Abstract
This study aims to compare digital vaginal examination with the patient in supine and standing position and to correlate the degree of pelvic organ prolapse (POP) with a prolapse quality of life (P-QOL) questionnaire. Two hundred and seven women with POP symptoms were digitally examined in supine and standing positions using a four-grade scale (none, minimal, moderate, and severe). P-QOL was used to assess the severity of prolapse symptoms. Cohen’s kappa coefficient was used to calculate the inter-observer agreement and Spearman rank correlation test to assess the correlation between examination findings and P-QOL scores. Only vaginal examination findings in standing position had a good inter-observer reliability (kappa value 0.76–0.91). The severity of P-QOL scores only correlated with the examination findings in the standing position (P < 0.001). Digital examination of POP is unreliable if woman is supine but is reliable and correlates with symptoms and QOL impairment when the examination is performed with the patient standing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse is a major cause of morbidity in women and is a common problem affecting up to 30% of those attending gynaecology outpatient clinics [1, 2].
It has been estimated that 50% of parous women have some degree of prolapse [3], but only 20% of these are symptomatic and require surgical treatment [4].
A complete assessment of pelvic organ prolapse is important to plan appropriate surgery. Therefore, it is important that the examiner uses a reliable method to visualise and describe the maximum uterovaginal protrusion reported by women during their daily activities, to specify the position of the subject, the type of examination table and chair used, the type of vaginal specula, retractors or tractors used, the type of straining used to develop the prolapse maximally (e.g., Valsalva manoeuvre, cough), the fullness of the bladder and the contents of the rectum [5].
Many grading systems such as halfway system or Beecham classification and many different positions such as supine, lithotomy, lateral Sims’ position, erect sitting, and standing for vaginal examination have been described [6–8]. However, to our knowledge, the reliability of these examination systems in relation to the woman’s position has never been evaluated.
A standard system for describing the anatomic position of the pelvic organs has been described by the International Continence Society in 1996 [5]. Although the pelvic organ prolapse quantification (POP-Q) is the only standardised, reliable and universally accepted descriptive system [5, 10], it is rarely adopted in the clinical practice since clinicians are not always familiar or confident with this quantification method. ‘Lack of time in performing POP-Q’, ‘lack of training’, ‘complex system’, and ‘need of ruler’ are the commonest reasons limiting the use of this examination system.
Surprisingly, an international survey showed that up to 60% of International Continence Society (ICS) and American Urogynecology Society (AUGS) member do not routinely use the POP-Q in their clinical practice [10].
In many European hospitals, digital vaginal examination and a four-grade scale system are often used to assess pelvic organ prolapse [11]. Accordingly to this system, the prolapse is defined as minimal, moderate and severe or first, second and third degree if the leading edge of the prolapse is seen at the maximum valsalva to be above, at or below the introitus. Although this system is not widely referred to in the American literature [10], it is widely accepted and still adopted in Europe [11].
The position of a woman during digital vaginal examination in the assessment of the pelvic organ prolapse has also never been standardised. In fact, the only studies reported in the literature that have looked at the effect of a woman’s position on the assessment of pelvic organ prolapse used the POP-Q as a clinical examination tool [12, 13]. Nevertheless, the supine, lithotomy and lateral Sims’ position are the most commonly used.
Finally, although digital vaginal examination for the assessment of pelvic organ prolapse is widely used in European countries, to our knowledge there are no studies in the literature comparing digital vaginal examination using a four grade scale in various positions. Therefore, the aims of our study were to determine the inter-observer reliability of vaginal examination with a woman lying and standing and also to correlate the degree of prolapse with its effect on the disease-specific quality of life.
Materials and methods
Women with symptoms of pelvic organ prolapse referred to gynaecology outpatient clinics of two tertiary referral urogynaecology teaching hospitals were prospectively studied. All women were asked to complete the prolapse quality of life (P-QOL) questionnaire [14] to determine the severity of prolapse symptoms and their impact on quality of life.
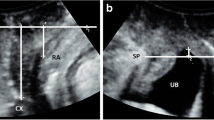
Each woman was examined digitally after voiding by two experienced clinicians separately, each blinded to the other’s findings, in the supine and standing positions. Digitally, the prolapse was defined as minimal, moderate or severe if the leading edge of the prolapse was felt at maximum Valsalva to be above, at or below the introitus [11]. If the woman was unable to perform a Valsalva manoeuvre, the pelvic organ prolapse was assessed asking the woman to cough.
No speculum was used during digital vaginal examination since this only involved the palpation with the index finger of the most caudal part of the leading edge of the vaginal wall or vault/cervix prolapse.
The inter-observer agreement was calculated using the Cohen’s kappa coefficient. Cohen’s kappa measures the agreement between the evaluations of two measurers when both are rating the same object. A value of 1 indicates perfect agreement. A value of 0 indicates that agreement is no better than chance. The strength of agreement is defined poor, fair, moderate, good and very good if the value of kappa is comprised between <0.20, 0.21–0.40, 0.41–0.60, 0.61–0.80, 0.81–1.00, respectively [16].
The different methods of vaginal examination were also correlated using the non-parametric Spearman rank correlation test with the prolapse quality of life domain scores. P values < 0.05 were reported as statistically significant. Statistical analysis was performed using SPSS version 14.0 (SPSS, Chicago USA). Each woman consented to participate in the study.
Results
Two hundred and seven women mean age 58 years (range 32–79 years) were studied between September 2000 and January 2002. The mean weight was 67 kg (range 45–105 kg). The median parity was 2 (ranges of 1–7).
The evaluations of anterior and posterior vaginal wall as well as the uterine/vaginal vault prolapse on standing are shown in Tables 1, 2 and 3.
When the women were examined digitally standing, the kappa value was 0.76 to 0.91, showing that this method has good repeatability.
The inter-observer reliability of the supine digital examinations was poor with a kappa value between 0.29–0.52.
The severity of PQOL scores strongly correlated only with the examination findings in the standing position (r = 0.7, P < 0.001) except for General Health Perceptions as shown in Table 4.
Discussion
Several methods have been proposed in the past for grading and describing disorders of pelvic floor support, but none has been rigidly standardised or validated to date [6–8]. In fact, Brubaker and Norton [16] in 1996 reviewed the English medical literature reported that ‘the clinical nomenclature used to describe the pelvic support defects is not standardised, and such a lack of standardisation limits the communication and advancement of knowledge regarding these common clinical problems’.
Therefore, in 1996, the International Continence Society, the Society of Gynecologic Surgeons and the American Urogynecologic Society introduced the first standardised, objective, site-specific system (POP-Q) for describing, quantitating and staging pelvic organ support in women [5]. More recently, a simplified POP-Q method as been described as reliable and reproducible [17]. It has been shown that this system is easy to learn and teach, takes only 2 to 3 min to perform, has good intra- and inter-observer reliability as well as the reliability of the measurements as demonstrated by independent examiners on women in the lithotomy position [9]. This method of examination improves clinical and scientific communication about pelvic organ prolapse [18–22] due to the accurate and reproducible nature of these measurements.
Different patient positions during POP-Q examination such as lithotomy, upright and standing have been tried [10, 12, 13]. However, contradictory results have been reported [12–22]. Swift and Herring found no significant differences between points and stages when the POP-Q was performed in both supine and standing position [13]. However, due to limitations of examining standing, the authors were unable to complete two of the nine POP-Q measurements, genital hiatus and perineal body length.
Visco et al. noted a greater degree of prolapse in the standing position as compared with the supine lithotomy orientation [18].
Recently, Barber et al. [12], comparing when women were examined upright, found a greater stage of prolapse, confirming the findings of a previous studies [10].
In the Barber study, overall, the average values for each measurement increased in upright position but only by a relatively small amount. Although this was statistically significant, this increase was not clinically important, varying between 0.20 and 0.60 cm. However, there was moderate to good correlation between the POP-Q measurements made in each position [12].
Nevertheless, we have to accept that if members of ICS and AUGS, who are clinicians with special interest in urogynaecology and if less than half routinely use the POP-Q, it is unlikely that general gynaecologists will use this system in their practice [10].
In fact, many clinicians, especially those not in specialist centres, continue to prefer a digital vaginal examination and to define the pelvic organ prolapse using a four-grade scale (none, minimal, moderate and severe or 0, I, II and III degree prolapse) [11].
However, unlike the POP-Q, the reliability of the clinical examination of the pelvic organ prolapse using the above digital examination system in relation to the woman’s position has never been evaluated.
Although the examination position has not been standardised yet, lying supine or in the left lateral positions are the most commonly used during digital vaginal examination.
In our study, we have demonstrated that ‘digital examination’ of pelvic organ prolapse may be performed, but it is unreliable if the woman is supine. Digital examination in the standing position and an empty bladder is reliable and strongly correlates with prolapse symptoms and QOL impairment.
In our routine clinical practice, we prefer and strongly recommend examining the women with an empty bladder. In fact, accordingly to previous studies, we believe that a full bladder inhibits the performance of a full Valsalva manoeuvre, possibly related to the fear of urinary leakage during the episode of increased intraabdominal pressure. In addition, during the bladder storage phase, there is increased pelvic floor muscle tone and stimulation of somatic nerves to the striated urogenital sphincter, which is not ideal in demonstrating the maximal extent of prolapse [22].
One of the weaknesses of our study is that the intra-observer reliability has not been evaluated. This is due to the fact that we considered that it was not clinically ethical to reassess the woman again after 2 weeks.
Some authors have proposed that the maximum protrusion needs to be demonstrated as this is the problem which troubles a woman during her daily activities and thus there is an emphasis on the need to evaluate pelvic organ prolapse with a woman upright sitting in a birthchair [10, 13]. This position has been proposed to allow maximum hip flexion straightening out and enlarging the pelvic outlet, allowing the pelvic organs to protrude to a greater extent than the lithotomy position even with maximum Valsalva [13].
Although the upright position offers the advantage of assessing the pelvic organ prolapse with greater descent than examination in the supine position, the birthing chairs are not universally available, taking up a considerable amount of space and are expensive.
The fact that the women were not examined in the upright position and we did not measure the intensity of straining, evaluating the vesical or a rectal pressure, represents another weakness of our study.
In conclusion, even accepting that the POP-Q still remains the gold standard system to assess pelvic organ prolapse, if a clinician wants to perform a digital examination using a four-grade classification, this must be done with women in a standing position. In the clinical practice, this will help clinicians, in the absence of the POP-Q system, to assess more appropriately women with pelvic organ prolapse and to describe correctly the maximum protrusion noted by the individual during her daily activity as recommended by the ICS [5]. However, further studies to assess the clinical value of a digital examination in the management of women with POP as well to confirm our preliminary data are still needed.
References
Bump RC, Norton PA (1998) Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 25:723–746
Swift SE (2000) The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol 183:277–285
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Beck RP, McCormick S, Nordstrom L (1991) A 25-year experience with 519 anterior colporrhaphy procedures. Obstet Gynecol 78:1011–1018
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Baden WB, Walker TA (1992) Surgical repair of vaginal defects. JB Lippincott, Philadelphia
Beecham CT (1980) Classification of vaginal relaxation. Am J Obstet Gynecol 136:957–958
Porges RF (1963) A practical system of diagnosis and classification pelvic relaxation. Surg Gynecol Obstet 117:769–773
Hall AF, Theofrastous JP, Cundiff GW, Harris RL, Hamilton LF, Swift SE et al (1996) Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol 175:1467–1470
Auwad W, Freeman RM, Swift S (2004) Is the pelvic organ prolapse quantification system (POPQ) being used? A survey of members of the International Continence Society (ICS) and the American Urogynecologic Society (AUGS). Int Urogynecol J Pelvic Floor Dysfunct 15(5):324–327
Kustner O (1912) Prolapsus uteri et vaginea. In: Kustner O, Bumm E, Doederlein A, Kroening B, Menge C (eds) Kurzes Lehrbuch der Gynaekologie. G Fishers Publishers, Jena, pp 159–181
Barber MD, Lambers A, Visco AG, Bump RC (2000) Effect of patient position on clinical evaluation of pelvic organ prolapse. Obstet Gynecol 96:18–22
Swift SE, Herring M (1998) Comparison of pelvic organ prolapse in the dorsal lithotomy compared with the standing position. Obstet Gynecol 91:961–964
Digesu GA, Khullar V, Cardozo L, Robinson D, Salvatore S (2005) P-QOL: a validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int Urogynecol J Pelvic Floor Dysfunct 16(3):176–181
Altman DG (1999) Practical statistics for medical research. Chapman & Hall/CRC, Boca Raton
Brubaker L, Norton P (1996) Current clinical nomenclature for description of pelvic organ prolapse. J Pelvic Surg 2:257–259
Swift S, Morris S, McKinnie V, Freeman R, Petri E, Scotti RJ, Dwyer P (2006) Validation of a simplified technique for using the POPQ pelvic organ prolapse classification system. Int Urogynecol J 17(6):615–620
Visco AG, Wei JT, McClure LA, Handa VL, Nygaard IE (2003) Effects of examination technique modifications on pelvic organ prolapse quantification (POP-Q) results. Int Urogynecol J Pelvic Floor Dysfunct 14:136–140
Grody MHT (1997) Posterior compartment defects. In: Rock J, Thompson T (eds) Telinde’s operative gynecology. 8th edn. Lippincott-Raven Press, Philadelphia, pp 1044–1056
Walters MD, Karram MM (1992) Enterocele. American Urogynecologic Society quarterly report. American Urogynecologic Society, Chicago 10
Benson TJ, Walters MD (1999) Neurophysiology of the lower urinary tract. In: Walters MD, Karram MM (eds) Urogynecology and reconstructive pelvic surgery. 2nd edn. Mosby, St. Louis (MO), pp 15–24
Silva WA, Kleeman S, Segal J, Pauls R, Woods SE, Karram MM (2004) Effects of a full bladder and patient positioning on pelvic organ prolapse assessment. Obstet Gynecol 104(1):37–41
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Digesu, G.A., Khullar, V., Cardozo, L. et al. Inter-observer reliability of digital vaginal examination using a four-grade scale in different patient positions. Int Urogynecol J 19, 1303–1307 (2008). https://doi.org/10.1007/s00192-008-0635-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-008-0635-6