Abstract
Objective
The purpose of our study was to determine whether the anatomic threshold for pelvic organ prolapse (POP) diagnosis and surgical success remains valid when the patient sees what we see on exam.
Methods
Two hundred participants were assigned, by computer-generated block randomization, to see one of four videos. Each video contained the same six clips representative of various degrees of anterior vaginal wall support. Participants were asked questions immediately after each clip. They were asked: “In your opinion, does this patient have a bulge or something falling out that she can see or feel in the vaginal area?” Similarly, they were asked to give their opinion on surgical outcome on a 4-point Likert scale.
Results
The proportion of participants who identified the presence of a vaginal bulge increased substantially at the level of early stage 2 prolapse (1 cm above the hymen), with 67 % answering yes to the question regarding bulge. The proportion of participants who felt that surgical outcome was less desirable also increased substantially at early stage 2 prolapse (1 cm above the hymen), with 52 % describing that outcome as “not at all” or “somewhat” successful.
Conclusion
Early stage 2 POP (1 cm above the hymen) is the anatomic threshold at which women identify both a vaginal bulge and a less desirable surgical outcome when they see what we see on examination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) and surgical success after reconstructive surgery have evolved from a physician-centered to a patient-centered diagnosis based on clinical data from well-designed epidemiologic studies [1–4]. Two of the more commonly used classification systems—Baden-Walker halfway system [5] and the Pelvic Organ Quantification (POP-Q) system [6]—established “normalcy” as the absence of anatomical prolapse on physical examination by the health-care provider. The US National Institutes of Health (NIH) panel on standardization of terminology for POP followed these recommendations by defining surgical success as the absence of anatomical prolapse on physical examination as well [7]. Surgical failure was evident when the leading edge of the prolapse descended 1 cm above the hymen or beyond (stage ≥ 2). Yet 37 % of asymptomatic women (17 % hysterectomized, median parity two) have stage 2 prolapse, suggesting incredibly high disease prevalence if these anatomic definitions are considered valid [2]. However, physical examination of nulliparous women reveals vaginal descent no greater than 1.46 cm above the hymen (< stage 2 prolapse) [4], suggesting that pregnancy, multiparity, and hysterectomy may contribute to pelvic support defects in asymptomatic women, regardless of the definition of prolapse or surgical success after reconstructive surgery [8]. Nonetheless, vaginal symptoms, including the feeling of a vaginal bulge, are the most reliable symptom of POP when the leading edge descends to or beyond the hymen [9]. Health outcomes researcher in female pelvic medicine and reconstructive surgery have redefined POP using this symptomatic threshold [1–3] rather than the previously established anatomic one. This new symptomatic threshold was used to retrospectively reclassify previously published surgical outcomes following vaginal reconstructive surgery, resulting in an unprecedented improvement in success rates from 30 to 46 % to 88 % for the surgical team [10]. More recently, prospective studies have used a composite definition for surgical success (anatomic success with absence of symptoms or need for retreatment), creating two additional hurdles for the surgeon to clear, thereby reducing the probability for a successful health outcome even after the most durable repair [11].
Surgeons must reconcile what they see on pelvic examination after reconstructive surgery with what the patient feels, especially when there is descent to the hymen in an asymptomatic patient. A finding of stage 2 prolapse in an asymptomatic patient can lead to uncertainty for the surgeon and is partially based on a lack of knowledge about the clinical significance, natural history, or progression of disease in this population. Knowledge regarding patient perspective of this problem is warranted, especially during the transition from a service-based to a health-outcomes-based payment system, so reconstructive surgeons can provide guidance when legislative decisions are made.
We were interested in gaining the patient’s perspective on a threshold for defining POP and success/failure after reconstructive surgery “if they could see what we see” on physical examination.
Materials and methods
We conducted a prospective, cross-sectional study of all eligible women presenting for a new-patient visit to our tertiary urogynecology referral center for care of any pelvic floor disorder. Women who declined participation, who were unable to consent for participation, or who were unable to complete study questionnaires in English were excluded. A convenience sample was approached, and informed consent was obtained, between August 2013 and August 2014. Study participation was completed prior to medical counseling to eliminate any possibility of information bias. This study was fully approved by the Institutional Review Board at Indiana University.
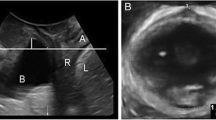
Participants were then assigned, by computerized block randomization, to see one of four videos. Each video contained the same six dynamic clips representative of various degrees of anterior vaginal wall support with Valsalva maneuver in the supine position. The order of clips was similarly randomized on the four videos. This double randomization was performed to minimize potential response bias introduced if prolapse stage was displayed by increasing or decreasing severity. The six clips represented stage 0, stage 1, early stage 2 (leading edge 1 cm above the hymen), mid stage 2 (leading edge at the hymen), late stage 2 (leading edge 1 cm below the hymen), and stage 3 POP using the POP-Q staging system [6]. In light of the previously described importance of the hymen as a reference point for treatment success and failure, stage 2 POP was subdivided into varying degrees because it includes points of descent above and below the hymen. Figure 1 includes still pictures taken directly from the dynamic videos participants were asked to view. These images show the vaginal introitus with the posterior blade of a Grave’s speculum compressing the posterior wall of the vagina and represent the maximal degree of descent of the anterior wall seen with Valsalva maneuver in the supine position.
Immediately after viewing each clip, participants were prompted to answer three questions. They were first asked to give a Yes or No response to the following question: “In your opinion, does this patient have a bulge or something falling out that she can see or feel in the vaginal area?” This question was adapted from question 3 of the POP Distress Inventory (POP-DI) subdomain of the validated Pelvic Floor Distress Inventory (PFDI-20) short form [12, 13]. Women were then asked to rate the certainty of their response on a 10-point visual analog scale (VAS), where 0 represented absolutely uncertain and 10 represented absolutely certain. This was ultimately converted to percentage certainty. Finally, participants were asked to give their opinion on surgical outcome on a 4-point Likert scale [11]. They were asked: “Assume this patient has previously had surgery to treat her vaginal bulge. In your opinion, has her surgery been very, moderately, somewhat or not at all successful.” Although no specific clinical context was provided to participants, all had bladder, vaginal, or bowel symptoms that warranted urogynecology referral, mimicking the experience of patients with a number of pelvic floor disorders who are presented with the PFDI-20 and Pelvic Floor Impact Questionnaire (PFIQ-7) prior to their subspecialty physician visit.
Additional demographic and clinical variables including age, race, chief complaint, and overall prolapse stage were then collected from the medical record. In addition, scores on two condition-specific validated questionnaires routinely administered in our office, the PFDI-20 and the PFIQ-7, were collected. Socioeconomic status (SES) was measured using the Hollingshead Four Factor Index [14], a composite index using three domains to measure socioeconomic status, including marital status, educational attainment, and occupation. The range on this scale is 8–66, with higher scores indicating higher SES. Finally, dispositional optimism was measured via the Life Orientation Test (LOT) [15]. This self-administered questionnaire was developed to assess individual differences in generalized optimism versus pessimism with LOT scores frequently used to assess the health consequences of this personality-variable trait. The range on this scale is 0–24, with higher scores indicating more dispositional optimism rather than pessimism.
Descriptive statistics were performed as appropriate for categorical and continuous variables based on histogram review. A Cochran’s Q test was performed to test the null hypothesis that there was no difference in K-related population proportions that identified a “symptomatic” vaginal bulge in each of the six video clips. Mann–Whitney U tests were performed to test the null hypothesis that a participant’s degree of response certainty about the presence or absence of a “symptomatic” vaginal bulge did not differ at each prolapse stage on the six video clips. Finally, a Cochran’s Q test was performed to test the null hypothesis that there was no difference in K-related population proportions that felt surgical outcome was less desirable in each of the six video clips. We dichotomized anatomic thresholds into two groups—(1) at or above the hymen, and (2) below the hymen—to determine when study participants first identified a “symptomatic” vaginal bulge. We dichotomized surgical outcome into two groups—(1) desirable (very and moderately successful), and (2) less desirable (somewhat and not at all successful)—to determine at what anatomic threshold our study participants first identified a less desirable surgical outcome. Bivariate analyses were performed to determine whether any baseline characteristics were predictive of a patient-centered anatomic threshold for defining a vaginal bulge or surgical success/failure either at and above or below the hymen. Statistical analysis was performed using SPSS v21.0 (IBM Corp, Armonk, NY, USA). P values of <0.05 were considered statistically significant.
Results
A total of 200 women were randomized during the study period, and 197 women completed the study questionnaires. Mean age of participants was 60 years [standard deviation (SD) 13.5], and the majority of participants were white (92 %). Forty-nine percent presented with a chief complaint of POP and 35 % with urinary incontinence or overactive bladder. The majority of women had never undergone prior incontinence or prolapse surgery (85 % and 86 %, respectively). The majority of women had stage ≤ 2 POP on physical examination (72 %). Mean SES score, as calculated from the Hollingshead Four Factor Index (scale 8–66), was 43 (SD 12), consistent with the social strata of medium-sized business owners, technical workers, and minor professionals. Mean LOT score, as calculated from the Life Orientation Test (scale 0–24), was 17 (SD 5), indicating moderate optimism. Briefly explained, our study participants tended to be more generally optimistic than pessimistic. Demographic and clinical characteristics are summarized in Table 1.
The proportion of participants who identified the presence of a symptomatic bulge increased substantially at the level of early stage 2 POP (1 cm above the hymen) (p < 0.001). After viewing the video clip representative of this stage of anterior vaginal wall support, 67 % of participants answered yes to the question: “In your opinion, does this patient have a bulge or something falling out that she can see or feel in the vaginal area?” This is a relatively sharp departure from responses to the same question after viewing the stage 1 POP clip, where only 38 % of participants responded affirmatively. Thus, 1 cm above the hymen seems to be the anatomic threshold at which women identified a vaginal bulge when they were allowed to see what we see on examination Fig. 2.
A graph of the degree of response certainty about the presence and absence of a bulge intersects at stage 1 prolapse where an equal level of uncertainty or “complete uncertainty” of participant responses exists. Immediately adjacent to stage 1 prolapse, there is a clear divergence of the two graphs, again supporting −1 cm above the hymen as the patient-centered anatomic threshold for “symptomatic” vaginal bulge identification when they can see what we see, in a statistically significant manner. The graphs do converge again, to a minor degree, at mid stage 2 POP (hymen). This could be related to factors other than the bulge affecting participant responses. It could also be related to the number of participants in the study and a lack of statistical power (Fig. 3).
The proportion of participants who felt that surgical outcome was less desirable also increased substantially at early stage 2 POP (1 cm above the hymen) (p < 0.001). Fifty-two percent of participants described the surgical outcome as “not at all successful” or “somewhat successful” (less desirable outcome) on a 4-point Likert scale after watching the video clip representative of this stage of anterior vaginal wall support. This is also a relatively sharp departure from the responses to the same question after viewing the stage 1 POP clip, where only 38 % of participants rated the surgical outcome as “not at all successful” or “somewhat successful”. Thus, 1 cm above the hymen may also be the anatomic threshold at which women identify surgical failure when they are allowed to see what we see on examination (Fig. 4).
Notably, 90 % of participants first identified symptomatic bulge as occurring at some level at or above the hymen after video viewing. Only 10 % felt that symptomatic bulge did not occur until the prolapse extended beyond the hymen. In addition, 84 % first identified a less desirable surgical outcome as prolapse occurring at some level at or above the hymen, while only 16 % felt that a less desirable surgical outcome did not occur until the prolapse extended beyond the hymen (Fig. 5). No single demographic or clinical characteristic predicted whether “symptomatic” vaginal bulge, or less desirable surgical outcome, was first identified with support at and above or below the hymen on bivariate analysis. This includes age, POP-Q stage on exam, and PFDI and PFIQ scores.
Discussion
Barber et al. recommended the use of patient perspective by including absence of bulge symptoms in any definition of surgical success after POP surgery, with the hymen as a reasonable threshold, until we have an understanding of the clinical significance of asymptomatic stage 2 disease [11]. However, the vaginal hymen is located in an inaccessible region for visual anatomic inspection and disease identification by the patient. The short-form PFDI-20 and PFIQ-7 are psychometrically valid, reliable, and responsive to change in women with pelvic floor disorders for assessment of symptom bother and impact on activities of daily living, respectively [12, 13]. Of the 41 questions that make up both questionnaires, only item 3 in the POP-DI subdomain of the PFDI-20 asks patients if they “usually have a bulge or something falling out that they can see or feel in the vaginal area.” Because the vagina is located in a less anatomically accessible region for visual inspection, a “yes” response to question 3 is highly correlated with self-identification of a vaginal bulge at or beyond the hymen—once the bulge can be seen. However, a “no” response should not rule out the existence of disease from the patient’s and provider’s perspective.
We purposely used the same wording from question 3 in the POP-DI subdomain of the PFDI-20 to gain patient perspective on a diagnosis of POP when “they saw what we saw” after video presentation. Similarly, we purposely used the same wording from the global impression of success scale to gain patient perspective on surgical success when “they saw what we saw” after video presentation [11]. In each case, we found that patients considered early (−1 cm) stage 2 disease clinically significant in their definition of POP and surgical success after reconstructive surgery. Anatomic thresholds of 1 cm above the hymen and “at or beyond the hymen” can coexist in the field of female pelvic medicine and reconstructive surgery. A diagnosis of POP based on a leading edge of −1 cm should not and would not require surgery, it would be “nonoperable,” until it descends beyond the hymen, when it becomes symptomatic and “operable.” To be clear, we do not advocate, nor do we feel that these findings support, surgical intervention on asymptomatic women with descent to −1 cm. Regardless, it appears that women, at least in the context of this study, identified descent to this level as less than ideal anatomical support.
We understand that this reasoning increases the percentage of “asymptomatic” women with disease from 3 % [16] to 37–69.8 % [4] based solely on an anatomic landmark. Yet this anatomic threshold (−1 cm) recognizes the contribution of pregnancy and vaginal delivery on pelvic support in multiparous women [2, 4]. Furthermore, we believe that this anatomic threshold does have utility for assessing surgical outcome after prolapse repair. Appraisal of surgical outcome continues to be the driving force for innovations in the field, including midurethral slings, ultra-light-weight macroporous mesh, biologic scaffolds and grafts, and minimally invasive approaches to abdominopelvic reconstructive surgeries.
There are several limitations to this study that must be considered before our conclusions can be accepted as valid. First, we did not establish the content validity or interobserver reliability of our video presentations for each POP-Q prolapse stage through consensus among experts in the field of female pelvic medicine and reconstructive surgery. In addition, we were unable to standardize the appearance of the video models’ external genitalia [age, body mass index (BMI), etc.] due to limitations of the available videos. However, the senior author, who has >20 years of experience in the field, established the content validity of our video presentations while we minimized systematic error through the randomization process. The clip sequence demonstrating POP-Q prolapse stage was randomly ordered in each of the four videos, which were randomly watched by study participants. Nonetheless, the results of our study may have differed if the videos containing clips of POP-Q prolapse stage were chosen by a panel of experts who were uninvolved in study design. Second, we provided limited clinical context for participants other than the study questions and the informed consent documents prior to video viewing. We purposely designed the study to mimic the experience of patients with a number of pelvic floor disorders who are presented with the PFDI-20 and PFIQ-7 prior to their subspecialty physician visit. Again, our study results may have differed if we limited study participation to women with POP who were presented with greater clinical context about their disorder prior to video viewing. Finally, our study was conducted with participants primarily affected by pelvic floor disorders and recruited from a urogynecology center. Thus, they may not be generalizable to women at large.
Study participants identified a leading edge descending 1-cm short of the hymen as the anatomic threshold for a “symptomatic” vaginal bulge suggestive of POP after seeing what we see on physical examination. We recommend consideration of the following possible definitions of POP and surgical success/failure: Nonoperable POP is a vaginal bulge in which the leading edge descends beyond 1 cm above the hymen with strain in the supine position in an asymptomatic patient. Operable POP is a vaginal bulge in which the leading edge descends beyond the hymen when symptoms are likely to occur. Study participants who characterize surgeries as unsuccessful when the leading edge of prolapse descends beyond 1 cm above the hymen validate providers’ feelings “when they see what we see on physical examination” because of our lack of knowledge about the natural history, or progression, of “asymptomatic” disease. Yet the provider and patient are likely willing to accept this degree of descent as nonoperable POP because it remains asymptomatic. While we accept the fact that the objective of reconstructive surgery is to relieve symptoms through bulge reduction, we are unwilling to characterize a surgical outcome as successful when in the eyes of both the patient and provider there is anatomic descent of the leading edge from −1 cm to the hymen on examination.
References
Swift SE, Tate SB, Nicholas J (2003) Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol 189:372–377
Swift S, Woodman P, O’Boyle A et al (2005) Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol 192:795–806
Tan JS, Lukacz ES, Menefee SA et al (2005) Predictive value of prolapse symptoms: a large database study. Int Urogynecol J Pelvic Floor Dysfunct 16:203–9
Trowbridge ER, Fultz NH, Patel DA et al (2008) Distribution of pelvic organ support measures in a population-based sample of middle-aged, community-dwelling African American and white women in southeastern Michigan. Am J Obstet Gynecol 198:548.e1–548.e6
Baden WF, Walker T (1992) Fundamentals, symptoms, and classification. In: Baden WF, Walker T (eds) Surgical repair of vaginal defects. JB Lippincott Company, Philadelphia, pp 9–23
Bump RC, Mattiasson A, Bo K, Brubaker LP et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–7
Weber AM, Abrams P, Brubaker L et al (2001) The standardization of terminology for researchers in female pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 12:178–86
Harris RL, Cundiff GW, Coates KW et al (1998) Urinary incontinence and pelvic organ prolapse in Nulliparous women. Obstet Gynecol 92(6):951–954
Barber M (2005) Symptoms and outcome measures of pelvic organ prolapse. Clin Obstet Gynecol 48(3):648–661
Chmielewski L, Walters MD, Weber AM, Barber MD (2011) Reanalysis of a randomized trial of 3 techniques of anterior colporrhaphy using clinically relevant definitions of success. Am J Obstet Gynecol 205:69.e1-8
Barber M, Brubaker I, Nygaard I et al (2009) Defining success after surgery for pelvic organ prolapse. Obstet Gynecol 114:600–9
Barber MD, Kuchibhatla MN, Pieper CF et al (2001) Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 185:1388–95
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition specific quality of life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193:103–113
Hollingshead AB (1975) Four-factor index of social status. Unpublished manuscript. Yale University, New Haven
Glaesmer H, Rief W, Martin A et al (2012) Psychometric properties and population-based norms of the Life Orientation Test Revised (LOT-R). Br J Health Psychol 17:432–445
Nygaard I, Barber M, Burgio K et al (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300(11):1311–1316
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None
Conflicts of interest
Dr. Hale is a consultant with Up to Date and President of AUGS. Dr. Sanchez is a consultant for Pelvalon. The remaining authors have no disclosures or conflicts of interest.
Rights and permissions
About this article
Cite this article
Kassis, N.C., Hamner, J.J., Takase-Sanchez, M.M. et al. If you could see what we see, would it bother you?. Int Urogynecol J 28, 59–64 (2017). https://doi.org/10.1007/s00192-016-3073-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3073-x