Abstract
Introduction and hypothesis
During vaginal hysterectomy, extraperitoneal uterosacral ligament suspension (ULS) bites can be taken before removing the uterus. We evaluated this modified extraperitoneal ULS for vault prolapse prevention.
Methods
Study period was 3.5 years. Fifty-one women with third- and fourth-degree prolapse were enrolled. An inverted V incision was made on the anterior vaginal wall and continued as a semicircular incision on the posterior vaginal wall. Lateral vaginal mucosa was pushed up to expose the cardinal–uterosacral ligament complex. The first ULS suture, using polypropylene no. 1, was taken in the upper-most exposed area of the uterosacral ligament. The second suture, using polyglactin no. 1 or 0, was taken 0.5–1 cm below the first suture. During placement of both sutures, traction on the cervix was maintained. The cardinal–uterosacral ligament complex was clamped, dissected, and ligated 1 cm below the second suture. Vaginal hysterectomy was completed. Ends of the ULS suture were fastened to the vault via vesicovaginal and rectovaginal septum using polypropylene within and polyglactin outside vaginal mucosa.
Results
Prolapse stage was 3 in 42 cases and 4 in nine. Duration of operation ranged from 60 to 120 min. Blood loss was 100–300 ml. During follow-up (average 2.3 years) four (8.3%), cases had stage 1 pelvic organ prolapse (POP), three were lost to follow-up, and 44 (91.6%) had no POP.
Conclusions
Using the cervix as a traction device is a good option when performing extraperitoneal ULS during vaginal hysterectomy to prevent vault prolapse.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vaginal surgical correction of pelvic organ prolapse (POP) using native tissue is minimally invasive [1]. Among the different native tissues used, uterosacral ligament suspension (ULS) is gaining popularity. There are two types of ULS: intraperitoneal and extraperitoneal. POP correction can done during vaginal hysterectomy and for posthysterectomy vault prolapse. Extraperitoneal ULS has less chance of ureteral injury. Dwyer and Fatton developed this technique [2]. We made minor modifications to their technique and performed this study.
Materials and methods
The study was conducted over 3.5 years (July 2014–Dec 2017). Women with third-and fourth-degree uterovaginal prolapse were included in the study; women medically unfit for surgery were excluded. Prolapse staging was done using the Pelvic Organ Prolapse Quantification (POP-Q) classification. A thorough general physical and systemic examination was done, as were routine preoperative investigations including ultrasonography of abdomen and pelvis. Informed consent was obtained from all patients. This study was in accordance with the institutional ethics committee.
Technique
An inverted V incision was made on the anterior vaginal wall, which was continued as a semicircular incision on the posterior vaginal wall. Vaginal mucosa was separated from the underlying structures. Laterally, the vaginal mucosa was separated from the underlying structures for ~3–4 cm on both sides. As a result, the uterosacral ligament got exposed for about 2–3 cm above its cervical attachment portion on both sides (Fig. 1). That means lower area of the intermediate part of uterosacral ligament was visible. A bite was taken through the upper-most exposed part of the ligament with a polypropylene suture no. 1 so that the suture went through the tissue of the intermediate part of the ligament; the ligament must not be encircled. Both ends of the suture were left long and held with curved, medium-sized artery forceps (first ULS suture) (Fig. 2). Approximately 0.5–1 cm below the previous suture, another bite was taken with polyglactin suture no. 1 or 0, and both ends were held with straight, medium-sized artery forceps (second ULS suture) (Fig. 3). The procedure was repeated on the other side. The cardinal–uterosacral ligament was clamped ~1 cm below the second ULS suture and ligated as usual for the vaginal hysterectomy. One end of this stump suture was brought outside the posterior vaginal mucosa at the angle of the vault, and the procedure performed on the other side. The vaginal hysterectomy was completed as usual.
During anterior colporrhaphy, the vesicovaginal septum was repaired. A bite was taken at the adjoining area of the lower part of the repaired septum using the upper end of the second suture, which was drawn completely through. The next bite was taken at the corresponding area of the anterior vaginal mucosa and drawn completely through; ends were held with artery forceps. Another bite was taken using the upper end of first suture at the adjoining area of the lower part of the repaired septum medial to the second bite and drawn completely through. The next bite was taken at the corresponding area of the anterior vaginal mucosa without drawing the needle completely through so the vaginal mucosa was not pierced; the end was held with artery forceps. The procedure was performed on the other side.
The lower end of the second suture was threaded through a free needle (either the upper or lower end of the suture can be used depending on which end is not already threaded through a needle). A bite was taken at the vault (rectovaginal septum) medial to the cardinal–uterosacral ligated vaginal hysterectomy suture, which was brought completely through the vaginal mucosa at the angle of the vault. The second suture was drawn completely through the posterior vaginal mucosa and the end held with straight medium-sized artery forceps. The next bite was taken at the vault by the remaining end of the first suture medial to the second suture. That bite incorporated the rectovaginal septum only, i.e., the posterior vaginal mucosa was not pierced (Fig. 4). This end was held with curved, medium-sized artery forceps and the procedure repeated on the other side.
The upper free end of the second uterosacral ligament suspension (USL) polyglactin suture was passed through the repaired vesicovaginal septum and brought through the anterior vaginal mucosa. The lower free end of the same suture was drawn through the posterior vaginal mucosa at the vault’s posterior lip, medial to the ligated uterosacral ligament suture of vaginal hysterectomy, which was also drawn completely through at the same angle. The free upper end of the first ULS suture (polypropylene) was passed through the repaired vesicovaginal septum superomedial to the second ULS suture and into the corresponding area of the anterior vaginal mucosa without drawing it through (piercing) the mucosa. The lower free end of the same suture was drawn into the rectovaginal septum and posterior vaginal mucosa at the vault’s posterior lip, just medial to the second ULS suture, again, without piercing the mucosa. Only one ULS suture on either side is shown for clarity
The anterior vaginal mucosa was closed to complete the anterior colporrhaphy. The free upper and lower ends of the left first ULS suture were tied together and the procedure repeated on the right, following which vault closure was begun. As a result, the nonabsorbable suture remained inside the vaginal mucosa. Upper and lower ends of the second suture were tied in the same way. Next vault was closed. Free ends of vault closing suture on lateral side were tied with the end suture of the ligated cardinal-utero-sacral ligament which was lying at the respective angle of the vault. The vault was thus well supported and placed high in the vagina (Figs. 5 and 6).
Cystoscopy could not be performed due to its unavailability. However, to avoid ureteral injury, bladder and ureters were held away from the operative field using a retractor anteriorly and pushing upward. Postoperatively, any complaint of pain and tenderness in the flank and back was carefully noted to determine the presence of ureteral injury.
Both uterosacral ligament suspension (ULS) sutures at the vault. The first suture lies medially. The upper end was drawn through the vesicovaginal septum but not through the vaginal mucosa. The lower end was drawn through the rectovaginal septum but, again, not through the vaginal mucosa. Upper and lower ends of the second ULS suture were both drawn outside the vaginal mucosa after taking a bite in vesicovaginal and rectovaginal septum, respectively
Result
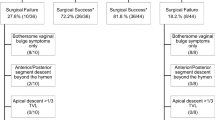
We performed 51 operations, all under spinal anesthesia. According to POP-Q classification, prolapses were stage 3–42 and 4–9 (Table 1). Surgery duration ranged from 60 to 120 min, and blood loss was 100–300 ml. Blood transfusion was given in one case. There was no bladder or ureteral injury, and postoperative recovery was uneventful. During follow-up (average 2.3 years), three patients were lost to follow-up, four had stage 1 vault prolapse (8.3%), and the remaining 44 (91.6%) were doing well without prolapse (stage 0). They are now on extended follow-up (Table 2).
Discussion
In the original description of the technique, extraperitoneal ULS was done to correct posthysterectomy vault prolapse [2]. Intraperitoneal ULS is performed both during hysterectomy and in posthysterectomy vault prolapse [3]. One to three permanent and/or delayed absorbable sutures are placed into the middle third of the uterosacral ligament bilaterally (permanent suture provides better anatomical support [1], and each end of these sutures is passed through the proximal transverse edge of the vesicovaginal septum and rectovaginal septum, recreating the pericervical ring and level 1 support [4]. There is a chance of ureteric support injury due to close proximity of uterosacral ligament and ureter, and this chance is greater during intraperitoneal ULS. Thus cystoscopy must be performed to rule out the possibility of ureteric injury following intraperitoneal ULS.
During extraperitoneal ULS, by placing the Landon retractor anteriorly, the ureter and bladder distanced from the operative field. ULS bites are taken on the lateral aspect of the ligament, i.e., opposite side of the ureteric relationship, meaning the chance of ureteric injury is almost nil. Hence, cystoscopy may not be needed in all cases. This is an advantageous situation, particularly where a cystoscope is unavailable. In our setup it was not available, thus we were unable to perform cystoscopy, and there was no postoperative complication.
During hysterectomy, re-establishing level 1 support using the uterosacral ligaments is crucial in decreasing the risk of posthysterectomy vault prolapse [2], which is why we performed extraperitoneal ULS during vaginal hysterectomy. As bilateral uterosacral ligaments are well exposed, ULS bites were taken before clamping the ligament for hysterectomy. We found it was easy to expose the high portion of the uterosacral ligament using the cervix as a traction device, greatly facilitating this part of the operation.
ULS allows fixing the vaginal vault high in the pelvis. New modifications in this technique using either the extraperitoneal or laparoscopic approach allow surgeons more freedom when planning surgery [5]. When performed for post-hysterectomy vault prolapse, prolapse recurrence was 4.6% over the 2-year follow-up; the global anatomical success rate was 85.5%, and urinary, bowel, and coital symptoms improved [6]. In the presence of dense pelvic adhesions, approaching the peritoneal sac at times become difficult. The extraperitoneal technique avoided this step, as the sac need not be opened. This technique carries less risk of ureteric injury, as ureters are retracted from the operative field [7].
Limitation of the study is the small number of participants, but the promising result encourages us to conduct larger studies.
In conclusion, vaginal hysterectomy with modified extraperitoneal ULS appears to have a low rate of posthysterectomy vault prolapse.
Abbreviations
- ULS:
-
Uterosacral ligament suspension
References
Chung CP, Miskimins R, Kuehl TJ, Yandell PM, Shull BL. Permanent suture used in uterosacral ligament suspension offers better anatomical support than delayed absorbable suture. Int Urogynecol J. 2012;23:223–7. https://doi.org/10.1007/s00192-011-1556-3.
Dwyer PL, Fatton B. Bilateral extraperitoneal uterosacral suspension: a new approach to correct posthysterectomy vaginal vault prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:283–92. https://doi.org/10.1007/s00192-007-0435-4.
Cvach K, Dwyer P. Surgical management of pelvic organ prolapse: abdominal and vaginal approaches. World J Urol. 2011. https://doi.org/10.1007/s00345-011-0776-y.
Shull BL, Bachofen C, Coates KW, Kuehl TJ. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol. 2000;183:1365–73; discussion 1373-4. https://doi.org/10.1067/mob.2000.110910.
Yazdany T, Bhatia N. Uterosacral ligament vaginal vault suspension: anatomy, outcome and surgical considerations. Curr Opin Obstet Gynecol. 2008;20:484–8. https://doi.org/10.1097/GCO.0b013e32830eb8c6.
Fatton B, Dwyer PL, Achtari C, Tan PK. Bilateral extraperitoneal uterosacral vaginal vault suspension: a 2-year follow-up longitudinal case series of 123 patients. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:427–34. https://doi.org/10.1007/s00192-008-0791-8.
Ow LL, Walsh CE, Rajamaheswari N, Dwyer PL. Technique of extraperitoneal uterosacral ligament suspension for apical suspension. Int Urogynecol J. 2016;27:637–9. https://doi.org/10.1007/s00192-015-2873-8.
Acknowledgements
We express our heartfelt thanks to Dr. Ranita Roy Chowdhury, Assistant Professor, Dr. Srijoni Chowdhury, Clinical Tutor, and other members of the unit for helping conduct this study.
Author information
Authors and Affiliations
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Pal, M., Bandyopadhyay, S. Modified extraperitoneal uterosacral ligament suspension for prevention of vault prolapse after vaginal hysterectomy. Int Urogynecol J 30, 633–637 (2019). https://doi.org/10.1007/s00192-018-3669-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3669-4