Abstract
The biomechanical properties of the puborectalis muscle are likely to be important for pelvic organ support. However, neither elasticity nor its clinical correlate, muscle resting tone, have received much attention to date. We therefore conducted a prospective study to test a newly developed resting tone scale for validity and reproducibility. Ninety-eight patients underwent a physical examination including prolapse staging and palpation of the levator ani. They were also assessed by 4D translabial ultrasound for levator hiatal dimensions and prolapse assessment. Resting tone was negatively associated with anterior and posterior compartment prolapse. An independent test–retest series yielded a weighted kappa of 0.55 (CI 0.44–0.66), implying “moderate” repeatability. Resting tone of the puborectalis muscle can be determined by digital palpation. It is moderately repeatable and associated with pelvic organ prolapse. Palpation of resting tone may be a useful new tool for assessing women with pelvic floor dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The biomechanical properties of the puborectalis muscle are likely to be important for pelvic organ support and in childbirth. There is evidence that levator hiatal dimensions on Valsalva are associated with progress in the second stage of labor [1]. The fact that levator trauma is more common in older primiparae [2–4] points towards biomechanical factors as a determinant of levator trauma, which seems to be an etiological factor for female pelvic organ prolapse [5]. There is a clear association between levator hiatal dimensions and pelvic organ descent [6, 7]. Part of this relationship may be due to delivery-related levator trauma [3, 6, 8], but it is likely that distensibility or elasticity of the levator hiatus is also an independent etiological factor for female pelvic organ prolapse since the relationship is also observed in nulliparous women [9]. Consequently, there is a need to develop methods for assessing biomechanical properties of the puborectalis muscle as this may help in risk stratification for women approaching parturition and in the assessment of women complaining of urinary incontinence and/or prolapse. A reliable method would be particularly valuable for determining the relative efficacy of interventions.
The most basic method of assessing the biomechanical properties of any material is digital palpation, and the levator ani muscle lends itself to such an assessment. Muscle resting tone can be clinically defined as compliance on palpatory compression, or resistance to passive stretch or distension [10]. It can therefore be assessed during a normal vaginal examination with minimal effort and at no additional cost and is associated with very limited inconvenience to the patient. In this study, we test a six-grade scale for resting tone, analogous to the Oxford grading scale used for assessing contractility, for repeatability and validity. As we allowed half-grades and as findings were documented separately for right and left, this gave us the opportunity to test six-point, 11-point, and 21-point scales for repeatability.
To date, digital assessment of the levator ani muscle or its most prominent component, the puborectalis muscle, has been limited to a semiquantitative evaluation of function, using the modified Oxford grading first proposed by Laycock in the late 1980s [11]. This form of assessment correlates moderately with contraction “strength” as measured by a perineometer and also with lifting function as determined by ultrasound [12, 13]. Repeatability is reasonable [14, 15], although some experts hold that Oxford grading is insufficiently reproducible for research applications [16] and have suggested a four-point scale of “absent”, “weak”, “normal”, and “strong” contractile effort.
The authors have found only one study in the world literature (Medline search March 26, 2008) that has attempted to quantify resting tone of pelvic floor muscles, without validating the concept against clinical or other diagnostic parameters. Tone was graded as abnormally low, normal, or high, with only two patients rated as “hypertonic” [17]. Validation is a difficult issue as there is, to our knowledge, currently no commercially available elastometer for intravaginal use, although such devices are very likely to be available in the near future (J. Kruger, Auckland, personal communication). As a consequence, the only potential measure of validation is distensibility of the levator hiatus, which can be obtained noninvasively by translabial ultrasound imaging. A recent attempt at determining a component of elasticity, strain, showed a weak but significant association between distension of the hiatus during valsalva and resting tone (r = −0.224, P = 0.033) [18], but strain alone is clearly not a sufficient measure of elasticity since it is likely to be confounded by reflex activation of the levator ani muscle [19]. For the time being, palpation may be the only way of determining a correlate of muscle elasticity, which is why we decided to test the validity and reproducibility of the digital assessment of muscle resting tone.
Materials and methods
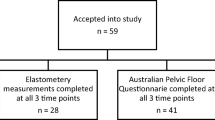
Ninety-eight consecutive patients referred with symptoms of lower urinary tract dysfunction and/or prolapse were investigated in a tertiary urogynecological unit. All patients underwent a physical examination, which included ICS POP-Q staging [20], vaginal digital palpation for modified Oxford grade [1], levator trauma, and puborectalis muscle resting tone grade as shown in Table 1, with increments between grades assumed to be notionally equal. Patients were in a modified lithotomy position, with knees bent and feet placed comfortably apart. Palpation was performed using one finger that was placed on the medial aspect of the puborectalis muscle, just anterior to the anorectal junction, at about 4–5 o’clock position using a clockface notation. MOS grades 1 and 2 did not require any lifting effect.
If one were to palpate muscle resting tone immediately after finger insertion, results would likely be confounded both by muscle activation due to a defensive reflex and possibly by thixotropy. Thixotropy is a viscoelastic property of skeletal muscle that results in tissue stiffening, i.e., a reduction in compliance, during periods of inactivity [21]. The assessment was therefore carried out after asking the patient to contract and then relax the (frequently contracted) muscle. In order to achieve relaxation and in order to overcome thixotropy, the muscle was then passively distended several times before assessment of resting tone, slowly in order to avoid reflex muscle contraction. Figure 1 illustrates the placement of the palpating finger.
As we obtained half-grades (e.g., three to four) and assessed both sides separately (resulting in a 21-point scale), we gained the opportunity to test (averaged) six- and 11-point scales as well as the original 21-point scale. The six- and 11-point scales were obtained from the 21-point scale by rounding. To give an example, if a patient had a score of 3.5 on the right and 3 on the left, then those were averaged to 3.25 (global 21-point scale) and rounded to 3.5 (global 11 point scale) and 3 (global six-point scale). This was undertaken both for the Modified Oxford Scale (MOS) and for resting tone grade.
Patients also underwent 4D translabial ultrasound imaging for levator hiatal dimensions and prolapse assessment as previously described [9]. We were therefore able to validate our resting tone scale against (a) clinical prolapse stage, (b) sonographically determined pelvic organ descent, and (c) levator hiatal dimensions. Volume datasets were obtained with the patient supine and after bladder emptying, at rest, on maximal Valsalva, and on maximal pelvic floor muscle contraction, the latter two after biofeedback teaching to ensure optimal performance of maneuvers. Measurements of hiatal dimensions were undertaken using post-processing software (GE Kretz 4D View v 5.0), with levator hiatal dimensions determined in the axial plane of minimal dimensions. This plane is identified in the midsagittal plane by locating the minimal distance between the posteroinferior surface of the symphysis pubis and the anterior surface of the puborectalis loop behind the anorectal junction [9]. These parameters have been shown to be highly reproducible [9, 22, 23] by the authors and others.
After completion of this study, the two authors performed a blinded interrater test–retest series for resting tone and Oxford Grading, using the same methodology for digital assessment. The assessment by the second operator was performed within 15 min of the first examination, with the record of the first palpation inaccessible to the second examiner. However, neither examiner was blinded to prolapse status or symptoms.
This study was conducted in the context of a parent project that had been approved by the local institutional Human Research Ethics Committee. Statistical analysis was undertaken using SAS (version 9, SAS Institute, Cary, NC, USA) and Minitab (v 13 (Minitab, State College, PA, USA). After normality testing (Kolmogorov–Smirnov analysis), we tested repeatability with weighted kappa (Fleiss–Cohen weights). Associations between MOS and resting tone scales on the one hand and continuous parameters of pelvic organ descent and levator hiatal morphometry and function on the other hand were tested by ANOVA. This was performed for all six-point, 11-point, and 21-point scales separately in order to gain insight into the relative discriminatory ability of the different scales. P < 0.05 was regarded as statistically significant.
Results
The mean age of patients was 54.7 (range 19–86). Median vaginal parity was 2 (range 0–8). Thirty-two patients had had a previous hysterectomy, and eight reported previous incontinence or prolapse surgery. They suffered from symptoms of stress incontinence (68%), urge incontinence (70%), frequency (62%), nocturia (62%), and symptoms of prolapse (40%). On clinical examination, 35 women showed pelvic organ prolapse of stage 2 or higher. On ultrasound assessment, the levator hiatal area at rest was 18.9 cm2 (SD 5, range 9.2 to 35.7); on Valsalva, it reached an average of 27.3 cm2 (SD 8.9, range 9.9–50.4). On pelvic floor contraction, the hiatal area was reduced to 15.4 cm2 (SD 3.8, range 6.96–27.23).
Modified Oxford grading and resting tone were determined separately for the right and left puborectalis muscle, resulting in 196 assessments. Mean Oxford grading was 2.6 (range 0–4.5) and mean resting tone was 2.8 (range 1–4.5), with both parameters normally distributed. Reduced resting tone on palpation was associated with cystocele, and this association was significant both for the six- (P = 0.019) and 21-point scale (P = 0.04), while it did not quite reach significance for the 11-point scale (P = 0.074). For posterior compartment descent, similar associations were found, with P values ranging from 0.046 (six-point scale) and 0.048 (11-point scale) to 0.032 (21-point scale) (see Table 2). Figure 2 shows ANOVA graphs of the relationship between muscle resting tone and ultrasound quantification of bladder and rectal descent.
Relationship between resting tone determined by vaginal palpation and descent of the bladder (top) and rectal ampulla (bottom) as quantified on translabial ultrasound on maximal Valsalva, in millimeters relative to the inferior margin of the symphysis pubis (F = 1.55, p = 0.195 for cystocele; F = 3.28, P = 0.015 for rectocele on ANOVA), n = 98 for cystocele and n = 96 for rectocele
Conversely, none of the Oxford grading scales was significantly associated with clinical prolapse grading, although this may be a power issue due to the limited size of the series. With regard to levator hiatal dimensions, resting tone again showed significant associations, with the 11-point scale performing best (see Table 3). Oxford grading was associated only with hiatal dimensions on pelvic floor muscle contraction, but not with hiatal dimensions at rest or on Valsalva. Overall, there were no major differences in discriminatory ability when comparing six-, 11-, and 21-point scales against each other.
In a separate blinded test–retest series on 107 patients, we obtained weighted kappas (Fleiss–Cohen weights) of 0.80 for a six-point MOS (CI 0.75–0.85), of 0.80 (CI 0.75–0.85) for an 11-point MOS, and 0.82 (CI 0.76–0.88) for a 21-point MOS. For resting tone, the respective figures were 0.42 for the six-point scale, 0.50 for the 11-point, and 0.55 (CI 0.44–0.66) for the 21-point scale (see Table 4). This implies “moderate” agreement for resting tone, as opposed to “excellent” agreement for Oxford grading. An increase in the number of categories did result in improved repeatability when it was measured by weighted kappa (see Table 4).
Discussion
Resting tone of the levator ani muscle can be determined by digital palpation. We have developed a grading system analogous to the MOS that is in widespread use for assessment of muscle function. The method seems less repeatable than the MOS, the repeatability of which in our study is consistent with literature data. Interestingly and despite the limitation of poorer repeatability, resting tone seems to be more strongly associated with pelvic organ prolapse than Oxford grading. While the scale described in this study may not be the optimal scale to use, any alternative would have to demonstrate better repeatability or validity.
There has been some discussion regarding the use of different scales for the assessment of pelvic floor function, with some holding that a six-point scale for MOS is insufficiently repeatable and that it may be preferable to use a four-point scale in the interests of reliability [16]. Interestingly, we found that, in our hands, repeatability was highest for a 21-point scale, both for MOS and resting tone, although confidence intervals overlapped widely. The weighted kappa for our 21-point Modified Oxford Scale reached 0.82 (CI 0.76–0.88) which is excellent. For resting tone, the optimal repeatability was 0.55 (CI 0.44–0.66), and this was again reached by the 21-point scale. It may therefore be deducted that a reduction in categories is inappropriate when palpation for levator strength or resting tone is undertaken by trained operators, as it is unlikely to result in improved repeatability.
The main attraction of a scale that includes a larger number of distinct categories is increased discriminatory ability. However, when we tested different scales against clinical prolapse grade and levator hiatal dimensions on ultrasound in an attempt to validate the new measure of “resting tone” and compare discriminatory power of different scales, we found only minor differences in the performance of six-, 11-, and 21-point scales. We therefore conclude that, while repeatability may be slightly higher for 11- and 21-point scales, there is little to choose between the scales when it comes to discriminatory ability. Consequently, the selection of scales should be left to the individual clinician or researcher.
The main weakness of any assessment of muscle tone is that “resting tone” is influenced by activation state, which may only be partly under conscious control. Clearly, it would be inappropriate to assess resting tone immediately after insertion of a finger for palpation since voluntary or involuntary activation of the levator ani would result in an artificially high tone. The viscoelastic properties of the muscle may also be influenced by stiffening during periods of inactivity (thixotropy) [21]. We therefore asked the patient to contract and relax the muscle and help achieve relaxation by slowly and gently stretching the muscle digitally, enabling the patient to distinguish varying grades of muscle activation. However, it is recognized that several different factors (not the least any psychological stress induced by the assessment itself) may act as confounders.
With regard to the scale used in this study, we are certain that it could be improved upon. The inclusion of pain may be questionable since many other conditions such as scarring or endometriosis could be responsible for pain, although very high “resting tone”, i.e., muscle spasm, would certainly be expected to be associated with pain. Others may debate the use of descriptors of hiatal width in a scale of resting tone since hiatal dimensions are confounded by other factors, e.g., muscle mass, muscle trauma such as avulsion, or simply personal biometric indices. Another issue is “normality”: What is “normal” resting tone, and what are the limits of normality? These issues will require clarification by a study of resting tone in normal, asymptomatic women.
Despite such limitations, it appears that palpation of levator ani resting tone is moderately repeatable. Resting tone is associated with pelvic organ prolapse and the dimensions of the levator hiatus. It clearly describes a hitherto inaccessible component of the biomechanical properties of the pelvic floor. Palpation of resting tone may be a useful new tool for assessing women with pelvic floor dysfunction, in particular, in the context of intervention studies aimed at altering pelvic floor biomechanical properties. Resting tone may be more important in the etiology of pelvic organ prolapse than muscle strength. Consequently, it may be preferable to focus on this parameter rather than contraction strength as a measure of muscle function and quality, especially in patients with pelvic organ prolapse. In the future, it is hoped that objective measures of pelvic floor muscle elasticity can be developed, both for research and clinical use, as such objective measures are likely to be more repeatable than palpation.
Abbreviations
- ICS POP-Q:
-
International Continence Society Pelvic Organ Prolapse Quantification
- MOS:
-
Modified Oxford Scale
- ANOVA:
-
Analysis of variance
- PFMC:
-
Pelvic floor muscle contraction
References
Lanzarone V, Dietz H (2007) Three-dimensional ultrasound imaging of the levator hiatus in late pregnancy and associations with delivery outcomes. Aust NZ J Obstet Gynaecol 47:176–180
Dietz H (2007) Does delayed childbearing increase the risk of levator injury in labour? Aust NZ J Obstet Gynaecol 47:491–495
Dietz HP, Lanzarone V (2005) Levator trauma after vaginal delivery. Obstet Gynecol 106:707–712
Kearney R, Miller J, Ashton-Miller J, Delancey J (2006) Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol 107:144–149
Dietz H, Simpson J (2008) Levator trauma is associated with pelvic organ prolapse. Br J Obstet Gynaecol 115:979–984
Dietz HP, Steensma AB (2006) The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG: Int J Obstet Gynaecol 113:225–230
Dietz H, De Leon J, Shek K (2008) Ballooning of the levator hiatus. Ultrasound Obstet Gynecol 31(6):676–680
Dietz H (2007) Quantification of major morphological abnormalities of the levator ani. Ultrasound Obstet Gynecol 29:329–334
Dietz H, Shek K, Clarke B (2005) Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol 25:580–585
Simons D, Mense S (1998) Understanding and measurement of muscle tone as related to clinical muscle pain. Pain 75:1–17
Laycock J (1992) Assessment and treatment of pelvic floor dysfunction. Ph.D thesis, University of Bradford, Bradford
Dietz HP, Jarvis SK, Vancaillie TG (2002) The assessment of levator muscle strength: a validation of three ultrasound techniques. Int Urogynecol J 13:156–159
Thompson JA, O’Sullivan PB, Briffa K, Neumann P, Court S (2005) Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. Int Urogynecol J 16:285–292
Neumann P, Grimmer-Somers K, Gill V, Grant R (2007) Rater reliability of pelvic floor muscle strength. Aust NZ Continence J 13:8–14
Frawley H (2006) Reliability of pelvic floor muscle strength assessment using different test positions and tools. Neurourol Urodyn 25:236–242
Messelink B, Benson T, Berghmans B et al (2005) Standardization of terminology of pelvic floor muscle function and dysfunction: report from the Pelvic Floor Clinical Assessment Group of the International Continence Society. Neurourol Urodyn 24:374–380
Devreese AM, Staes F, De Weerdt W et al (2004) Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn 23:190–197
Thyer I, Shek C, Dietz HP (2007) Clinical validation of a new imaging method for assessing pelvic floor biomechanics. Ultrasound Obstet Gynecol 31:201–205
Oerno A, Dietz H (2007) Levator co-activation is a significant confounder of pelvic organ descent on Valsalva maneuver. Ultrasound Obstet Gynecol 30:346–350
Bump RC, Mattiasson A, Bo K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Walsh E (1992) Muscles, masses and motion. Mac Keith, London, UK
Guaderrama N, Liu J, Nager C et al (2006) Evidence for the innervation of pelvic floor muscles by the pudendal nerve. Obstet Gynecol 106:774–781
Yang J, Yang S, Huang W (2006) Biometry of the pubovisceral muscle and levator hiatus in nulliparous Chinese women. Ultrsound Obstet Gynecol 26:710–716
Acknowledgements
This study was supported, in part, by the Betty Byrne Henderson Foundation, University of Queensland, Brisbane, Queensland, Australia, and by OZWAC (Australian Women and Children Research Foundation), Penrith, Australia.
Conflicts of interest
Hans Peter Dietz has received support in the form of loan equipment from ultrasound equipment manufacturers (GE Kretz, Toshiba, Bruel&Kjaer, and Phillips) and has received speakers’ honoraria from AMS, GE, and Astellas. He has acted as consultant for AMS and CCS.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dietz, H.P., Shek, K.L. The quantification of levator muscle resting tone by digital assessment. Int Urogynecol J 19, 1489–1493 (2008). https://doi.org/10.1007/s00192-008-0682-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-008-0682-z