Abstract
Introduction and hypothesis
This study aims to compare pre-operative Pelvic Organ Prolapse Quantification (POP-Q) point C with and without cervical traction to that obtained intra-operatively in women undergoing pelvic organ prolapse surgery and to assess acceptability of examination with cervical traction without anaesthesia.
Methods
Eighty-one women were randomised to having pre-operative examination with or without cervical traction to measure point C. Visual analogue scale (VAS) pain scores were recorded for each pre-operative examination. Comparisons were made between pre-operative and intra-operative findings.
Results
The mean difference between pre-operative and intra-operative point C in the non-traction group was statistically higher than in the traction group (3.2 vs 1.6 cm, p = 0.0001). The level of agreement between pre-operative point C measurement with traction and intra-operative point C measurement was better than pre-operative point C measurement without traction and intra-operative point C measurement on Bland and Altman plots. Women having cervical traction reported significantly greater pain score on the VAS (3.4 vs. 1.2, p < 0.0001).
Conclusions
Compared to routine pre-operative examination with Valsalva and cough manoeuvres only, pre-operative examination with cervical traction had better agreement with intra-operative point C findings. Although women reported greater pain score when examined with cervical traction, it was still a tolerable and acceptable examination without anaesthesia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) is a prevalent condition affecting millions of women worldwide. Whilst the often quoted lifetime risk of a woman undergoing at least one operation for POP or urinary incontinence (UI) is 11% by the age of 80 years [1], a more recent cross-sectional study [2] reported a lifetime risk of 19% for prolapse surgery in the general female population of Western Australia.
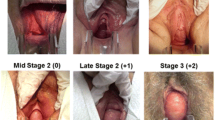
Currently, the POP-Q remains the most objective, site-specific system for quantifying and describing POP with proven intra-observer and inter-observer reliability and reproducibility [3, 4]. However, studies have shown that its reproducibility can be affected by different examination conditions and techniques, e.g. patient position, vaginal specula, retractors or tractors, type of straining and fullness of bladder and rectum [5]. Furthermore, there is evidence to suggest that intra-operative examination of prolapse under anaesthesia could be significantly different from pre-operative examination even if the POP-Q system is used [6–8]. Increase in uterine descent intra-operatively may be due to the absence of levator co-activation under anaesthesia, progression of the prolapse or not eliciting the maximal uterine descent at the time of initial examination.
It is our practice to perform a vaginal hysterectomy or uterine suspension as part of the POP surgery if the uterus descends to −1 cm or distal to the hymen with traction intra-operatively. Patients are counselled and informed that the definitive decision is only made after examination in theatre under anaesthesia.
Use of a speculum and vulsellum is already commonplace in outpatient gynaecology practice. Cervical traction to ascertain maximal uterine descent without anaesthesia pre-operatively may allow a more accurate pre-operative assessment.
The aims of this study are twofold—to determine if pre-operative examination with cervical traction improves agreement between pre-operative and intra-operative POP-Q point C measurements and to determine patient acceptability of examination with cervical traction without anaesthesia.
Materials and methods
This randomised prospective study, with ethical approval obtained from each centre, was performed at two urogynaecology units in Melbourne, Australia between June 2010 and March 2011 (ethical approval numbers R10/09 and 10048B). The study is registered with the Australian New Zealand Clinical Trials Registry—ACTRN12611000141943.
Patients presenting to both urogynaecology units for POP surgery (vaginal repair ± vaginal hysterectomy ± mesh suspension) with or without continence surgery between June 2010 and March 2011 were invited to participate in the study. Patients who had a hysterectomy were excluded. A total of 81 patients were recruited.
After consent was obtained, the patient was randomised into one of two groups—pre-operative assessment without traction (non-traction group) or pre-operative assessment with traction (traction group). Randomization with allocation concealment was performed using computer-generated blocks of four. The pre-operative and intra-operative examiners were randomly allocated, with the only stipulation being that the pre-operative and intra-operative examiners were different for each patient. This random allocation of examiners was planned to reduce potential bias and maintain heterogeneity in the degree of traction applied, albeit without standardised applied traction. All pre-operative and intra-operative measurements of POP-Q point C were made using either a uterine sound or ruler and recorded in centimetres. Point C was taken as the lowest point of cervical descent and measured in relation to the hymen as described in the POP-Q system.
Routine POP-Q examination in our unit involves digital vaginal examination and palpation (with the use of a Sims or one blade of a bivalve speculum), with the patient in the supine position either performing Valsalva manoeuvres or a series of coughs, to ascertain the maximal descent of each of the three compartments. Examination with cervical traction was performed with a bivalve speculum and vulsellum. The bivalve speculum aided in locating the cervix and application of the vulsellum to the anterior lip of the cervix. The vulsellum was closed to one ‘click’ only and the bivalve speculum closed and retracted gently with cervical traction. Patients were offered local anaesthetic spray on the cervix prior to application of the vulsellum. Pre-operative examinations in both groups were performed with the patients’ bladders relatively empty, i.e. no urge to void. All patients were given an opportunity to empty their bladders prior to an examination in the outpatients department and also prior to going to the anaesthetic room.
Pain scores using a 10-cm visual analogue scale (VAS) pain score with numerical rating scale were obtained for each of the pre-operative examinations. All patients had point C assessed under anaesthesia using a vulsellum and Sims speculum in lithotomy position prior to the commencement of the surgery by the allocated examiner. The bladder was not emptied prior to the intra-operative assessment of point C.
Pre-operative examinations in both groups of patients were performed in the anaesthetic room without pre-medication just prior to surgery except for nine patients randomised to the non-traction group. These nine patients had their pre-operative POP-Q examination performed at their outpatient consultation within 3 months of the scheduled surgery.
We used a mean VAS pain score of <5.0 as an acceptable or tolerable pain level. This is based on a study [9] investigating pain and acceptability in traditional outpatient hysteroscopy, which demonstrated a mean VAS pain score of 4.7 correlated with a mean acceptance score of 8.3. We used studies from traditional outpatient hysteroscopy as in this procedure; traction is also applied to the cervix with forceps.
This is a study of a continuous response variable from independent control and experimental subjects with one control per experimental subject. We assume that the difference between point C measurements with and without traction was normally distributed with standard deviation of 1. If the true difference in the experimental and control means is 1 cm, at a power of 80% and a significance level of 0.05, the sample size estimate was 17 subjects per group to reject the null hypothesis.
All data were entered into an excel spreadsheet and imported into STATA 9.2 (StataCorp., College Station, TX, USA) for analysis. To compare the means of continuous variables, t test was used and, for comparisons of proportions, Pearson’s chi-squared test was used. Bland and Altman plots were used to reflect the level of agreement between point C with and without cervical traction and intra-operative point C measurement.
Results
A total of 82 patients were invited to participate. One patient declined participation, leaving a total of 81 patients recruited during the study period. Progress of the participants is shown in the flowchart (Fig. 1).
Patient demographics (mean age, BMI and parity) are displayed in Table 1. There was no significant difference between the two groups.
One patient, randomised to the traction group, was unable to have examination with cervical traction because of vaginal burning from the local anaesthetic spray prior to the application of the vulsellum. Another patient randomised to the traction arm was unable to have the examination with traction, as the examiner was unable to visualise the cervix due to a large cystocele. Both these patients’ point C data sets were analysed as part of the non-traction group, and their VAS pain scores were excluded from analysis.
The mean difference in pre-operative and intra-operative point C measurement in the non-traction group was 3.2 cm (95% confidence interval [CI], 2.6–3.8). In the traction group, the mean difference in point C measurement obtained with cervical traction pre-operatively and intra-operatively was 1.6 cm (95% CI, 1.2–2.0). The difference between these two means is statistically significant, p = 0.0001 (Table 2).
Pre-operative and intra-operative point C measurements differed by 3 cm or more in 14% of 37 patient data sets in the traction group compared with 57% of 44 patient data sets in the non-traction group. This difference is highly statistically significant with p = 0.0001. Pre-operative cervical traction also resulted in a significantly greater proportion of patients having the same POP-Q point C measurement to that obtained intra-operatively (24% vs. 7%, p = 0.027). A significantly greater number of patients in the traction group had pre-operative point C measurements within 1–2 cm of that obtained intra-operatively (62% vs. 36%, p = 0.021) (Table 3).
Level of agreement between pre-operative and intra-operative point C measurements in the traction group was assessed with Bland and Altman plots (Fig. 2). The level of agreement between pre-operative point C measurement and intra-operative point C measurements was better in the traction group.
a Bland and Altman plot for pre-operative point C without traction and intra-operative point C. Solid red line mean difference in point C measured pre-operatively and intra-operatively, dashed red line 2 standard deviations of the mean. b Bland and Altman plot for pre-operative point C with traction and intra-operative point C. Solid red line mean difference in point C measured pre-operatively and intra-operatively, dashed red line 2 standard deviations of the mean
In the traction group, the mean VAS pain score without traction was 1.2 (95% CI, 0.7–1.7) and 3.4 (95% CI, 2.7–4.1) with traction. The difference in the mean pain scores was statistically significant, p < 0.0001. Of the 39 patients randomised to the traction arm, only one patient received local anaesthetic spray to the cervix prior to application of the vulsellum and had significant vaginal burning from the local anaesthetic spray with a VAS pain score of 10—examination with traction was not performed and her pain score excluded from analysis. Six and three patients reported VAS pain scores of 5 and above 5, respectively, with cervical traction.
Discussion
Our study found that pre-operative examination with cervical traction correlated substantially better and more accurately reflected point C measured under anaesthesia, arguably the maximal descent. The mean VAS pain score recorded in this study was 3 out of 10 where traction was used and 1 out of 10 in the non-traction group, significantly higher with traction but a low level of discomfort overall.
Loss of apical support is the most challenging compartment to assess prior to surgery. Several studies have examined the effects of confounders of pelvic organ descent measures using the POP-Q system. Silva et al. [10] and Visco et al. [11] reported that the maximal extent of prolapse is better demonstrated in the standing position. However, routine examination on standing may not be necessary if a good examination in dorsal lithotomy is performed [12], with the patient confirming the extent of her prolapse and is able to perform a forceful Valsalva.
Prolapse size differs depending on strength, duration and number of efforts of Valsalva. Tumbarello et al. [13] demonstrated that 40% of women have at least a 2-cm increase in prolapse size on dynamic MRI when the Valsalva is repeated three times in women who had been instructed on how to perform a proper Valsalva and who had demonstrated their ability to do so during pelvic examination. Orejuela et al. [14] reported that, in order to reach maximal organ descent, Valsalva had to be sustained for an average of 9 s. Orno and Dietz [15] demonstrated on ultrasound that the Valsalva manoeuvre is frequently accompanied by levator co-activation.
Gentle traction on the cervix using instruments that are readily available in most gynaecological outpatient departments to elicit the maximal uterine descent is a simple and inexpensive method of assessment of uterine descent. It eliminates patient position, ineffective Valsalva or levator co-activation as confounding factors of accurate examination of the degree of uterine prolapse.
The mean VAS pain score recorded in this study is significantly higher with examination using traction (3.4 vs. 1.2, p < 0.0001). However, the mean pain score recorded with traction was <5 and in the tolerable range reported by studies on traditional outpatient hysteroscopy.
One of the deficiencies in our study is that we did not standardise or measure the degree of traction applied at our examinations. Even though examiners were randomly allocated to reduce bias and maintain heterogeneity in the level of traction applied, they were not specifically blinded. This may have led to the larger difference between point C measured with traction pre-operatively and intra-operatively in our study, compared to 2.3 cm reported by Vierhout et al. [7].
Fullness of the bladder is another reported confounder of POP-Q measurements. We did not empty the patient’s bladder prior to pre-operative and intra-operative examinations as the study design is aimed to reflect our clinical practice. However, all patients were given an opportunity to empty their bladders prior to entering the anaesthetic room. Furthermore, a substantial number of our pre-operative and intra-operative assessments were performed very close together in timing in women who were fasting for theatre. We believe that bladder volume would not have been significantly different between examinations.
In conclusion, examination with cervical traction without anaesthesia pre-operatively is a simple and acceptable examination that may aid clinical assessment of uterine descent.
Abbreviations
- POP:
-
Pelvic organ prolapse
- UI:
-
Urinary incontinence
- POP-Q:
-
Pelvic Organ Prolapse Quantification
- CI:
-
Confidence interval
- VAS:
-
Visual analogue scale
- IUD:
-
Intrauterine device
References
Olsen AL, Smith V, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Smith FJ, Holman CDJ, Moorin RE, Tsokos N (2010) Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol 116(5):1096–1100
Hall AF, Theofrastous JP, Cundiff GW et al (1996) Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol 175:1467–1470, discussion 1470–1471
Kobak WH, Rosenberger K, Walters MD (1996) Interobserver variation in the assessment of pelvic organ prolapse. Int Urogynecol J 7:121–124
Digesu GA, Khullar V, Cardozo L, Robinson D (2008) Inter-observer reliability of digital examinations using a four-grade scale in different patient positions. Int Urogynecol J 19:1303–1307
Vineyard DD, Kuehl TJ, Coates KW, Shull BL (2002) A comparison of preoperative and intraoperative evaluations for patients who undergo site-specific operation for the correction of pelvic organ prolapse. Am J Obstet Gynecol 186:1155–1159
Vierhout ME, Stoutjesdijk J, Spruijt J (2005) A comparison of preoperative and intraoperative evaluation of patients undergoing pelvic reconstructive surgery for pelvic organ prolapse using the pelvic organ prolapse quantification system. Int Urogynecol J 17:46–49
Fayyad A, Hill S, Gurung V, Prashar S, Smonth ARB (2007) How accurate is symptomatic and clinical evaluation of prolapse prior to surgical repair? Int Urogynecol J 18:1179–1183
Lau WC, Ho RYF, Tsang MK, Yuen PM (1999) Patient’s acceptance of outpatient hysteroscopy. Gynecol Obstet Invest 47:191–193
Silva WA, Kleeman S, Segal J, Pauls R, Woods SE, Karram MM (2004) Effect of a full bladder and patient positioning on pelvic organ prolapse assessment. Obstet Gynecol 104:37–41
Visco AG, Wei JT, McClure LA, Handa VL, Nygaard IE (2003) Effect of examination technique modifications on pelvic organ prolapse quantification (POP-Q) results. Int Urogynaecol J 14:136–140
Swift SE, Herring M (1998) Comparison of pelvic organ prolapse in the dorsal lithotomy compared with the standing position. Obstet Gynecol 91:961–964
Tumbarello JA, Hsu Y, Lewicky-Gaupp C, Rohrer S, DeLancey JOL (2010) Do repetitive Valsalva maneuvers change maximum prolapse on dynamic MRI? Int Urogynecol J 21:1247–1251
Orejuela F, Shek KL, Dietz HP (2010) The time factor in the assessment of prolapse and levator ballooning. Int Urogynecol J 21:S365–S367
Orno AK, Dietz HP (2007) Levator co-activation is a significant confounder of pelvic organ descent on Valsalva maneuver. Ultrasound Obstet Gynecol 30:346–350
Acknowledgements
We would like to thank our colleagues Joseph Lee, Yik N. Lim, Frank Buchanan, Kok-Weng Chan, Alison DeSouza and Geoff Edwards who have contributed to the recruitment process, data analysis and manuscript editing.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chao, F.L., Rosamilia, A., Dwyer, P.L. et al. Does pre-operative traction on the cervix approximate intra-operative uterine prolapse? A randomised controlled trial. Int Urogynecol J 23, 417–422 (2012). https://doi.org/10.1007/s00192-011-1656-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1656-0