vs 11.4 %, respectively, p = 0.03).
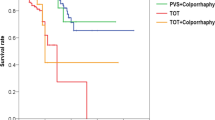
Clinical outcomes during follow-up
The mean follow-up was 21 months (median 12 months, range 1–108 months), with a total of 25 patients (22.4 %) lost to follow-up. In the entire study population, subjective cure rate was 60.7 % and improvement rate was 16.1 %, indicating an overall success of 76.8 %. Among the 20 patients with vaginal or urethral mesh exposure, 17 were cured (85 %), none was improved, and 3 had a second sling failure (15 %). We found that clinical and urodynamic preoperative parameters had no effect on the outcomes in both uni- and multivariable analyses nor did the etiology of failure or the sequence in which the slings were placed (Table 3).
Table 4 displays results for patients whose follow-up was greater than or equal to 6, 12, and 24 months, showing that long-term outcomes could be typically established after the first 6 months following surgery.
The cure and overall success rates were 65.4 and 81.8 % in the retropubic group and 57.4 and 72.2 % in the transobturator group, respectively. No significant difference was found between groups (p = 0.5 and p = 0.2, respectively). However, after adjustment for MUCP, patients having a retropubic approach had a 3.02-fold higher odds of cure (p = 0.05) and a 2.86-fold higher odds of overall success (p = 0.02) compared to the transobturator approach (Table 5). When additionally adjusting for follow-up time, the magnitude of effect remained the same for both cure (OR = 2.72, p = 0.046) or overall success (OR = 2.81, p = 0.06).
Complications associated with operation
There was no reported intraoperative morbidity, especially no bladder perforation or urethral injury. Postoperative complications were as follows: 8.9 % de novo urgency (2.7 % with urgency incontinence), 7.1 % temporary voiding dysfunction (successfully treated with clean intermittent catheterization), 3.6 % pelvic pain, and 2.7 % recurrent urinary tract infections. Five patients (4.5 %) had their sling removed because of three vaginal mesh exposures (2.7 %, none of them had vaginal or urethral mesh exposure after the first sling) and two complete retentions (1.8 %, 1 TOT, 1 TVT). None of the sling types were associated with an increased risk of complications.
Discussion
Currently, MUS are the preferred first-line treatment for female SUI. High cure rates over long periods are a clearly attainable goal, with one prospective evaluation reporting 90 % after 11 years [9]. Nevertheless, there remains 5 to up to 20 % risk of failure depending on the study population. Women with recurrent SUI who still have urethral hypermobility could technically benefit from a second MUS. We report that 76.8 % of patients have a successful second SUI, with the large majority completely resolving SUI. Furthermore, outcomes were typically determined within the first 6 months after surgery and were stable over time. To the best of our knowledge, this study represents the largest number of patients with repeat slings to date.
A literature review of studies since 2007 identified only seven case series of repeat MUS in which more than ten patients were included (Table 6). In three of seven studies, there was a heterogeneous distribution of first and second slings. Cure rates largely varied from 40 to 91.7 % with a weighted average of 64.9 %, while overall success rates similarly varied from 58 to 91.7 % with a weighted average of 76.6 %. In one of the more well-designed, prospective studies, a much higher cure rate (74 %) was reported among 31 women with 18 months of follow-up [10]. Unfortunately, their data can only be extended to a specific population, as numerous exclusion criteria [body mass index (BMI) > 30 kg/m2, associated urge incontinence or voiding dysfunction, concomitant pelvic floor surgery] arguably led to a population at low-risk of failure. With a subjective cure at 60.7 % and overall success at 76.8 %, our findings are similar to what has been previously described in the literature despite the aforementioned discrepancies. Our study comprising 112 patients is the largest performed on repeat sling outcomes to date.
In our cohort, no clinical or urodynamic parameter was correlated to surgical outcomes. Currently, few studies have included multivariable analysis in which other factors predictive of sling success or failure were observed. Nonetheless, it should be noted that several factors have been previously identified for first sling failure (age, previous incontinence surgery, urge incontinence, BMI > 25 kg/m2, diabetes, intrinsic sphincter deficiency, overactive bladder [11]).
A large number of studies have compared transobturator and retropubic slings. In a recent meta-analysis, TVT appeared to be followed by significantly higher rates of objective continence rates than TOT, with no difference in subjective continence rates [12]. On the contrary, more intraoperative complications and storage lower urinary tract symptoms were observed with TVT than TOT slings. Studies on repeat slings have also aimed to compare the two approaches. Lee et al. found a trend toward higher success for the retropubic approach, although the difference between the two groups was not statistically significant [13]. Only Stav et al. demonstrated a significant difference in favor of the retropubic approach (71 vs 48 %, p = 0.04) [14]. In our cohort there was no significant unadjusted difference between the two groups. On the other hand, after adjusting for closure pressure, retropubic slings were significantly superior to the transobturator approach: the retropubic approach increased in effectiveness as the MUCP decreased. Several studies have already shown that retropubic slings are more effective in woman with intrinsic sphincter deficiency [15, 16]. A possible explanation is the U-shape of the retropubic tape, which may be more supportive and obstructive than the horizontal orientation of the transobturator tape.
One limitation of our study is its retrospective design, considering that prospective randomized controlled trials are difficult to perform for second-line surgery. Tenon and Bichat hospitals represent two reference centers for urogynecology in France, with similar and well-standardized methods of perioperative evaluation and operative procedures. Nonetheless, 21.4 % of patients had missing urodynamic data.
Nineteen patients had missing data on MUCP. It could be argued that significance after adjustment for this factor was more likely due to selection of the patient subpopulation. We performed a sensitivity analysis in which crude OR were calculated among those with MUCP data and found no substantial difference in either the magnitude of effect or significance.
Another limitation is the use of numerous types of slings. Hence, several different kinds of materials were compared (allowing the comparison of retropubic and transobturator approaches). Some have been withdrawn from the market due to their increased risk in vaginal or urethral mesh exposures, fistulas, or cellulitis (ObTape®, Uratape®, IVS®, etc.). Currently, the only recommended type of sling is nonwoven polypropylene.
Despite a 22.4 % loss to follow-up, results were very stable regardless of minimal amount of follow-up time. We can therefore suppose that the outcomes of patients with less than 6, 12, or even 24 months of information would not have significantly altered the results of our study.
Conclusion
With 77 % overall success and low risk of complications, repeat slings are still a worthwhile therapeutic alternative in patients whose symptom is a social handicap. Moreover, we found that retropubic slings are more efficient than transobturator slings after adjusting for low MUCP. These data can be useful when choosing the approach after failure. However, the success of repeat slings is inferior to a first procedure.
Patients requiring a repeat sling should be carefully selected. Tape failure brings to light a great variety of situations that require rigorous assessment. Notwithstanding its simplicity, clinicians should not be driven to repeat MUS automatically when other solutions may be more appropriate (bulking agents, Adjustable Continence Therapy®, artificial sphincter).
References
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7(2):81–85, discussion 85–86
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 11(6):1306–1313
DeLancey JO (1994) Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis. Am J Obstet Gynecol 170(6):1713–1720, discussion 1720–1723
Fong ED, Nitti VW (2010) Review article: Mid-urethral synthetic slings for female stress urinary incontinence. BJU Int 106(5):596–608
Haab F, Richard F, Amarenco G, Coloby P, Arnould B, Benmedjahed K, Guillemin I, Grise P (2008) Comprehensive evaluation of bladder and urethral dysfunction symptoms: development and psychometric validation of the Urinary Symptom Profile (USP) questionnaire. Urology 71(4):646–656
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P (2004) ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn 23(4):322–330
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21(1):5–26
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, Dwyer PL, Fatton B, Kocjancic E, Lee J, Maher C, Petri E, Rizk DE, Sand PK, Schaer GN, Webb RJ (2011) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) & grafts in female pelvic floor surgery. Int Urogynecol J 22(1):3–15
Nilsson CG, Palva K, Rezapour M, Falconer C (2008) Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 19(8):1043–1047
Liapis A, Bakas P, Creatsas G (2009) Tension-free vaginal tape in the management of recurrent urodynamic stress incontinence after previous failed midurethral tape. Eur Urol 55(6):1450–1455
Stav K, Dwyer PL, Rosamilia A, Schierlitz L, Lim YN, Lee J (2010) Risk factors of treatment failure of midurethral sling procedures for women with urinary stress incontinence. Int Urogynecol J 21(2):149–155
Novara G, Artibani W, Barber MD, Chapple CR, Costantini E, Ficarra V, Hilton P, Nilsson CG, Waltregny D (2010) Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Eur Urol 58(2):218–238
Lee KS, Doo CK, Han DH, Jung BJ, Han JY, Choo MS (2007) Outcomes following repeat mid urethral synthetic sling after failure of the initial sling procedure: rediscovery of the tension-free vaginal tape procedure. J Urol 178(4 Pt 1):1370–1374
Stav K, Dwyer PL, Rosamilia A, Schierlitz L, Lim YN, Chao F, De Souza A, Thomas E, Murray C, Conway C, Lee J (2010) Repeat synthetic mid urethral sling procedure for women with recurrent stress urinary incontinence. J Urol 183(1):241–246
Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A, Lim YN, Hiscock R (2008) Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol 112(6):1253–1261
Miller JJ, Botros SM, Akl MN, Aschkenazi SO, Beaumont JL, Goldberg RP, Sand PK (2006) Is transobturator tape as effective as tension-free vaginal tape in patients with borderline maximum urethral closure pressure? Am J Obstet Gynecol 195(6):1799–1804
Tsivian A, Neuman M, Yulish E, Shtricker A, Levin S, Cytron S, Sidi AA (2007) Redo midurethral synthetic sling for female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18(1):23–26
Eandi JA, Tanaka ST, Hellenthal NJ, O’Connor RC, Stone AR (2008) Self-reported urinary continence outcomes for repeat midurethral synthetic sling placement. Int Braz J Urol 34(3):336–342
Van Baelen AA, Delaere KP (2009) Repeat transobturator tape after failed mid-urethral sling procedure: follow-up with questionnaire-based assessment. Urol Int 83(4):399–403
Palva K, Nilsson CG (2009) Effectiveness of the TVT procedure as a repeat mid-urethra operation for treatment of stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 20(7):769–774
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meyer, F., Hermieu, J.F., Boyd, A. et al. Repeat mid-urethral sling for recurrent female stress urinary incontinence. Int Urogynecol J 24, 817–822 (2013). https://doi.org/10.1007/s00192-012-1941-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1941-6