Abstract
Introduction and hypothesis
The etiology of pelvic organ prolapse (POP) likely includes over-distension or tears (avulsion) of the levator ani muscle. However, there is a lack of studies evaluating the association between symptoms of POP and these factors. This study was designed to determine the association between POP symptoms and clinical prolapse stage on the one hand, and pelvic floor functional anatomy on the other hand.
Methods
This prospective observational study included 258 patients seen at a tertiary urogynecological unit with symptoms of POP as defined by pertinent ICIQ questions. After informed consent and a detailed history including ICIQ responses, 3D transperineal ultrasonography was performed using a GE Voluson i ultrasound system. Offline analysis was performed on de-identified datasets.
Results
The mean age of the patients was 60.6 years (25–91 years) and their mean BMI was 29.8 kg/m2 (18–53 kg/m2). Levator defects were found in 78 (32.4%) of the patients and the defect was bilateral in almost half of these patients (n = 36). There were significant associations between awareness and visualization of a vaginal lump on the one hand and hiatal area measurements as well as diagnosis of avulsion on the other. Interference with everyday life was significantly associated with hiatal area and prolapse stage, but not with avulsion.
Conclusions
There is a significant association between awareness, visualization and/or feeling of a vaginal lump and abnormal pelvic floor functional anatomy, that is, hiatal ballooning and levator avulsion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Symptomatic female pelvic organ prolapse (POP) is a common gynecological problem that negatively affects various quality of life domains [1]. Although the pathophysiology is still poorly understood, both macroscopic trauma (‘avulsion’) and microtrauma (irreversible overdistension) to the levator ani muscle are regarded as causative factors in at least some forms of symptomatic female POP [2]. The first prospective study to demonstrate a direct association between levator trauma and vaginal childbirth was published in 2005. In a prospective observational study of nulliparous women, levator avulsion was diagnosed using 3D transperineal ultrasonography between 2 and 6 months postpartum in 14 (36%) of 39 women delivered vaginally [3]. Subsequent prospective observational studies found that levator avulsion occurs in 13–36% of vaginally parous women and is also prevalent in patients presenting for urogynecological evaluation [4–6]. Levator avulsion is more common in patients with major prolapse and a risk factor for prolapse recurrence [7–10]. In an observational longitudinal cohort study of 269 primigravidae, levator avulsion was diagnosed in 21% of those with vaginal delivery, and these women reported more troublesome vaginal symptoms according to the validated International Consultation on Incontinence Questionnaire–Vaginal Symptoms (ICIQ-VS) [5, 11].
While early studies of pelvic floor symptoms focused primarily on evaluating the relationship with prolapse stage, a few studies have evaluated the association with functional pelvic floor anatomy using ultrasonography [12, 13]. In addition, most of the data in the literature were obtained in Caucasians. We sought to determine the relationship between the most commonly reported vaginal symptoms of POP (awareness of lump/bulge; visualization of lump/bulge and the need for digitation to empty the bowels) and clinical prolapse stage, levator hiatal area at rest, on maximum pelvic floor muscle contraction (PFMC) and on Valsalva maneuver, and levator avulsion, in a multiethnic population.
Materials and methods
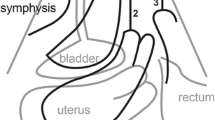
Between June 2013 and March 2015, women who attended a tertiary urogynecology clinic with symptomatic POP were invited to participate in a prospective observational study on pelvic floor morphology in South African women as part of an ongoing PhD thesis. After providing informed consent, patients were requested to empty their bladder. Clinical examination was performed with the patient in the supine position with the hips and knees flexed at 90°. Prolapse was staged according to the POP-Q method [14]. To assess levator muscle morphology 3D/4D transperineal pelvic floor ultrasonography (TPUS) was performed with a GE Voluson i system using a 4–8 MHz RAB probe with an acquisition angle of 85° . Volume datasets were de-identified and acquired at rest, on maximum PFMC and on maximum Valsalva maneuver by the first author. Levator hiatal areas were measured at rest, on maximum PFMC and on maximum Valsalva maneuver 6–8 weeks after volume acquisition using 4D View version 10 software, following the rendered volume method described previously [15]. Measurements were obtained by the first author, blinded against all clinical data. Tomographic ultrasound imaging (TUI) on maximum PFMC was used to diagnose levator avulsion as previously described [16]. Figure 1 illustrates marked distension (ballooning) of the levator hiatus on maximum Valsalva maneuver and the corresponding midsagittal plane in a woman presenting with a cystocele [17].
Transperineal 3D ultrasound images in the midsagittal plane in a woman presenting with a cystocele. a Measurement of cystocele descent. b The corresponding axial view shows marked distension (ballooning) of the levator hiatus on maximum Valsalva maneuver (S pubic symphysis, B bladder, R rectal ampulla, L levator ani, A anal canal)
Patients completed the ICIQ-VS which is routinely used at our urogynecology clinic. This study was approved by the National Research Ethics Committee (University of Pretoria, 226/2011). Statistical analysis was performed after normality testing which included histogram analysis and/or Kolmogorov-Smirnov testing using SPSS version 23. Our null hypothesis was defined as “prolapse symptoms/clinical prolapse stage are not associated with levator hiatal area and avulsion of the levator ani muscle as diagnosed by TPUS.”
To determine the relationship between commonly reported vaginal symptoms/POP-Q stage and levator avulsion, chi squared statistics were used since avulsion is a binary variable. The ICIQ produces four-point or five-point Likert responses, and thus we used analysis of variance tests to determine the relationship between vaginal symptoms and levator hiatal area (at rest, on maximum PFMC and on maximum Valsalva maneuver). A p value <0.05 was considered statistically significant.
Results
The datasets from 5 of 263 women recruited had missing information. Thus, 258 women were included in the study. Their mean age was 60.6 years (range 25–91 years), their median parity was 3 (range 0–9) and their mean BMI was 29.8 kg/m2 (range 18–53 kg/m2). Of the 258 women, 254 (98.5%) were vaginally parous. Previous assisted delivery was recalled by 38 women (14.7%), and 55 (21.3%) had undergone a previous prolapse operation. The study cohort was racially diverse: 31 (12%) Asian, 107 (41.5%) Black, and 120 (46.5%) Caucasian; ethnicity was self-reported. POP-Q stage II was detected in 124 patients (48.1%) and POP-Q stage III or IV in 115 (44.5%). The demographic characteristics of the 258 women are shown in Table 1. Only 236 datasets were analyzed for levator avulsion as 22 patients could not perform a pelvic floor muscle contraction, and four could not perform a Valsalva maneuver despite repeated coaching, leaving 254 datasets for hiatal area assessment.
Table 2 shows the associations between questionnaire answers, POP-Q staging and ultrasound measurements of functional pelvic floor anatomy. Statistically significant associations were found between awareness of lump or bulge in the vagina (question 5a of the ICIQ-VS), feeling and visualization of the lump or bulge (question 6a) and levator avulsion (p = 0.003, and p = 0.000, respectively) and for all measurements of hiatal area and POP-Q stage. Interference with everyday life was statistically significantly associated with POP-Q stage (p = 0.009) and hiatal area on Valsalva maneuver (p = 0.028) but not with levator avulsion. The correlation between visualization of bulge and interference with everyday life and hiatal area at rest did not reach statistical significance (p = 0.052 and p = 0.065, respectively). Exclusion of women with previous prolapse surgery did not materially change these results.
Discussion
This prospective observational study in a multiethnic population demonstrated strong correlations between abnormal functional pelvic floor anatomy and the core symptoms of POP defined according to the ICIQ-VS. This correlation was strongest for core symptoms such as awareness of lump/bulge and visualization or feeling of lump/bulge on the outside. Associations were weaker for the question on digitation to defecate. This is not surprising as the need for digitation has been shown to be positively associated with true rectoceles for which there is no strong link with abnormal levator ani anatomy [9, 18]. Of note, we chose to test the relationship between abnormal functional pelvic floor anatomy and the core symptoms of POP, as the other questions (“Are you aware of pain in your lower abdomen”, “Are you aware of soreness in your vagina”, “Do you feel that you have a reduced sensation in or around your vagina”) are nonspecific for POP, and statistical analysis did not reveal significant correlations with levator avulsion, levator hiatal area or POP-Q stage. ICIQ question 14 investigated by us is much less specific (“Overall, how much do vaginal symptoms interfere with your everyday life?”) as it would also be answered positively by women suffering, for example, from vaginal atrophy and/or dyspareunia.
The etiology of POP is thought to be multifactorial, but it is increasingly evident that in many instances prolapse is mediated by alterations in pelvic floor functional anatomy. There seems to be little doubt that major levator trauma is a factor in the pathogenesis of POP [9]. While a cause and effect relationship seems highly plausible for avulsion, the role of excessive hiatal distensibility, i.e. ballooning, is complex [19]. Since there is some evidence that ballooning often persists after a successful prolapse procedure, it may plausibly be considered a ‘cause’, but this remains unproven [20]. The findings of our study support this contention.
Considering that levator avulsion has a significant effect on both pelvic floor anatomy and function, it is not surprising that such trauma is associated with awareness and visualization of bulge [21–24]. Interestingly, this is not the case for other symptoms of pelvic floor dysfunction such as stress urinary incontinence, urge incontinence and anal incontinence [17, 25]. Dietz et al. [25] studied the relationship between levator avulsion and bladder function in 420 women presenting with pelvic floor dysfunction and lower urinary tract symptoms and found that women with avulsion were less likely to report stress urinary incontinence (p < 0.001) and urodynamic stress incontinence (p = 0.065) and were more likely to present with POP symptoms. The lack of association between levator avulsion and stress urinary incontinence/urodynamic stress incontinence and anal incontinence is most likely explained by the complex nature of the pathophysiology of urinary and fecal incontinence.
To our knowledge this is the first study conducted at a tertiary urogynecology clinic presenting data demonstrating an association between prolapse questionnaire components and abnormal functional anatomy of the pelvic floor. The multiethnic composition of our population could be considered a major strength, and we plan to report the findings of interethnic variation on pelvic organ descent and distensibility in a separate publication. Limitations of the study include the fact that ultrasonography and clinical examination were both performed by the first author. To overcome this potential bias, volumes were de-identified during acquisition and only analyzed 6–8 weeks later. Hence, the ultrasonography data presented here should not have been confounded by assessment bias. Also, we are aware that levator avulsion may be diagnosed at rest [26], but at the time of recruitment we decided to only allow diagnosis of levator avulsion on TUI during maximum PFMC, as originally described [16]. Finally, it would also be of interest to investigate the association between other symptoms of pelvic floor dysfunction (symptoms of bladder and sexual dysfunction) and pelvic floor functional anatomy. We are in the process of performing such a study in this cohort.
References
Mouritsen L, Larsen JP. Symptoms, bother and POPQ in women referred with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:122–127.
Dietz H. Clinical consequences of levator trauma. Ultrasound Obstet Gynecol. 2012;39:367–371.
Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106:707–712.
Shek KL, Dietz HP. Intrapartum risk factors for levator trauma. Br J Obstet Gynaecol. 2010;117:1485–1492.
van Delft K, Sultan AH, Thakar R, Schwertner-Tiepelmann N, Kluivers K. The relationship between postpartum levator ani muscle avulsion and signs and symptoms of pelvic floor dysfunction. Br J Obstet Gynaecol. 2014;121:1164–1171.
Dietz HP, Steensma AB. The prevalence of major abnormalities of the levator ani in urogynaecological patients. Br J Obstet Gynaecol. 2006;113:225–230.
Weemhoff M, Vergeldt TF, Notten K, Serroyen J, Kampschoer PH, Roumen FJ. Avulsion of puborectalis muscle and other risk factors for cystocele recurrence: a 2-year follow-up study. Int Urogynecol J Pelvic Floor Dysfunct. 2012;23:65–71.
Model AN, Shek KL, Dietz HP. Levator defects are associated with prolapse after pelvic floor surgery. Eur J Obstet Gynecol Reprod Biol. 2010;153:220–223.
Dietz H, Simpson J. Levator trauma is associated with pelvic organ prolapse. Br J Obstet Gynaecol. 2008;115:979–984.
Vergeldt TF, Notten KJ, Weemhoff M, van Kuijk SM, Mulder FE, Beets-Tan RG, et al. Levator hiatal area as a risk factor for cystocele recurrence after surgery: a prospective study. Br J Obstet Gynaecol. 2015;122:1130–1137.
Price N, Jackson SR, Avery K, Brookes ST, Abrams P. Development and psychometric evaluation of the ICIQ vaginal symptoms questionnaire: the ICIQ-VS. Br J Obstet Gynaecol. 2006;113:700–712.
Burrows LJ, Meyn LA, Walters MD, Weber AM. Pelvic symptoms in women with pelvic organ prolapse. Obstet Gynecol. 2004;104:982–988.
Romanzi LJ, Chaikin DC, Blaivas JG. The effect of genital prolapse on voiding. J Urol. 1999;161(2):581–586.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–17.
Dietz HP, Wong V, Shek KL. A simplified method for determining hiatal biometry. Aust N Z J Obstet Gynaecol. 2011;51:540–543.
Dietz HP. Quantification of major morphological abnormalities of the levator ani. Ultrasound Obstet Gynecol. 2007;29:329–34.
Dietz HP, Haylen BT, Broome J. Ultrasound in the quantification of female pelvic organ prolapse. Ultrasound Obstet Gynecol. 2001;18:511–514.
Dietz HP, Korda A. Which bowel symptoms are most strongly associated with a true rectocele? Aust N Z J Obstet Gynaecol. 2005;45:505–508.
Dietz HP, Franco AV, Shek KL, Kirby A. Avulsion injury and levator hiatal ballooning: two independent risk factors for prolapse? Acta Obstet Gynecol Scand. 2012;91:211–214.
Andrew B, Shek KL, Chantarasorn V, Dietz HP. Enlargement of the levator hiatus in female pelvic organ prolapse: cause or effect. Aust N Z J Obstet Gynaecol. 2013;53:74–78.
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185:1332–1337.
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109:295–302.
Abdool Z, Shek KL, Dietz HP. The effect of levator avulsion on hiatal dimension and function. Am J Obstet Gynecol. 2009;201:89.e1–89.e5.
Otcenasek M, Krofta L, Baca V, Grill R, Kucera E, Herman H, et al. Bilateral avulsion of the puborectal muscle: magnetic resonance imaging-based three-dimensional reconstruction and comparison with a model of a healthy nulliparous woman. Ultrasound Obstet Gynecol. 2007;29:692–696.
Dietz HP, Kirby A, Shek KL, Bedwell P. Does avulsion of the puborectalis muscle affect bladder function? Int Urogynecol J. 2009;20:967–972.
Dietz HP, Pattillo Garnham A, Guzmán Rojas R. Is it necessary to diagnose levator avulsion on pelvic floor muscle contraction? Ultrasound Obstet Gynecol. 2015. doi:10.1002/uog.15832.
Acknowledgements
The authors thank Susan Terblanch, B.Com (Hons. Statistics), OLRAC SPS, South Africa, for assistance with the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Abdool, Z., Dietz, H.P. & Lindeque, B.G. Prolapse symptoms are associated with abnormal functional anatomy of the pelvic floor. Int Urogynecol J 28, 1387–1391 (2017). https://doi.org/10.1007/s00192-017-3280-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3280-0