Abstract
To estimate the accuracy of clinical examination and the indications for defecography in patients with primary posterior wall prolapse. Fifty-nine patients with primary pelvic organ prolapse were evaluated with a questionnaire, clinical examination and defecography. Defecography was used as reference standard. There was no relation between bowel complaints and posterior wall prolapse evaluated by clinical examination (p = 0.33), nor between bowel complaints and rectocele (p = 0.19) or enterocele (p = 0.99) assessed by defecography. The diagnostic accuracy of clinical examination in diagnosing rectocele was 0.42, sensitivity was 1.0 and specificity was 0.23. The diagnostic accuracy of clinical examination in diagnosing enterocele was 0.73, with a sensitivity of 0.07 and a specificity of 0.95. Clinical examination is not accurate to assess anatomic defects of the posterior vaginal wall. Defecography is recommended as a helpful diagnostic tool in the work-up of patients with posterior vaginal wall prolapse if surgical repair is considered.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Constipation, incomplete rectal emptying, the need for manual assistance, excessive straining and fecal incontinence are often associated with pelvic organ prolapse (POP), i.e. posterior vaginal wall prolapse [1]. Accurate assessment of posterior compartment defects is essential in selecting the optimal (surgical) therapy. Missing of concealed defects like intussusception or enterocele can result in a disappointing treatment outcome. Additional diagnostic tests can be initiated to support clinical decision making. One of the diagnostic options is defecography [2, 3]. The aim of defecography is to evaluate the anatomy (rectocele, enterocele and intussusception) as well as the function (contraction and relaxation of the puborectalis muscle, poor rectal emptying or trapping) of the anorectum [4]. The role of defecography in the work-up of POP is not clear. Often defecography is performed at random in case of defecatory disorders or in case defects of the posterior compartment are suspected.
The aim of this study is to estimate the diagnostic accuracy of the clinical examination compared to defecography in cases of primary POP. The following two questions were researched. Firstly, are defecation problems related to posterior wall prolapse and/or grade of rectocele and enterocele? Secondly, what is the diagnostic accuracy of clinical examination in detecting rectoceles and enteroceles, with defecography as reference standard?
Materials and methods
Between January 2000 and January 2002, all women referred to the gynecology outpatient clinic of the Onze Lieve Vrouwe Hospital (OLV Hospital) with suspected primary POP were invited to participate in a study evaluating the diagnostics of POP. Defecography was performed as part of this study. Included were women who experienced a sagging sensation and/or micturition and defecation problems at least once a week, and in whom one of the compartments was at least stage I prolapse according to the Pelvic Organ Prolapse-Quantification (POP-Q) classification system [5]. Exclusion criteria were: gynecological pathology additional to the prolapse or previous prolapse surgery and/or hysterectomy. We enrolled 68 patient in the study; five patients dropped out (the extra diagnostic tests were too burdensome) and in four patients, defecography was not correctly carried out or read. The study was approved by the Medical Ethics Board of the OLV Hospital.
We conducted a prospective (non-randomised) cohort study. The required examinations for the study were carried out during two outpatient visits. During the first visit at the gynecology outpatient clinic of the OLV Hospital, patient’s characteristics and symptoms were recorded by standard history taking.
Defecation symptoms and impact on daily life were additionally measured with the Defecation Distress Inventory (DDI), a Dutch-validated disease-specific questionnaire analogue to the Urinary Distress Inventory (UDI) and the Colorectal-anal Distress Inventory (CRADI) [6–8].
The DDI consists of 15 items grouped to four domains: constipation defecation, fecal incontinence, painful defecation and incontinence for gas. The scores of each of the DDI domains range from 0–100, a higher score indicates more burden of symptoms or unfavorable impact on daily functioning. The 15 questions were developed after studying the literature and international definitions, interviewing patients who presented with constipation or fecal incontinence and by interviewing three experts in the field from the Department of Surgery and Department of Obstetrics and Gynecology from the University Medical Center Utrecht, The Netherlands. Eventually, a structured interview of the 15 selected items was held with 20 female patients.
The prolapse was assessed according to the POP-Q by the first author (A.G.G.). A critical parameter of the POP-Q system in our study was point Bp, quantifying the severity of the posterior vaginal wall prolapse. The presence of an enterocele was assessed by digital rectal–vaginal examination. Following Bump (ICS), we use the terms posterior vaginal wall prolapse for bulging of the posterior vaginal wall assessed by clinical examination and rectocele for bulging of the anterior rectum wall diagnosed by defecography [5].
During the second outpatient visit, defecography was carried out in all participating patients at the Department of Radiology of the OLV Hospital. Defecography was carried out according to a predefined protocol. Bowel preparation consisted of coating the small bowels with stomach porridge (barium sulfate suspension diluted in water-micropaque, Guerbet) 2 h before the examination. Before the start of the procedure patients were advised to go to the toilet in order to prevent a full bladder during defecography recording. At the onset of the examination barium sulfate (maximal 350 ml) mixed with two sachets Volcolon was inserted in the colon. The vagina was marked with 30 ml amidotrizoicacid gel solution. A chain with radio-opaque small bullets was inserted between the anal cleft, delineating the pelvic floor. The patient was seated on an artificial toilet with a water filled motor scooter tube on top of it. The toilet was constructed against a vertical X-ray table. Assessment of the anatomy and position of small bowels, anorectum and pelvic floor was made at rest, during contraction of the pelvic floor muscles, weak straining and forceful straining. Finally the patient was allowed to defecate so that the function of anorectum and pelvic floor could also be examined. X-ray films were taken and the whole process was recorded on videotape. All images were evaluated by one radiologist [VPvdH]. The radiologist was blinded for the findings of clinical examination.
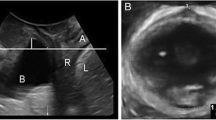
Primary outcome of defecography was the grade of rectocele and enterocele, respectively. Rectocele was quantified by determination of the distance between the most ventral part of the anterior rectal wall and the expected rectal lining. Enterocele was defined as a widening between the vagina and anterior rectal wall with herniation of the small bowels. Rectocele and enterocele were classified according to the grading system proposed by Wiersma [9]. Rectocele grade 0: no rectocele; grade I: rectocele < 2 cm; grade II: rectocele ≥ 2 cm and <4 cm; grade III: rectocele ≥ 4 cm. (Fig. 1). We considered a rectocele < grade 2 (smaller than 2 cm) as a physiologic condition [10].
Grading system for rectocele. Grade 0: no rectocele. Grade I: rectocele < 2 cm. Grade II: 2 cm ≤ rectocele < 4 cm. Grade III: rectocele ≥ 4 cm. Reproduced with permission from [9]
Enterocele grade 0: normal situation; grade I: herniation of the small bowels reaching to the distant half of the vagina and partial or complete reduction of the rectal lumen; grade II: small bowels reaching down to the perineum; grade III: herniation of the small bowels protruding out of the anal canal (Fig. 2a,b and c).
a–c Grading system for enterocele. a Enterocele grade I. b Enterocele grade II. c Enterocele grade III. Reproduced with permission from [9]
Due to lack of studies on defecography outcome in POP, a formal sample size could not be calculated. Instead, we adopted a convenience sample of 59 patients with primary POP. The prevalence and burden of bowel symptoms and DDI were presented with conventional descriptive statistics.
Diagnostic accuracy of the clinical examination in the assessment of posterior wall prolapse was evaluated in terms of proportion of correct test results, sensitivity, specificity, positive predicted value (PV+) and negative predicted value (PV−), using the outcome at defecography as reference standard. The relation between the burden of defecation disorders as measured by the DDI domains, and the presence of posterior wall prolapse, rectocele and enterocele were evaluated with the non-parametric Mann Whitney U Test. SPSS 15.0 for Windows was used for data management and statistical analysis. A p value < 0.05 (two sided) was considered statistically significant.
Results
Table 1 shows the patient’s characteristics, the overall POP-Q stages and the stages of point Bp. The majority of patients had an overall POP-Q stage III (n = 40, 68%) and a posterior wall prolapse stage II (n = 38, 64%).
Table 2 displays the prevalence and impact of bowel symptoms on daily life. Incontinence for gas (36/59 (0.61)) is the most prevalent and most bothersome complaint followed by a feeling of incomplete evacuation (27/59 (0.46)). Other frequent occurring complaints were false urge (24/59 (0.41)) and obstructed defecation (20/59 (0.34)).
Tables 3, 4 and 5 shows the relation between constipation, painful defecation, fecal incontinence and flatus incontinence, and the presence of defects of the posterior compartment assessed by clinical examination and by defecography. No significant relation between defecation disorders and the presence of posterior wall prolapse, rectocele or enterocele was observed.
Tables 6 and 7 show the outcome of posterior wall prolapse (stage ≥ 2) and enterocele as determined at clinical examination, in relation to rectocele (grade ≥ 2) and enterocele at defecography. Defecography revealed 15 rectoceles; no rectoceles were missed by clinical examination (sensitivity: 15/15 (1.0), 95%CI: [0.82–1.00]). In 34 patients, posterior wall prolapse (stage ≥ 2) was diagnosed clinically, but defecography revealed no rectocele of grade II or higher (false positives; specificity: 10/44 (0.23), 95%CI: [0.11–0.38]). The proportion of correct test results was 25/59 (0.42), 95%CI: [0.30–0.56]. PV+ was 15/49 (0.31), 95% CI: [0.18–0.45] and PV− was 10/10 (1.0), 95% CI: [0.74–1.00].
Table 7 shows that defecography revealed 15 enteroceles of which one was correctly diagnosed (sensitivity: 1/15 (0.07), 95%CI: [0.002–0.32] while 14 enteroceles were missed by clinical examination (false negative rate: 14/15). Specificity was 42/44 (0.95), 95%CI: [0.85–0.99]). No enterocele was diagnosed in 44 patients of which two were diagnosed at the clinical examination (false positive rate: 2/44).The proportion of correct test results was 43/59 (0.73), 95%CI: [0.60–0.84]), PV+ was 1/3 (0.33), 95%CI: [0.008–0.91]) and PV− was 42/56 (0.75), 95%CI: [0.62–0.86].
Discussion
In our study no relation was found between the impact of constipation, painful defecation, fecal incontinence and flatus incontinence on daily life on the one hand and the stage of posterior wall prolapse or the grade of rectocele on the other. Posterior wall prolapse stage II or higher was prevalent in 83% (n = 49) at clinical examination. The prevalence of rectocele grade II or higher, as diagnosed by defecography, was 25% (n = 15). While the sensitivity of diagnosing rectocele by clinical examination was excellent (1.0), specificity was poor (0.23); 44 patients had no rectocele but in only ten cases did clinical examination predict correctly.
Enterocele was incorrectly classified by clinical examination in 16/59 (0.27) patients, largely due to the large false negative rate; the clinical examination missed 14 out of 15 enteroceles, indicating extremely low sensitivity (0.07). However, the specificity of clinical examination was high (0.95).
There are several possible explanations for the discordant results between clinical examination and defecography. Firstly, measurement of the posterior wall prolapse may have been inaccurate, although measurements were done by one experienced physician according to the standardised POP-Q system. Besides, the number of posterior wall prolapses can be overestimated by mistaking enteroceles for rectoceles (five enteroceles were missed in 34 patients (0.12) with posterior wall prolapse ≥ stage 2 and rectocele < grade II). Secondly, in spite of a standard protocol for defecography, inaccurate assessment of the rectocele by the radiologist must be considered. The interobserver agreement for posterior wall prolapse represented by point Bp of POP-Q system varies between moderate (r s 0.53) and good (r s 0.75) [11, 12]. A recent study of Dobben et al. indicates good interobserver agreement for enterocele and anterior rectocele (weighted К = 0.64, 95%CI: [0.41–0.87] and weighted К = 0.72; 95%CI: [0.61–083], respectively) [13]. A third explanation is that relaxation of the vaginal wall does not necessarily go together with bulging of anterior rectal wall, implying that posterior wall prolapse and rectocele are different anatomic disorders and not synonyms for the same condition [14]. Finally, vaginal wall morphology can be influenced by muscularis hypertrophy, rugae and obstetric lacerations [15].
Only a few studies have examined the association between clinical findings and intra-operative or radiological findings. The study of Burrows et al. largely support our findings: they concluded that the diagnostic accuracy of clinical examination is poor and the predictive value of clinical evaluation for all defects was less than 40% [16]. To our knowledge, only two studies have examined the relation between posterior wall prolapse (POP-Q point Bp) and rectocele [17, 18]. They concluded that POP-Q staging neither predicts radiological size nor visceral involvement in posterior wall prolapse.
Kelvin et al. studied the contribution of defecography to the evaluation of pelvic organ prolapse, he also found that enteroceles were frequently missed at physical examination [19].
Many studies did not find a relation between defecatory symptoms and the grade of rectocele [20]. Since many of these symptoms also occur in women without POP [21], defecatory symptoms may be non-specific for POP. The question if defecation disorders are the result of POP, the cause of POP or co-incidental, remains unanswered [22].
Our results are in agreement with previous research which indicates that there is no relation between defecation disorders and posterior wall prolapse (evaluated by POP-Q) or rectocele (assessed by defecography). If true, the consequences are far reaching: no benefit can be expected by surgical correction of these anatomic disorders.
Our study contains some limitations. Possibly, the power of our study is low given the relatively small study group. Ex post sample size calculation, based on our study results, shows that at least 79 patients (posterior wall prolapse) and 38 patients (enterocele) were needed to reject the null hypothesis that the diagnostic accuracy of posterior wall prolapse and enterocele, respectively, compared to the outcome of defecography which is not equivalent (equivalence limit difference of 25%; alpha = 0.05; 1-beta-0.90).
The small number of severe prolapses of the posterior compartment may be due to the rather homogeneous composition of our patient group, that largely consisted of patients with mild to moderately severe primary pelvic organ prolapse with only few higher posterior wall prolapse stages. In patients with recurrent pelvic organ prolapse, severe posterior wall prolapse appears more prevalent [23]. Our study does not allow any definite statements about a possible relation between disordered defecation and severe stages of posterior wall prolapses. Finally, can we use defecography as gold standard? In spite of the fact that the number of reproducibility studies with good interobserver agreement are limited, the diagnostic and therapeutic significance of defecography has proved to be high in patients with defecation disorders [24]. Therefore, defecography can be regarded the best available diagnostic test for evaluation of the anorectum [25].
The advantage of improved preoperative diagnosis needs to be balanced against the inconvenience of the patient as well as the extra medical costs. Roovers et al. commented on the invasive and embarrassing character of defecography. They developed a prognostic model which can predict the presence of abnormal defecography [26].
We found no relation between defecation disorders (evaluated by a validated questionnaire) and posterior wall prolapse (evaluated by POP-Q) or rectocele (assessed by defecography), i.e. symptoms reported on a validated questionnaire may not correspond with physical examination findings. Assuming that posterior wall prolapse and rectocele can be considered the same anatomic entity, clinical examination is not accurate in diagnosing anatomical defects of posterior vaginal wall and enteroceles, compared to defecography as reference standard. Clinical examination overestimates the presence of the posterior wall defects (large false positive rate) but misses enterocele in patients with primary POP (large false negative rate). Furthermore, clinical examination is an inadequate technique for diagnosing other structural anomalies of the anorectum like rectal intussusception and rectal prolapse. We recommend defecography as helpful diagnostic tool in the work-up of patients with posterior wall prolapse, especially when surgical treatment is considered.
References
Digesu GA, Chaliha C, Salvatores S, Hutchings A, Khullar V (2005) The relationship of vaginal prolapse severity to symptoms and quality of life. BJOG 112:971–976
Segal JL, Karram MM (2002) Evaluation and management of rectoceles. Curr Opin Urol 12:345–352
Kenton K, Shott S, Brubaker L (1999) The anatomic and functional variability of rectoceles in women. Int Urogynecol J 10:96–99
Wiersma TG, Mulder CJ, Reeder JW, Tytgat GN, Van Waes PF (1994) Dynamic rectal examination (defecography). Baillieres Clin Gastroenterol 8:729–741
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Van Brummen HJ, Bruinse HW, Van de Pol G, Heintz AP, van der Vaart CH (2006) Defecatory symptoms during and after the first pregnancy: prevalences and associated factors. Int Urogynecol J 17:224–230
Van der Vaart CH, De Leeuw JR, Roovers JP, Heintz AP (2003) Measuring health related quality of life in women with urogenital dysfunction: the urogenital distress inventory and incontinence impact. Neurourol Urodyn 22:97–104
Bradley CS, Nygaard IE, Brown MB, Gutman RE, Kenton KS, Whitehead WE, Goode PS, Wren PA, Ghetti C, Weber AM (2007) Bowel symptoms in women 1 year after sacrocolpopexy. Pelvic Floor Disorders Network Am J Obstet Gynecol 197:642.e1–642.e8
Wiersma TG (1994) Dynamic Rectal Examination. Clinico-Radiologic Correlation. Thesis. ISBN 90-801844-2-X
Shorvon PJ, McHughes S, Diameant NE, Somers S, Stevenson GW (1989) Defecography in normal volunteers. Gut 30:1737–1749
Groenendijk AG, de Blok S, Birnie E, Bonsel GJ (2005) Interobserver agreement and intersystem comparison of the halfway system of Baden and Walker versus the POP-Q prolapse classification system in assessing the severity of pelvic organ prolapse. J Pelvic Med and Surg 11:243–250
Hall AF, Theofrastous JP, Cundiff GW, Harris RL, Hamilton LF, Swift SE, Bump RC (1996) Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol 175:1467–1470
Dobben AC, Wiersema TG, Janssen LW, de Vos R, Terera MP, Baeten CGM, Stoker J (2005) Prospective assessment of interobserver agreement for defecography in fecal incontinence. Am J Roentgenol 185:1166–1172
Soligo M (2007) Posterior pelvic floor dysfunction: there is an immediate need to standardize terminology. Int Urogynecol J 18:369–371
Zyczynski HM, Lloyd LK, Kenton K, Menefee S, Boreham M, Stoddard AM, for the urinary Incontinence Treatment Network (UITN) (2007) Correlation of Q-tip values and Point Aa in stress-incontinent women. Obstet Gynecol 110:39–43
Burrows LJ, Sewell C, Leffer KS, Cundiff GW (2003) The accuracy of clinical evaluation of posterior wall defects. Int Urogynecol J 14:160–163
Altman D, Lopez A, Kierkgaard J, Zetterstrom J, Falconer C, Pollack J, Mellgren A (2005) Assessment of posterior vaginal wall prolapse: comparison of physical findings to cystodefecoperitoneography. Int Urogynecol J 16:96–103
Kenton K, Shott S, Brubaker L (1997) Vaginal topography does not correlate with visceral position in women with pelvic organ prolapse. Int Urogynecol J 8:336–339
Kelvin FM, Maglinte DDT, Hornback JA, Benson JT (1992) Pelvic prolapse: assessment with evacuation proctography (defaecography). Radiology 184:547–551
Da Silva GM, Gurland B, Sleemi A, Levy G (2006) Posterior vaginal wall does not correlate with fecal symptoms or objective measures of anorectal function. Am J Obstet Gyencol 195:1742–1747
Burrows LJ, Meyn LA, Walters MD, Weber AM (2004) Pelvic symptoms in women with pelvic organ prolapse. Obstet Gynecol 104:982–988
Soligo M, Salvatore S, Emmanuel AV, De Ponti E, Zoccatelli M, Cortese M, Milani R (2006) Patterns of constipation in urogynecology: clinical importance and pathophysiologic insights. Am J Obstet Gynecol 195:50–55
Swift SE (2000) The distribution of pelvic organ support in a population of female subjects seen for routine gynaecologic health care. Am J Obstet Gynecol 183:277–285
Lienemann A, Anthuber C, Baron A, Reiser M (2000) Diagnosing enteroceles using dynamic resonance imaging. Dis Colon Rectum 43:205–213
Maglinte DD, Bartram C (2007) Dynamic imaging of posterior compartment pelvic floor dysfunction by evacuation proctography: techniques, indications, results and limitations. Eur J Radiol 61:454–461
Roovers JP, Van der Bom G, Van der Vaart CH, Heintz AP (2005) Prediction of findings at defecography in patients with genital prolapse. BJOG 112:1547–53
Acknowledgement
The authors would like to thank Jan-Paul W.R. Roovers, Academic Medical Center-University of Amsterdam, for his careful reading and his contribution to the revision of this article.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Groenendijk, A.G., van der Hulst, V.P., Birnie, E. et al. Correlation between posterior vaginal wall defects assessed by clinical examination and by defecography. Int Urogynecol J 19, 1291–1297 (2008). https://doi.org/10.1007/s00192-008-0632-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-008-0632-9