Abstract
Introduction and hypothesis
This study aims to elucidate and expand current knowledge of the uterosacral ligament (USL) from a surgical viewpoint.
Methods
Studies were performed on 12 unembalmed cadaveric pelves and five formalin-fixed pelves.
Results
The USL, 12–14-cm long, can be subdivided into three sections: (1) distal (2–3 cm), intermediate (5 cm), and proximal (5–6 cm). The thick (5–20 mm) distal section, attached to cervix and upper vagina, is confluent laterally with the cardinal ligament. The proximal section is diffuse in attachment and generally thinner. The relatively unattached intermediate section is wide, and thick, well defined when placed under tension, more than 2 cm from the ureter and suitable for surgical use. The strength of the USL is perhaps derived not only from the ligament itself, but also from the addition of extraperitoneal connective tissue.
Conclusions
The USL can be subdivided into three sections according to thickness and attachments with the intermediate section suitable for surgical use, particularly for vaginal vault support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The uterosacral ligament (USL) has become an increasing focus of interest in terms of its use for surgical support in the management of pelvic organ prolapse [1–11]. Intraperitoneal techniques used to date [1–9] are known to carry the risk of neurovascular or ureteric damage with extraperitoneal techniques in development [10–12] seeming to be at a lesser risk. There have been some previous studies to identify the USL’s anatomical relationships, in particular, to the ureter, to improve surgical safety [13, 14]. There has been no systematic mapping of the USL including the total length and relative lengths of different sections. Previous descriptions [13–15] have divided the USL into three segments, cervical, intermediate, and sacral, without clear justification for making them “equal” in length. In terms of total length, the only one cited we could find was a mean cranio-caudal length using MRI studies [16] of 21 ± 8 mm (range 10–50 mm).
The published descriptions of the anatomy of the USL have differed widely. The proximal attachment has been the subject of controversy with some believing it connects to the sacrum [13–15] while others postulating an attachment to the sacrospinous ligament and coccygeus [16]. While some authors [13, 15], distinguish between the USL and the so-called (as there is controversy over terminology) cardinal ligament (CL), others [10, 17] refer to a less defined “uterosacral-cardinal ligament complex”. The surgical literature has noted the USL to be a dense, strong band of connective tissue. However, cadaveric and histological studies have generally demonstrated no condensed ligamentous structures [17].
There is some consensus on the USL’s neurovascular contents. The lateral and deeper aspects of the USL and the CL have been shown to contain large nerve trunks and ganglia from the superior hypogastric plexus [18]. The S1–S4 trunks of the sacral plexus, not the pudendal nerve, have been deemed to be vulnerable to injury during a uterosacral suspension procedure [19].
Our aim is firstly to elucidate the macroscopic aspects of the USL including its total length, an appropriate division into sections, and the relative lengths of these sections, as well as the USL proximal and distal attachments, including its distal confluence with the CL. We also intend to review established findings on the neurovascular relations of the USL. From this analysis, we will make surgically relevant anatomical conclusions, particularly in regard to vaginal vault support at pelvic reconstructive surgery
Materials and methods
There were three aspects to our studies of the USL: [1] Observations were made on ten unembalmed cadaveric pelves when they were dissected for the purpose of teaching gynecology trainees; [2] Dissection was carried out on two unembalmed cadaveric pelves; [3] Dissection was also carried out on five formalinized hemipelves. All the cadavers were bequeathed to the Department of Anatomy, School of Medical Sciences, University of New South Wales, Sydney, Australia for scientific and teaching purposes. Only one pelvis was known to be nulliparous from the donor’s medical records; the remaining pelves did not have parity recorded on files but had parous cervical appearance. None of the dissected cadavers had evidence of previous pelvic surgery.
Terminology
One cause of confusion in the description of the USL in the literature has been a lack of rigorously defined terminology. In this paper, anatomical terminology is used to describe relations and direction. The sacrum is described as posterior and the pubic symphysis anterior. The iliac crest is described as being cranial to the pelvic floor. As to attachments of the ligaments, their attachment [1] to the sacrum is described as sacral or proximal (closer to the axis of the body) and [2] to the cervix as cervical or distal (further from the axis of the body).
Dissection of the unembalmed pelves
Fresh frozen cadavers were cut above the iliac crest and the gastrointestinal tube excised just proximal to the rectosigmoid junction to facilitate the study of relations of the USL.
Anterior traction was applied to the uterine fundus to accentuate the sacrouterine folds (also known as rectouterine folds), and the peritoneum was incised along the crest of the peritoneal folds. Peritoneum was carefully dissected off the underlying structures, on both the anterior and posterior surfaces of the fold, from the incision caudally down to the pelvic floor. Care was taken to preserve all the connective tissue and neurovascular structures lying deep to the peritoneum. The peritoneum was peeled off caudally to the pelvic floor and laterally to expose the entire lateral pelvic wall from the sacrum to the pubic symphysis. Fat was carefully removed to expose the connective tissue and neurovascular structures. The entire USL was identified; its appearance, attachments, and relations with surrounding structures were noted.
Dissection of the embalmed hemipelves
The embalmed pelves were sectioned at the median plane. Dissection began from the median plane, and the peritoneum was carefully detached to expose the underlying structures from the midline to the lateral pelvic wall, leaving intact the underlying connective tissue and neurovascular structures. The appearance of the USL, its attachments, and the relations of the ligament with surrounding structures were noted.
Measurements were taken with a flexible ruler, and readings were recorded to the nearest 0.1 cm.
Results
When traction was applied to the uterine fundus, the sacrouterine peritoneal folds always extended from the corner of the uterus to the sacrum up to the level of the second or first sacral segment (Fig. 1). It draped the USL, but it extended much further cranially than the latter. When the peritoneum was incised at its crest, it was evident that the strip of the fold from the crest was only a duplication of the peritoneum.
The USL was considered to begin when connective tissue was first encountered as the peritoneum was “peeled” off from the incision. The general direction of the ligament was from the cervico-vaginal junction, curving posteriorly on the side of the rectum, to reach the sacroiliac joint.
Three sections of the USL
The total length of the USL ranged from 12 to 14 cm. Based on the thickness and attachments of the ligament, it can be subdivided into three sections: distal (cervical), intermediate, and proximal (sacral; Fig. 2).
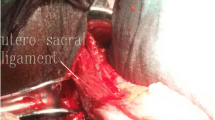
The distal (cervical) section was the thickest portion (Fig. 2). At the edge of the cervix and vagina, it was fused with the CL (Figs. 2 and 3). When it became separated from the latter, it measured 20–30 mm in vertical length and 5–20 mm in thickness. Macroscopically, this distal section was made up of dense connective tissue containing small blood vessels and small branches of the hypogastric plexus.
The intermediate section averaged 5 cm in length and 5 mm in thickness (Fig. 4), and it thinned out gradually as it progressed posteriorly. It was best seen when anterior traction was applied to the uterus.
The proximal (sacral) section was on average 5.5-cm long but was variable in thickness (up to 0.5 cm) and appearance. This section was consistently discernible as a thin sheet of connective tissue with no clear fibrillar appearance. In three hemipelves, the ligament was a thick and dense ligamentous structure, with clear parallel bundles similar to the appearance of ligaments of large joints. In all specimens, the ligament was thin at its free border and thicker closer to the pelvic floor, this thickness difference being more pronounced in the three instances with dense ligamentous appearance.
Attachments of the USL
Cervical attachment
The USL was found attached to the cervix and vaginal vault in all pelves of this series. Its attachment was mostly but not exclusively on the posterior aspect of the cervico-vaginal junction. It also spreads to the lateral aspects of the junction, where its fibers were seen to interlace with the attachment of the CL. The two ligaments appeared to fuse together into one single unit and were not easily separated from each other for a distance of 2 cm from the lateral aspect of the cervix. Beyond that point, the CL remained a thick bundle of connective tissue which ran postero-laterally to a broad triangular area of attachment on the lateral wall of the pelvis, the apex of the triangle reaching as high cranially as the point where the internal iliac artery began to branch. The USL continued posteriorly on the medial side of the CL as a well-defined discrete bundle of connective tissue (Fig. 3).
Sacral attachment
In all pelves, the ligament could be traced posteriorly to its attachment over the area of the sacroiliac joint and the lateral edge of the sacrum. It was not attached directly to the joint or the sacrum, only to the overlying fascia. It extended vertically from the sacrococcygeal joint to the level of the third piece of the sacrum. The upper border of the ligament was very thin, covered by the sacrouterine peritoneal fold which extended further cranially to the level of the second piece of the sacrum, or to the first piece of the sacrum in two hemipelves. The attachment to pelvic fascia was mainly over the sacroiliac joint and the sacrum, but it also spreads as a thin extension, from the pelvic sacral foramina medially to the fascia overlying piriformis and levator ani, about 5 cm lateral to the sacroiliac joint. Caudally, it spreads out over the fascia overlying the levator ani muscle. The sacral portion of its inferior border appeared to continue into the so-called (again some controversy on terminology) lateral ligament of the rectum.
Relations of the USL
Relation with the ureter
The ureter entered the lesser pelvis at the bifurcation of the common iliac artery, crossed the uterine artery at the base of broad ligament, and then ended anterior to the cervix to reach the base of the bladder. At the cervix, it was located anterior to the CL and was on the average 0.7–1 cm lateral to the cervix. The ureter therefore was located in a plane anterior to the USL, and when measured along the free border of the ligament, it was 2–3 cm from the cervical attachment of the ligament (Fig. 5).
Relations with neurovascular structures
The sacral attachment of the USL was just lateral to the sacral sympathetic trunks and ganglia and the emergence of the sacral nerve roots S2, S3, and S4. The medial aspect of the ligament lying against the rectum was mostly fibrous. The pelvic splanchnic nerves and the hypogastric plexus were found on the lateral side of the ligament after teasing off the fibers from its rectal side.
The arteries and veins were on a plane even more lateral to the neural plane (Fig. 6). The sacral portion of the USL spreads caudally toward the lateral ligament of the rectum, which was a band of connective tissue accompanying the middle rectal artery as it reached the rectum from its origin from the internal iliac artery. The middle rectal artery was thus located close to the caudal border of the sacral section of the USL. At the level of the upper border of the sacral section, but lateral to it, were the superior gluteal artery and vein. They were more closely related to the pelvic attachment of the CL and 4–5 cm lateral to the USL.
Discussion
In order to reappraise macroscopically the structure, relations, and attachments of the USL, traditional method of dissection was used, similar to the method described by the comprehensive study of Blaisdell [14]. Our findings concurred with his macroscopic observations, but we have gone further to clarify the layered organization of the neurovascular structures in the USL.
We see our study as the first to cite the overall and sectional USL length on the basis of thickness and attachments. While we agree with the sectional names, proximal (sacral), intermediate, and distal (cervical) used in previous series [13, 15], we do not see them as “equal” sections in length. In terms of overall cranio-caudal length, our “direct anatomical” measure of 12–14 cm is different to the equivalent measurement of 21 ± 8 mm on axial MRI scans [16].
Our study clarifies the USL attachments from the descriptions in previous studies [13–16]. While there is a consensus on its distal attachment to the vaginal dome and neighboring cervix, the nature of the confluence of the USL with the CL over a length of around 2 cm from the lateral aspect of the cervix and the subsequent separation of the ligaments into separate entities have not been highlighted. According to the 1998 Terminologia Anatomica and recent efforts to re-classify the pelvic connective tissue, these two “ligaments” belong to two groups of fascia [20, 21]. We would not favor the term “uterosacral-cardinal ligament complex” [10, 17] as a global term for the two “ligaments.”
Our study offers a more comprehensive description of the sacral attachment of the USL, which has so far differed widely in the literature. Many factors could explain the discrepancies. Definition is the first factor. When the USL is defined as synonymous with sacrouterine fold (or rectouterine/sacrogenital fold), then its sacral attachment extends to the first segment of the sacrum [22]. When the ligament is considered as part of the endopelvic fascia, the proximal attachment will be even more arbitrary and widespread transversely [23, 24]. Another factor is the author’s opinion on how much connective tissue would be considered as the ligament. In this series, when the sacrouterine peritoneal fold was opened, the underlying connective tissue appeared a few centimeters caudal to the fold and thickened gradually. The ligament began where the connective tissue was of noticeable thickness. As this point was relatively arbitrarily defined, the attachment and extent of the ligament would vary in different descriptions. The findings of our dissections do not concur with the conclusion of Umek et al. [15] whose series of MRI images of 82 subjects indicated that the USL was attached to the sacrospinous ligament and coccygeus muscle in 82% of cases, to the piriformis muscle in 11%, and to the sacrum in only 7%.
We generally support previous descriptions of the ureteric relations of the USL [13]. The separations of USL from ureter (0.7–1 cm from the cervical section of the USL and 2–3 cm from the intermediate section) are similar to the findings of Buller et al. ([13] – 0.9 ± 0.4 and 2.3 ± 0.9 cm, respectively).
We also agree, in general, with previous descriptions of the neurovascular relations of the USL [25–29]. In our series, there was a clear “layering” of neurovascular structures in the ligament (Fig. 6), especially in its proximal section: The medial layer was almost entirely composed of connective tissue, the middle layer was the neural plane, and the most lateral layer was the vascular plane. Butler-Manuel et al. [25] had first noted the greater predominance of neural tissue in the middle and lateral thirds of the USL. The hypogastric plexus is formed at an area anterolateral to the rectum [26] and lies on the lateral surface of the ligament [25]. Sutures place in this section, especially beginning from the medial side with poorly controlled depth, could damage the hypogastric plexus on its lateral side [25] and may even entrap the sacral nerve trunks S2–S4 [19] especially if the sutures are placed lateral to the ligament or too close to the pelvic wall [27].
The importance of the USL as a uterine support has been highlighted [30]. Its intermediate section appears to be the safest section for surgical fixation. Most commonly, this would be for vaginal vault fixation in pelvic reconstructive surgery. It is thick and strong in our series; it contains predominantly connective tissue [13], and it has the lowest count of nerve fiber bundles. In our series, it is again farther from the ureter than the cervical section and farther from the sacral nerve trunks and the pelvic splanchnic nerves than the sacral section.
The appearance of the ligament has been described as strong bands of connective tissue [13, 19]. In this series, most of the ligaments had the appearance of a membrane of connective tissue with no obvious fibrillar arrangement. Only in three hemipelves did the caudal part of the ligament has a strong ligamentous appearance and, even in those cases, only in their caudal half. This observation concurs with previous reports which found no true microscopic evidence of an organized condensed ligamentous structure [17] except for a small percentage of the specimens studied [24]. However, it has been proven that the USL has adequate tensile strength to serve as a good support for vaginal vault fixation [13]. In a series of 14 hemipelves, Cole et al. [24] noted poorly organized connective tissue with sparse collagen fibers and low cellularity in most of the specimens, except for three specimens which had a clearly ligamentous structure with organized collagen fibers and interspersed elastic fibers.
Conclusion
While the USL has taken many different guises under the pens of different authors for decades, we believe its sections and proximal and distal attachments can be clearly described. Our findings on neurovascular relations are largely consistent with previous studies. The intermediate section merits consideration for surgical use, e.g., vaginal vault fixation, on the basis of its strength and safety. While some have even questioned the term “ligament” because there rarely has been histological evidence that it has an orderly organization of collagen and elastic fibers of a ligament, it has been proven to have a tensile strength and has served as a good support for vaginal vault fixation. It is probable that its strength derived also from the surrounding extraperitoneal connective tissue and endopelvic fascia that is included in any uterosacral suspensory sutures.
References
Miller N (1927) A new method of correcting complete inversion of the vagina: with or without complete prolapse: report of 2 cases. Surg Gynecol Obstet 44:550–555
McCall ML (1957) Posterior culdoplasty: surgical correction of enterocoele during vaginal hysterectomy; a preliminary report. Obstet Gynecol 10:595–602
Jenkins VR 2nd (1997) Uterosacral ligament fixation for vaginal vault suspension in uterine and vaginal vault prolapse. Am J Obstet Gynecol 177:1337–1343
Barber MD, Visco AG, Weidner AC, Amundsen CL, Bump RC (2000) Bilateral uterosacral ligament vaginal vault suspension with site-specific endopelvic fascia defect repair for treatment of pelvic organ prolapse. Am J Obstet Gynecol 183:1402–1410
Shull BL, Bachofen C, Coates KW, Kuehl TJ (2000) A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol 183:1365–1373
Karram M, Goldwasser S, Kleeman S, Steele A, Vassallo B, Walsh P (2001) High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocoele and vaginal vault prolapse. Am J Obstet Gynecol 185:1339–1343
Amundsen CL, Flynn BJ, Webster GD (2003) Anatomical correction of vaginal vault prolapse by uterosacral ligament fixation in women who also require a pubovaginal sling. J Urol 169:1770–1774
Silva WA, Pauls RN, Segal JL, Rooney CM, Kleeman SD, Karram MM (2006) Uterosacral ligament vault suspension: five-year outcomes. Obstet Gynecol 108:255–263
Park AJ, Ridgeway B, Gustilo-Ashby AM, Paraiso MFR, Walters MD, Barber MD (2008) Efficacy of a standardized technique of trans-vaginal entry into the peritoneal cavity for post-hysterectomy vaginal vault suspension. Int Urogynecol J 19:1393–1398
Dwyer PL, Fatton B (2008) Bilateral extraperitoneal uterosacral suspension: a new approach to correct posthysterectomy vaginal vault prolapse. Int Urogynecol J 19:283–292
Fatton B, Dwyer PL, Achtari C, Tan PK (2009) Bilateral extraperitoneal uterosacral vaginal vault suspension: a 2 year follow-up longitudinal case series of 123 patients. Int Urogynecol J 20(4):427–434
Haylen BT, Yang V, Vu D, Tse K (2009) Midline uterosacral suspension anterior colporrhaphy combo (MUSSACC): preliminary report. Int Urogynecol J (in press)
Buller JL, Thompson JR, Cundiff GW, Sullivan LK, Schön Ybarra MAS, Bent AE (2001) Uterosacral ligament: description of anatomic relationships to optimize surgical safety. Obstet Gynecol 97(6):873–879
Blaisdell FE (1917) The anatomy of the sacro-uterine ligaments. Anat Rec 12:1–42
Campbell R (1950) The anatomy and histology of the sacrouterine ligaments. Am J Obstet Gynecol 59:1–12
Umek WH, Morgan DM, Ashton-Miller JA, DeLancey JOL (2004) Quantitative analysis of uterosacral ligament origin and insertion points by magnetic resonance imaging. Obstet Gynecol 103(3):447–451
Ramanah R, Parratte B, Arbez-Gindre F, Maillet R, Riethmuller D (2008) The uterosacral complex: ligament or neurovascular pathway? Anatomical and histological study of fetuses and adults. Int Urogynecol J 19:1565–1570
Butler-Manuel SA, Buttery LDK, Polak JM, A’Hern RA, Barton DJP (2008) Autonomic nerve trauma at radical hysterectomy: the nerve content and subtypes within the superficial and deep uterosacral ligaments. Reprod Sci 1:91–96
Siddique SA, Gutman RE, Schön Ybarra MA, Rojas F, Handa VL (2006) Relationship of the uterosacral ligament to the sacral plexus and to the pudendal nerve. Int Urogynecol J 17:642–645
Ercoli A, Delmas V, Fanfani F, Gadonneix P, Ceccaroni M, Fagotti A, Mancuso S, Scambia G (2005) Terminologia Anatomica versus unofficial descriptions and nomenclature of the fasciae and ligaments of the female pelvis: a dissection-based comparative study. Am J Obstet Gynecol 193:1565–1573
Yabuki Y, Sasaki H, Hatakeyama N, Murakami G (2005) Discrepancies between classic anatomy and modern gynecologic surgery on pelvic connective tissue structure: harmonisation of those concepts by collaborative cadaver dissection. Am J Obstet Gynecol 193:7–15
DeCherney AH, Nathan L, Goodwin TM, Laufer N (2006) Current obstetrics and gynecologic diagnosis and treatment, 10th edn. McGraw-Hill Medical, New York, p 46
Otcenasek M, Baca V, Ladislaw K, Jaroslaw F (2008) Endopelvic fascia in women. Obstet Gynecol 111:620–630
Cole EE, Leu PB, Gomelsky A, Revelo P, Shappell H, Scarpero HM, Dmochowski RR (2006) Histopathological evaluation of the uterosacral ligament: is this a dependable structure for pelvic reconstruction? BJU Int 97(2):345–348
Butler-Manuel SA, Buttery LDK, A’Hern RP, Polak JM, Barton DPJ (2000) Pelvic nerve plexus trauma at radical hysterectomy and simple hysterectomy. Cancer 89(4):834–841
Tong XK, Huo RJ (1991) The anatomical basis and prevention of neurogenic voiding dysfunction following radical hysterectomy. Surg Radiol Anat 13(2):145–148
Maas CP, Trimbos JB, DeRuiter MC, van de Velde CJH, Kenter GG (2003) Nerve sparing radical hysterectomy: latest developments and historical perspective. Crit Rev Oncol Hematol 48:271–279
Trimbos JB, Maas CP, DeRuiter MC, Peters AAW, Kenter GG (2001) A nerve-sparing radical hysterectomy: guidelines and feasibility in western patients. Int J Gynecol Cancer 11:180–186
Wieslander CK, Roshanravan SM, Wai CY et al (2007) Uterosacral ligament suspension sutures: anatomic relations in unembalmed female cadavers. Am J Obstet Gynecol 197:672e1–672e6
Fritsch H, Lienemann A, Brenner E, Ludwikowski B (2004) Clinical anatomy of the pelvic floor. Adv Anat Embryo Cell Biol 175(III–IX):1–64
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vu, D., Haylen, B.T., Tse, K. et al. Surgical anatomy of the uterosacral ligament. Int Urogynecol J 21, 1123–1128 (2010). https://doi.org/10.1007/s00192-010-1147-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1147-8