Abstract
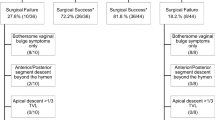
The aim of this paper is to describe the efficacy and safety of a standardized technique of trans-vaginal entry into the peritoneal cavity for post-hysterectomy vault prolapse and determine how well the pre-operative pelvic examination predicted successful peritoneal entry. A retrospective review of patients undergoing post-hysterectomy trans-vaginal apical suspensions using a standardized technique of peritoneal entry was employed in this study. A subset of patients underwent a standardized pre-operative evaluation to predict what organ was behind the vaginal cuff and posterior cul-de-sac. Peritoneal entry was attempted in 280 patients, and successfully achieved in 223(80%). One cystotomy and one proctotomy (0.3%) occurred during attempted entry. Of those who underwent the standardized pre-operative evaluation, peritoneal entry was successful 86% of the time when small bowel was predicted to lie behind the vaginal cuff or posterior cul-de-sac. Peritoneal entry can be safely achieved in the majority of post-hysterectomy prolapse patients. Pre-operative examination assists in predicting successful peritoneal entry.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse is estimated to affect up to a third of women [1, 2]. Of this group, post-hysterectomy vaginal vault prolapse is a common condition. Options for treatment include abdominal, laparoscopic, and vaginal approaches. In the United States, over 90% of procedures for prolapse are performed vaginally [3]. The advantage to the vaginal, compared to the abdominal, approach is decreased morbidity and recovery time, avoidance of the presacral vessels in the case of the abdominal sacral colpopexy, and better cosmetic outcome.
Vaginal procedures that address apical prolapse can be divided into extra-peritoneal and intra-peritoneal techniques. Extra-peritoneal techniques include the sacrospinous ligament fixation, the iliococcygeus fixation, and certain newer trans-vaginal mesh kit procedures. Intra-peritoneal procedures include the McCall’s or Mayo culdoplasty and the uterosacral ligament vaginal vault suspension. Compared with the sacrospinous ligament fixation, the Mayo culdoplasty and uterosacral vault suspensions preserve the natural orientation of the vaginal axis.[4–6] Although no randomized trials have yet been done, the 5-year outcomes for the uterosacral vault suspension show a failure rate of 15% [6], which is roughly comparable to the results obtained after other types of vaginal vault suspension [7].
Some gynecologic surgeons are hesitant to perform an intra-peritoneal vault suspension in patients with post-hysterectomy vault prolapse, due to a perceived difficulty in accessing the peritoneal cavity. This issue has rarely been specifically addressed in the literature. Our primary aim of this study was to describe the efficacy and safety of a standardized technique of trans-vaginal entry into the peritoneal cavity for trans-vaginal vault suspension in the treatment of pelvic organ prolapse. A second aim of this study was to determine how well the pre-operative pelvic examination predicted successful entry into the peritoneal cavity using this standardized technique, i.e., whether small bowel or an enterocele was lying behind the vaginal apex or the posterior cul-de-sac [8].
Materials and methods
After Institutional Review Board approval was obtained, we conducted a retrospective review of all 342 patients undergoing post-hysterectomy trans-vaginal apical suspensions for prolapse by three surgeons at an academic tertiary care hospital during 2001–2006. Data were collected on patient demographics, pre-operative pelvic organ prolapse (either Baden–Walker or POP-Q) stage, prior prolapse or incontinence surgery, and operating room data with regards to successful entry into the peritoneal cavity and complications related to attempted peritoneal entry. Successful entry was defined as entrance into the peritoneal cavity and was not time-dependent. Three reviewers (AJP, BR, and AMG) collected all the pertinent data. The first author made the final judgment on any ambiguous issues in chart review, e.g., whether peritoneal entry was attempted and another type of vaginal colpopexy was performed in lieu of an intra-peritoneal procedure. Statistical analysis was performed with the chi-squared test using JMP 6.0.
During the study period, there was also a project where patients underwent a standardized pre-operative evaluation to predict what organ was behind the POP-Q points Aa, Ba, C, Ap, Bp—i.e., bladder, small bowel, sigmoid colon, rectum, or scar. This pre-operative evaluation was performed in a subset of the study population of 127 patients. These POP-Q points have been previously defined [8]; the hymen serves as a reference landmark with the plane of the hymen as 0. The anatomic position of the other points (Aa, Ba, C, Ap, Bp) are described in reference to the hymen in centimeters above or proximal to the hymen (negative number), or centimeters below or distal to the hymen (positive number). Aa is located in the midline of the anterior vaginal wall 3 cm proximal to the external urethral meatus, corresponding to the approximate location of the urethrovesical junction, defined as −3 to +3 cm relative to the hymen. Ba is the point most distal or dependent of any part of the proximal anterior vaginal wall from the vaginal cuff or anterior vaginal fornix to point Aa. This point is defined as −3 cm in the patient without prolapse and a positive value equal to the position of the cuff in women with total post-hysterectomy vault prolapse. Point C represents the leading edge of the vaginal cuff. Points Ap and Bp are the analogous points to Aa and Ba on the posterior vaginal wall. Ap is located in the midline posterior vaginal wall 3 cm proximal to the hymen, ranging from −3 to +3 cm, while Bp is the most dependent position of the proximal posterior vaginal wall from the vaginal cuff to point Ap, with the values ranging from −3 cm in the subject with normal vaginal anatomy and a positive value equal to the position of the cuff in a patient with total vault eversion. Data were also collected on an additional point called point X (see Figs. 1 and 2). This point X was designated at a location half-way down the posterior vaginal wall between the points Ap and C, i.e., between a point 3 cm proximal to the hymen on the midline posterior vagina and the vaginal cuff. It was meant to roughly correlate to the location of the posterior cul-de-sac. These POP-Q points were obtained during maximal prolapse elicited in the dorsal lithotomy position while the subject performed a Valsalva maneuver. Rectovaginal examination and evaluation of levator function were also performed at the time of the POP-Q.
An example of the pre-operative evaluation to predict what organ was behind each POP-Q in a subject with normal vaginal anatomy. The pubic symphysis is represented as the black oval. In the subject with normal vaginal anatomy, assuming the uterus has been removed, one would expect the bladder to lie behind points Aa and Ba, scar, or small bowel to be behind point C, and the rectum to lie beneath points Ap, Bp, and X. To reiterate, point X is the point half-way between Ap and C and is meant to designate the posterior cul-de-sac
An example of the pre-operative evaluation to predict what organ was behind each POP-Q in a subject with Stage IV prolapse, or total vaginal vault eversion. The pubic symphysis is represented as the black oval. In the subject with Stage IV prolapse, one could predict that the bladder lies behind point Aa, the rectum lies behind point Ap, while an enterocele or small bowel would lie behind the rest of the POP-Q points of Ba, C, Bp, and X
Technique
Our standardized technique for entry into the peritoneal cavity consists of first identifying the vaginal cuff scar. Allis clamps are placed at the dimples at the lateral edges of the vaginal cuff, at the midpoint of the vaginal cuff, and in the posterior cul-de-sac (Fig. 3). These Allis clamps are pulled on tension in order to create a diamond shape (Fig. 4). Next, the vaginal epithelium overlying this diamond-shaped wedge is excised (Fig. 5). We then dissect the areolar tissue off the rectum while concomitantly performing a rectal exam with the non-dominant hand (Fig. 6). If necessary, we will pass a uterine sound through the urethra or perform a retrograde filling of the bladder to demarcate the borders of the bladder. Once the peritoneum is visualized, it is grasped with two hemostats and incised in order to enter to the peritoneal cavity (Fig. 7). A Credé maneuver may be performed in order to visualize bowel epiploicae behind the peritoneum as a confirmatory technique. Once peritoneal entry was achieved, a uterosacral vault suspension was performed by grasping the uterosacral ligament with long Allis clamps at the level of the ischial spine and passing a 0 PDS and a 0 Prolene suture from lateral to medial. The 0 PDS suture was anchored into the anterior epithelium at the new vaginal apex and the 0 PDS was anchored into the anterior vaginal muscularis or into the anterior colporrhaphy if performed, and into the posterior vaginal muscularis, making sure to avoid exiting through the vaginal epithelium in order to avoid extrusion of this permanent suture material and avoid the potential risk of future granulation tissue.
Results
During a 6-year period, 342 patients with post-hysterectomy vaginal prolapse underwent a trans-vaginal apical suspension procedure. Of these 342 patients, 62 patients (18%) had a planned extra-peritoneal vault suspension (i.e., 49 sacrospinous ligament fixations or iliococcygeus fascia suspensions, and 13 vaginal mesh kits). Peritoneal entry was attempted in 280 patients (82%). This group represents our study population. Baseline demographics are listed in Table 1.
Of our study population, successful peritoneal entry was achieved in 223 patients (80%). In the remaining 20%, or 57 patients, where access to the peritoneal cavity was not achieved, these patients either had an extra-peritoneal vaginal vault suspension (54 patients, or 95%) or no vault suspension was performed (three patients, or 5%). In terms of complications, there was one cystotomy and one proctotomy, with a rate of 0.3% for both (95% CI [0.06%–1.9%]). After the cystotomy was repaired, an iliococcygeus fascia suspension was performed. In the case of the proctotomy, the surgeon elected not to do a vaginal vault suspension.
One hundred twenty-seven subjects (45%) had a standardized pre-operative evaluation to predict what organ was behind each POP-Q point and point X. Regarding the question of whether the pre-operative POP-Q examination can predict successful peritoneal entry, we had an 86% success rate in entering the peritoneal cavity when small bowel (i.e., an enterocele) was predicted to lie behind POP-Q points C or X. These points of C and X were chosen as, empirically, they would be the most relevant in gaining peritoneal access at the site of an enterocele anywhere in the proximal third of the posterior vaginal wall. In contrast, if any other viscera or scar was predicted to lie behind these two points, successful entry occurred only 46% of the time (p < 0.0001).
We also examined whether prolapse stage or prior surgery for prolapse or incontinence affected the peritoneal entry rates. Prior surgery for prolapse or incontinence did not affect the ability to enter the peritoneal cavity (p = 0.8 and 0.9, respectively). Increasing stage of prolapse was associated with increased peritoneal entry rates (p < 0.02 for trend), with successful entry into the peritoneal cavity by stage of prolapse as follows: 74% for Stage II, 78% for Stage III, and 100% for Stage IV prolapse. Small bowel was predicted to be behind points C or X 15% of the time in Stage 2 prolapse, 66% in Stage 3 prolapse, and 90% of the time in Stage 4 prolapse.
Discussion
Post-hysterectomy vaginal prolapse is common; according to the data from the Women’s Health Initiative, almost 38% of women after hysterectomy have some form of prolapse [2]. The method of surgical repair can be abdominal, laparoscopic, or vaginal, with vaginal surgery being the most commonly performed prolapse repair in the United States.
Our study demonstrates that this standardized technique for trans-vaginal entry into the peritoneal cavity is associated with few complications and can be safely achieved in the majority of patients with post-hysterectomy vaginal prolapse. The advantage of performing an intra-peritoneal vault suspension, i.e., a McCall’s culdoplasty or uterosacral vault suspension, lies in the ability to perform a more anatomically correct prolapse repair that preserves the natural axis of the vagina. The long-term outcomes of these techniques have been shown to be good [4–6]. Nevertheless, the choice of whether to perform an intra- vs. extra-peritoneal vaginal vault suspension technique ultimately lies with the surgeon, as well as the specific prolapse sites and anatomic defects of each individual patient. As with any surgical procedure, the success and safety of this technique depends on the technical skill and comfort level of the surgeon. These data demonstrate the experience at an academic tertiary care institution where these procedures were primarily performed by fellows. This technique has been utilized at our institution for approximately 30 years.
Interestingly, prior prolapse or incontinence surgery did not affect the ability to successfully enter the peritoneal cavity. The cystotomy and proctotomy occurred in patients who had prior prolapse repairs; both of these patients had had vaginal hysterectomies and anterior and posterior colporrhaphies. Nevertheless, the number of patients who suffered from visceral injury on attempted entry is too small to draw any conclusions regarding prior prolapse surgery as a risk factor for injury.
Peritoneal entry rates increased by stage of prolapse, with 100% success in entering the peritoneal cavity in Stage IV prolapse. This reflects that the fact that there were more enteroceles in advanced prolapse with pronounced herniation of the vagina and its support structures. With lower stages of prolapse, the peritoneal entry rate is lower possibly because of a lower enterocele rate and that the access to the vaginal apex area is decreased compared to Stage IV prolapse.
In the subset of patients who underwent a standardized pre-operative evaluation to predict which organ was behind each POP-Q point, we found that the surgeon’s prediction of an enterocele behind points C or X (i.e., the cuff or posterior cul-de-sac) was significantly correlated with successful peritoneal entry. Although the ability to predict the underlying organ depends on the clinical judgment and experience of the surgeon, if one could develop this skill, this would assist in pre-operative surgical planning.
The main strength of this study is the large number of patients from our institution where peritoneal entry was attempted using this standardized technique. The study was limited by its retrospective nature and by the quality of the dictated operative reports. The primary author reviewed all the operative notes and standardized the criteria for inclusion into the study in terms of attempting trans-vaginal entry into the peritoneal cavity. The main criterion to determine attempted trans-vaginal entry was judged by both the initial approach dictated in the operative note, i.e., initial excision of the diamond-shaped vaginal epithelium, as well as the description of the attempted entry.
In conclusion, patients with post-hysterectomy vaginal vault prolapse should not be limited only to extra-peritoneal techniques such as sacrospinous ligament fixations, iliococcygeus fascia suspensions, or mesh kits, as intra-peritoneal entry can safely and effectively be achieved in the vast majority of cases. Further study via prospective randomized surgical trials is warranted in order to compare which apical vaginal suspension technique is superior.
References
Samuelsson EC, Arne Victor FT, Tibblin G, Svardsudd KF (1999) Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol 180:299–305
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A (2002) Pelvic organ prolapse in the women’s health initiative: gravity and gravidity. Am J Obstet Gynecol 186:1160–1166
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Webb MJ, Aronson MP, Ferguson LK, Lee RA (1998) Posthysterectomy vaginal vault prolapse: primary repair in 693 patients. Obstet Gynecol 92:281–285
Karram M, Goldwasser S, Kleeman S, Steele A, Vassallo B, Walsh P (2001) High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse. Am J Obstet Gynecol 185:1339–1342 discussion 1342–3
Silva WA, Pauls RN, Segal JL, Rooney CM, Kleeman SD, Karram MM (2006) Uterosacral ligament vault suspension: five-year outcomes. Obstet Gynecol 108:255–263
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM et al (2004) Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol 104:805–823
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Conflicts of interest
Dr. Paraiso is a paid instructor for Ethicon and a paid consultant for American Medical Systems; Dr. Walters is a paid consultant for American Medical Systems; Drs. Park, Barber, Ridgeway, Gustilo-Ashby have no disclosures
Financial support
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, A.J., Ridgeway, B., Gustilo-Ashby, A.M. et al. Efficacy of a standardized technique of trans-vaginal entry into the peritoneal cavity for post-hysterectomy vaginal vault suspension. Int Urogynecol J 19, 1393–1398 (2008). https://doi.org/10.1007/s00192-008-0642-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-008-0642-7