Abstract
Purpose
The aim of this study is to investigate clinical and magnetic resonance imaging (MRI) outcomes after anterior cruciate ligament (ACL) repair using the suture tape augmentation (STA) technique.
Methods
This prospective interventional case series included 35 patients who underwent STA ACL repair and were all followed up for 2 years. The ACL rupture was between 4 and 12 weeks old and per-operatively confirmed repairable. The International Knee Documentation Committee (IKDC), and Lysholm and Tegner scores were collected together with return to work (RTW), return to sport (RTS), re-rupture, and re-intervention rate. Lachman testing was performed and ACL healing was evaluated on MRI using a grading scale based on the ACL’s morphology and signal intensity with grade 1 representing good ACL healing and grade 3 representing poor ACL healing.
Results
The number of patients who returned to their pre-rupture level for IKDC, Lysholm, and Tegner scores at 2 years of follow-up are 17/26 (65.4%), 13/25 (52.0%), and 18/27 (66.7%) patients, respectively. Median RTW and RTS periods were 5.5 weeks (range 0–32 weeks) and 6 months (range 2–22 months), respectively. The Lachman side-to-side difference decreased significantly (P < 0.001) to less than 3 mm after surgery and remained stable. Four patients [11.4%, 95% CI (3.2, 26.7)] suffered from a re-rupture and three other patients [8.6%, 95% CI (1.8, 23.1)] needed a re-intervention for another reason than re-rupture. MRI follow-up of 31 patients showed overall grade 1 ACL healing in 14 (45.2%) patients, grade 2 ACL healing in 11 (35.5%) patients, and grade 3 ACL healing in 6 (19.4%) patients. A higher risk of re-rupture was associated with grade 3 ACL healing at 6 months post-operatively and a pre-operative Tegner score of ≥ 7.
Conclusion
This study shows that treatment of the acute, repairable ACL with the STA technique leads to a stable knee and favorable patient-reported outcome measures (PROMs). However, the re-rupture rate of 11.4% within the 2-year follow-up is a concern.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the 1970's and 80's, repair techniques were performed to treat anterior cruciate ligament (ACL) ruptures. These open repair techniques were abandoned after disappointing 5-year follow-up outcomes and ACL reconstruction became the gold-standard treatment [10, 32]. The introduction of several novel ACL repair techniques in the last decade has led to renewed interest in acute primary ACL repair [15, 22, 30, 32].
Van der List et al. reported that arthroscopic ACL repair techniques were safe, with failure rates of 7–11%, no complications, and functional outcome scores of > 85% of maximum scores [32]. Bucci et al. also reported that current literature on ACL repair reports better outcomes than in the past and subjective patient-reported outcome measures (PROMs) following ACL repair are not inferior to PROMs after ACL reconstruction [5].
One of the most published ACL repair techniques is the Dynamic Intraligamentary Stabilization (DIS) technique. The first publications by the DIS developer group confirm the healing capacity of the ACL and report excellent patient satisfaction and re-rupture rates of 2.9 and 10% [7, 15]. More recent publications from independent researchers show re-rupture rates up to 20% at 2-year follow-up and failure rates of 30% at 5-year follow-up [3, 37].
The Suture Tape Augmentation (STA) technique is a repair technique that preserves the native ACL and provides a secondary stabilizer to reinforce the repaired ACL during the healing phase [17, 42]. Preservation of the native ligament and its proprioceptors contributes to the feedback on position and dynamic stability of the knee, which improves rehabilitation after surgery [17, 24, 25, 30]. The STA technique is less-invasive compared to ACL reconstruction as graft harvesting morbidity is avoided, and the 3.5 mm bone tunnels drilled for the STA technique are less than half the size of bone tunnels needed for ACL reconstruction [17, 25, 32].
Currently, literature on STA ACL repair is not extensive. Two STA ACL case series report promising results in terms of an increase in PROMs and re-rupture rates of 4.8 and 1.5%. However, both studies do not compare postoperative data with pre-rupture data and lack a clinical as well as magnetic resonance imaging (MRI) follow-up [17, 22]. A retrospective study by Ortmaier et al. on sports activity states that short-term outcomes after STA ACL repair and ACL reconstruction are comparable, and that STA treatment enables sports activity and provides a sense of well-being similar to that of classic ACL reconstruction [36].
To the best of our knowledge, no independent prospective clinical results, longitudinal MRI follow-up, or risk factors for re-rupture on STA ACL repair have been reported yet.
The purpose of this study was to investigate clinical results, re-rupture risk factors, and MRI outcomes, 2 years after primary ACL repair with the STA technique. The hypothesis was that STA ACL repair would lead to an acceptable re-rupture rate around 6% and good clinical outcomes in terms of PROMs and knee stability.
Materials and methods
Patient recruitment
This prospective case series was approved by the institutional review board of the Antwerp University Hospital (B300201525523) and written informed consent was obtained from all study participants. Patients with a proximal or mid-substance bundle ACL rupture between 4 and 12 weeks old at the moment of surgery were recruited for treatment with the STA technique. Patients with an acute ACL rupture of less than 4 weeks old were recruited for treatment with DIS in a different study. Per-operative evaluation of good ACL tissue quality and sufficient contact between the stumps were vital inclusion criteria and determined whether the ACL was suitable for repair. Patients who were not active in sports and therefore could be treated with a conservative treatment, or patients who had multi-ligament injuries, excluding medial collateral ligament or anterolateral ligament lesions, or fractures that could compromise rehabilitation were not included.
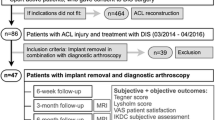
Seventy-two patients presented at the Antwerp University Hospital between 2015 and 2017 with an acute ruptured ACL of less than 12 weeks old. Thirteen patients were pre-operatively excluded for not meeting inclusion and exclusion criteria. Fifteen patients were treated within 4 weeks with DIS and 44 patients were allocated to be treated with the STA technique. Seven of these 44 patients were per-operatively excluded due to a non-repairable ACL rupture and two patients refused to be followed up. This prospective case series thus includes the first 35 consecutive patients treated with the STA technique at the Antwerp University Hospital who were all followed up for 2 years (Fig. 1).
The mean age (SD) of the study population was 32.8 (9.7) years and ranged from 18 to 54 years, and 18 (51.4%) patients were female.
Study design
Pre-rupture and postoperative PROMs after 6, 12, and 24 months were collected via questionnaires completed during consultation. The International Knee Documentation Committee (IKDC), Lysholm, Tegner, and Visual Analogue Scale (VAS) satisfaction scores were collected [13, 41]. Time between the surgery and return to work (RTW), time between the surgery and return to sport (RTS), re-intervention, and re-rupture data were collected, as well. Patients who suffered from re-rupture were subsequently treated with ACL reconstruction and further excluded from analysis of study results. Lachman testing was performed using a Rolimeter (Aircast, Neubeuern, Germany) to measure the anterior–posterior knee laxity difference between the injured and contralateral knee [19]. Clinical failure was defined as Lachman test of > 3 mm difference between the injured and contralateral knee in combination with a subjective feeling of instability. All patients were asked to undergo MRI follow-up at 6, 12, and 24 months post-operatively. Imaging was performed on a commercially available, clinical whole-body 3 T MRI system (Magnetom Prisma Fit, Siemens Healthcare, Erlangen, Germany). A dedicated phased-array knee-coil with 15 receiver channels and 1 transmission channel (Quality Electrodynamics, Mayfield Village, OH, USA) was used. A radiologist with 20 years of experience in musculoskeletal radiology interpreted all images, blinded to the patient’s clinical information. ACL healing on MRI was evaluated and categorized based on the ACL’s morphology and signal intensity, as follows: grade 1: well-defined, straight, continuous, normal-sized ACL with signal intensity similar to or only slightly higher than that of the posterior cruciate ligament (PCL); grade 2: normal sized (or slightly thickened) continuous, straight ACL demonstrating a high signal compared to that of the PCL; and grade 3: an ill-defined, irregular ACL that is thinned or not discernible [23, 40]. The ACL healing grade was defined per time point and an overall healing grade was determined for each patient with two or three postoperative MRI images based on the evolution of the ACL’s healing process over time during follow-up. For the test–retest reliability, we calculated a weighted kappa and found a very good reliability of 0.85 [95% CI (0.71, 0.98)] [29].
Surgical technique
The surgical technique has previously been described by Heusdens et al. [17]. Proximal and mid-bundle ACL ruptures were repaired using the STA technique (InternalBraceTM Ligament Augmentation Repair, Arthrex Inc., Naples, FL). After inspection of the ACL stump, a 3.5 mm tibial tunnel was drilled, ending at the center of the ACL footprint. A looped suture (FiberLink®, Arthrex Inc., Naples, FL) was placed through the distal ACL stump. At the femoral attachment, two-to-four microfracturing holes were made to enhance healing of the ACL. The femoral tunnel was drilled from the center of the femoral footprint inside out, with the knee fully flexed. A suture shuttle and the looped suture were passed through the femoral tunnel. A femoral button, loaded with a high-strength tape (FiberTape®, Arthrex Inc., Naples, FL), was flipped on the femoral cortex and the high-strength tape was advanced in the femoral tunnel. The high-strength tape was fixed in extension in the tibia with a bone anchor (SwiveLock®, Arthrex Inc., Naples, FL). The ruptured ACL fibers were gently tensioned with the looped suture to approximate the distal stump to the femoral footprint with the knee in 90° of flexion. The looped suture was tied on the femoral button with appropriate tension on the ACL.
Postoperative rehabilitation
The postoperative rehabilitation protocol could be compared to an accelerated ACL reconstruction protocol. Patients were allowed full weight-bearing with crutches as required during the first weeks. Physical therapy focused on early range of motion, muscle control, and restoration of function. This was facilitated by the limited pain and swelling, allowing accelerated early phase rehabilitation. Patients were allowed to perform pivoting sports if the knee had a full range of motion, no effusion, upper leg muscular circumference > 90%, and a single leg hop test > 90% [17].
Statistical analyses
A post hoc sample size calculation was performed, indicating that to obtain a 95% confidence interval of width 16% around the acceptable re-rupture rate of 6%, a total of 34 patients were needed. The goal of this study was to recruit all possible patients during a 2-year period and explore the findings. IKDC, Lysholm, VAS satisfaction scores, and the Lachman difference were presented as mean with standard deviation (SD) and Tegner score as median with range at the different time points. A linear mixed model including time (categorical variable) as a fixed effect and individual as a random intercept was fitted for each of the outcomes. In case of a significant time effect, post hoc testing was done comparing each of the considered time points to the pre-rupture (pre-operative) values on one hand, and the consecutive time points on the other hand. Raw and corrected P values using the Bonferroni–Holm correction for multiple testing were reported. The mixed model was corrected for age and gender by adding these factors, one by one, to the model. Return to pre-rupture level was defined, respectively, for the IKDC, Lysholm, and Tegner scores. A return to pre-rupture level was considered for the IKDC score if the current score was higher than or equal to the IKDC score pre-rupture minus 10 points [20]. A return to pre-rupture level was considered for the Lysholm score if the current score lay within the same range or a higher range as the pre-rupture score, assuming the following ranges: < 65 poor, 65–83 fair, 84–90 good, and > 90 excellent [33, 41]. For the Tegner score, a return to pre-rupture level was considered when the current score was the same as or higher than the pre-rupture score [20, 41]. Median times to reach the pre-rupture level were calculated for each of these scores with 95% confidence intervals. For RTW and RTS, Kaplan–Meier curves were produced, and median RTW and RTS with 95% confidence intervals were reported. For each time point during follow-up, the proportion of patients with different grades of ACL healing on MRI were reported. The ACL re-rupture rate was expressed as a proportion with 95% confidence interval (using exact Clopper–Pearson method). The association between the occurrence of re-rupture and the type of rupture, grade of ACL healing on MRI 6 months postoperative, pre-operative Tegner score (< 7 versus ≥ 7), and age (< 25 versus ≥ 25) on re-rupture was evaluated using a Fisher’s exact test. Results were considered significant if P < 0.05. All analyses were performed with SPSS statistics (IBM, version 21) and R 3.5.2 (R core team, 2018) except the mixed model, which was done in SAS 9.4 (SAS Institute, Cary NC).
Results
Patient and surgical characteristics
The patient population of this study consists of non-elite athletes from various sport levels, with pre-rupture Tegner scores ranging from 1 to 9, and a median Tegner score of 6. Pre-rupture, 9/33 (27.3%) patients were performing heavy physical work, 10/33 (30.3%) patients light physical work, and 14/33 (42.4%) patients sedentary work, and the working category of the two remaining patients is unknown.
Twenty-two (62.9%) patients had one or more additional procedures together with the STA surgery (Table 1). The overall mean (SD) surgery time was 91 (21) min. The mean (SD) surgery time of the patient group (n = 22) that underwent additional procedures during primary intervention was 102 (18) min and of the patient group (n = 13) without additional procedures was 73 (11) min.
Clinical outcomes during 2-year follow-up
Mean scores (SD) of IKDC, Lysholm, and VAS satisfaction at different time points during follow-up are reported in Table 2 together with the mean (SD) Lachman side-to-side difference in millimeters and median Tegner (range). The Lachman side-to-side difference remained < 3 mm post-operatively for all patients and no clinical failure was observed, except for those suffering from re-rupture. A linear mixed model with time as fixed effect showed significant effects over time for all these measurements (P < 0.001), except for VAS satisfaction (n.s.) which can be expected, since there are no pre-operative data available about patient satisfaction. Comparing the two-sided 95% CI for the difference between IKDC score at 24 months post-operatively and pre-rupture [15.1, − 4.7] to a non-inferiority margin of 10 IKDC points showed no non-inferiority after 24 months compared to the pre-rupture level. When correcting the linear mixed model for age and gender, we found a significant effect of these variables on the reported Tegner scores (P = 0.012 and P = 0.041, respectively). On average, there is a decrease in Tegner score of 1 point per 10 years [95% CI (− 1, − 0.2)], and on average, this score is 1 point [95% CI (− 2, − 0.04)] lower for women compared to men (time estimates were similar in the unadjusted and adjusted models). (Supplementary Table 1).
The proportions of patients who returned to their pre-rupture level for IKDC, Lysholm, and Tegner scores at different time points during follow-up are reported in Table 3. The median times to return to the pre-rupture level were 24 months [95% CI (17.8, 30.2)], 6 months [95% CI (3.2, 8.8)], and 12 months [95% CI (5.6, 18.4)] for the IKDC, Lysholm, and Tegner score, respectively. The median RTW period was 5.5 weeks [95% CI (4.4, 6.6)], ranging from 0 to 32 weeks, and is represented in Fig. 2. The median RTS period was 6 months [95% CI (4.6, 7.4)], ranging from 2 to 22 months, and is represented in Fig. 3.
MRI, re-intervention, and re-rupture
The proportion of patients for the different grades of ACL healing per time point is presented in Table 4. Cross-tabulation of the ACL healing grades showed that ACL healing grade did not change between 1 and 2 years of follow-up for the 20 patients who fully completed their MRI follow-up.
Three (8.6%) patients had a second surgery. One patient was treated for a medial meniscus rupture in combination with arthrofibrosis. The second patient suffered from arthrofibrosis and a cyclops lesion. The third patient was treated for an extension deficit that was caused by an overly tight FiberTape® (Arthrex, Inc., Naples, FL). These problems were solved after the re-intervention.
Four other patients (11.4%) suffered from re-rupture. One patient had a motorcycle accident 7 months post-operatively which resulted in an ACL re-rupture. Two patients experienced the re-rupture while playing soccer at 9 and 13 months post-operatively and one patient while dancing 22 months post-operatively. These patients were subsequently treated with an ACL reconstruction and further excluded from analysis of study results. Significance between type of rupture (proximal or mid-bundle), age, pre-operative Tegner score, and grade of ACL healing on MRI 6 months post-operatively and re-rupture are reported in Table 5.
Discussion
The most important findings of this study are that treatment with the STA ACL repair technique leads to a stable knee and favorable PROMs. However, four (11.4%) patients of our study cohort experienced a re-rupture within the 2-year follow-up. Analysis of risk factors for re-rupture showed that patients with a pre-operative Tegner score of ≥ 7 and with grade 3 ACL healing on MRI 6 months post-operatively have a higher chance of re-rupture.
Longitudinal MRI follow-up shows healing of the ACL between 6 and 12 months. The healing status remained unchanged between 12 and 24 months post-operatively in our study, suggesting that the repaired ACL does not further heal after one year post-operatively. Similar findings have been described in a study after ACL repair with DIS [16]. However, in a non-longitudinal MRI study, van der List et al. describe different results after ACL repair with a hyper-intense repaired ligament within 1 year, and a signal similar to that of the intact PCL only after 2 years [31]. Van Dyck et al. performed a Diffusion Tensor MRI (DTI) study on 14 patients treated with the STA technique. DTI results are different from conventional MRI, as DTI provides information about tissue microstructure and its degree of organization by quantifying water diffusion. Their findings suggest that healing of the ACL is incomplete at 24 months post-operatively [6]. We observed overall poor ACL healing on MRI in six (19.4%) of our study patients during the 2-year follow-up. Mid- to long-term MRI follow-up could contribute in determining the ACL repair healing time and potential clinical consequences. In addition, we observed a significant association between grade 3 ACL healing at 6 months post-operatively on MRI and re-rupture (P = 0.006). Postoperative MRI grading as a possible predictor for re-rupture after ACL repair has not been described before and needs to be further investigated.
Only two other STA ACL repair case series on adults, from the developer of the STA technique, have been published. They reported re-rupture rates of 1.5% and 4.5 [17, 22]. The re-rupture rate of 11.4% in this case series is rather high. The learning curve that comes with new techniques could be a possible explanation for this re-rupture rate. Also, patient selection could have influenced the re-rupture rate as patients with proximal and mid-bundle ruptures were included, while recent literature on other ACL repair techniques states that mid-substance ruptures are less suitable for repair and have a higher complication rate [8, 9, 34, 39]. Achtnich et al. and Jonkergouw et al. found similar results regarding failure after ACL repair using suture anchors with failure rates of 15% and 10.7%, respectively [1, 24]. Ahmad et al. conclude that there is evidence for the potential space of ACL repair in the decision tree for individualized treatment, and the best outcome will be in hands of the best patient selectors [2].
A quick rehabilitation was observed in this case series with a median RTW of 5.5 weeks (range 0–32 weeks) and median RTS of 6 months (range 2–22 months). Patients were only allowed to return to their pivoting sports if the knee had a full range of motion, no effusion, upper leg muscular circumference > 90%, and a single leg hop test > 90% [17]. Groot et al. describe a general RTW of 11 weeks after ACL reconstruction [12]. Lai et al. reported that most elite athletes RTS between 6 and 13 months after ACL reconstruction, which is less time than reported for non-elite athletes [28]. The healing phases of the repaired ACL differs from the ACL reconstruction ligamentization phases, and therefore, the rehabilitation period could be different, as well [40]. The quick rehabilitation in our study could be explained by the less-invasive STA technique and the preservation of the native ACL with its proprioceptors. ACL reconstruction does not preserve the native ligament with its proprioceptors which could lead to overloading of the ACL graft or loss of confidence in the knee [4, 11, 22, 25]. Kiapour et al. state that preservation of the native ACL with its proprioceptors may lead to more normal joint mechanics and a decreased risk for post-traumatic osteoarthritis [25].
The proportion of study patients who returned to their pre-rupture level for IKDC, Lysholm, and Tegner score increased over time to 65.4, 52.0, and 66.7%, respectively, but it needs to be noted that some patients who reached their pre-rupture level within 1 year lost this level again at 2 years. This is also observed after ACL reconstruction [20]. Ardern et al. report that less than 50% of patients RTS at their pre-rupture level after ACL reconstruction [4]. Ohsawa et al. on the other hand report that 64.6% of patients return to their pre-rupture level of Tegner score after ACL reconstruction, which is similar to the proportion observed in this study [35].
Risk factors for a re-rupture with the STA technique have not previously been described for adults. For DIS repair, young age and a high level of sport activity have been found to influence the risk of failure [2, 3, 14, 26, 27]. This case series with four patients who experienced a re-rupture suggests a higher risk on re-rupture for patients with a pre-operative Tegner ≥ 7 (P = 0.035) and for patients with grade 3 ACL healing on MRI at 6 months post-operatively (P = 0.006). In this study, the risk on a re-rupture for patients younger than 25 years did not reach significance (P = 0.061). As patient selection is emphasized for ACL repair, further investigation is needed [2].
The re-intervention rate of 20% in this STA ACL repair cohort study is similar to the re-intervention rate reported in other studies. Rousseau et al. observed a surgical re-intervention rate of 28% in their cohort of 958 ACL reconstruction patients [38]. Two randomized-controlled trials comparing ACL DIS repair versus ACL reconstruction report an overall re-intervention rate of 25.6% and 29.5% in the ACL DIS repair groups versus 22.5% and 33.3% in the ACL reconstruction groups [20, 26].
This study has several limitations. First, the sample size is relatively small, as the goal of this study was to recruit all possible patients during a 2-year period and explore the findings. We realize that a sample of 35 patients is not adequate to prove non-inferiority of 24 months to pre-rupture or the estimate percentage returned to pre-rupture level in a very precise way due to lack of power. Also the results on the effect of patient characteristics on the clinical outcomes or the analysis of the risk factors for re-ruptures are only explorative in this relative small sample and need further investigation. However, results in this study can serve as a pilot to guide future sample size calculations. Second, as this study is a case series, no direct comparison can be made between the STA technique and reconstruction surgery or other repair techniques. Hence, high-quality large randomized clinical trials with longer follow-up comparing ACL repair techniques and ACL reconstruction are needed [18, 21]. Third, patients were recruited at one center, which could bias the representativeness of our study population. Fourth, a learning curve could have influenced the results as patients included in this case series are the first patients who have been treated with the STA technique by two surgeons.
To the best of our knowledge, this is the first case series which presents independent prospective clinical results, longitudinal MRI follow-up, and risk factors for re-rupture on STA ACL repair. Patients with Tegner ≥ 7 have a higher chance on re-rupture. A strict patient selection could contribute in decreasing the re-rupture rate. Further studies with a long-term follow-up will have to show if modern ACL repair can be a “game changer” or if history will repeat itself [10].
Conclusion
This study shows that treatment of the acute, repairable ACL with the STA technique leads to a stable knee and favorable PROMs. However, the re-rupture rate of 11.4% within the 2-year follow-up is a concern.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- DIS:
-
Dynamic intraligamentary stabilization
- DTI:
-
Diffusion tensor imaging
- IKDC:
-
International Knee Documentation Committee
- MRI:
-
Magnetic resonance imaging
- PCL:
-
Posterior cruciate ligament
- PROM:
-
Patient-reported outcome measure
- RTS:
-
Return to sport
- RTW:
-
Return to work
- STA:
-
Suture tape augmentation technique
- VAS:
-
Visual analogue scale
References
Achtnich A, Herbst E, Forkel P, Metzlaff S, Sprenker F, Imhoff AB, Petersen W (2016) Acute proximal anterior cruciate ligament tears: outcomes after arthroscopic suture anchor repair versus anatomic single-bundle reconstruction. Arthroscopy 32:2562–2569
Ahmad SS, Schreiner AJ, Hirschmann MT, Schröter S, Döbele S, Ahrend MD, Stöckle U, Ateschrang A (2019) Dynamic intraligamentary stabilization for ACL repair: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:13–203
Ahmad SS, Schürholz K, Liechti EF, Hirschmann MT, Kohl S, Klenke FM (2020) Seventy percent long-term survival of the repaired ACL after dynamic intraligamentary stabilization. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05749-z
Ardern CL, Taylor NF, Feller JA, Webster KE (2012) Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med 40:41–48
Bucci G, Begg M, Pillifant K, Singleton SB (2018) Primary ACL repair vs reconstruction: investigating the current conventional wisdom. Orthop J Sports Med 6(6):2325967118S00049. https://doi.org/10.1177/2325967118S00049 (eCollection 2018 Jun)
Van Dyck P, Froeling M, Heusdens CHW, Sijbers J, Ribbens A, Billiet T (2020) Diffusion tensor imaging of the anterior cruciate ligament following primary repair with internal bracing: A longitudinal study. J Orthop Res. https://doi.org/10.1002/jor.24684
Eggli S, Kohlhof H, Zumstein M, Henle P, Hartel M, Evangelopoulos DS, Bonel H, Kohl S (2015) Dynamic intraligamentary stabilization: novel technique for preserving the ruptured ACL. Knee Surg Sports Traumatol Arthrosc 23:1215–1221
Engebretsen L, Svenningsen S, Benum P (1988) Poor results of anterior cruciate ligament repair in adolescence. Acta Orthop Scand 59:684–686
Evangelopoulos DS, Kohl S, Schwienbacher S, Gantenbein B, Exadaktylos A, Ahmad SS (2017) Collagen application reduces complication rates of mid-substance ACL tears treated with dynamic intraligamentary stabilization. Knee Surg Sports Traumatol Arthrosc 25:2414–2419
Feagin JA, Curl WW (1976) Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med 4:95–100
Fridén T, Roberts D, Ageberg E, Waldén M, Zätterström R (2001) Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. J Orthop Sports Phys Ther 31:567–576
Groot JAM, Jonkers FJ, Kievit AJ, Kuijer PPFM, Hoozemans MJM (2017) Beneficial and limiting factors for return to work following anterior cruciate ligament reconstruction: a retrospective cohort study. Arch Orthop Trauma Surg 137:155–166
Haverkamp D, Sierevelt IN, Breugem SJM, Lohuis K, Blankevoort L, Van Dijk CN (2006) Translation and validation of the Dutch version of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med 34:1680–1684
Henle P, Bieri KS, Brand M, Aghayev E, Bettfuehr J, Haeberli J, Kess M, Eggli S (2018) Patient and surgical characteristics that affect revision risk in dynamic intraligamentary stabilization of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 26:1182–1189
Henle P, Röder C, Perler G, Heitkemper S, Eggli S (2015) Dynamic Intraligamentary Stabilization (DIS) for treatment of acute anterior cruciate ligament ruptures: Case series experience of the first three years. BMC Musculoskelet Disord 16:27
Heusdens CH, Dossche L, Zazulia K, Michielsen J, Van Dyck P (2019) Tips and tricks to optimize surgical outcomes after acl repair using dynamic intraligamentary stabilization. Surg Technol Int 36:
Heusdens CHW, Hopper GP, Dossche L, Roelant E, Mackay GM (2019) Anterior cruciate ligament repair with Independent Suture Tape Reinforcement: a case series with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 27:60–67
Heusdens CHW, Zazulia K, Roelant E, Dossche L, Van Tiggelen D, Roeykens J, Smits E, Vanlauwe J, Van Dyck P (2019) Study protocol: A single-blind, multi-center, randomized controlled trial comparing dynamic intraligamentary stabilization, internal brace ligament augmentation and reconstruction in individuals with an acute anterior cruciate ligament rupture: LIBRE study. BMC Musculoskelet Disord 20:547
Höher J, Akoto R, Helm P, Shafizadeh S, Bouillon B, Balke M (2015) Rolimeter measurements are suitable as substitutes to stress radiographs in the evaluation of posterior knee laxity. Knee Surg Sports Traumatol Arthrosc 23:1107–1112
Hoogeslag RAG, Brouwer RW, Boer BC, de Vries AJ, Huis in ‘t Veld R, (2019) Acute anterior cruciate ligament rupture: repair or reconstruction? Two-year results of a randomized controlled clinical trial. Am J Sports Med 47:567–577
Hoogeslag RAG, Brouwer RW, de Vries AJ, Boer BC, Huis in ‘t Veld R (2020) Efficacy of nonaugmented, static augmented, and dynamic augmented suture repair of the ruptured anterior cruciate ligament: a systematic review of the literature. Am J Sports Med. Doi: https://doi.org/10.1177/0363546520904690363546520904690
Iain C, Anthony GM (2015) Anterior cruciate ligament repair revisited. preliminary results of primary repair with internal brace ligament augmentation: a case series. Orthoped Muscular Syst Curr Res. https://doi.org/10.4172/2161-0533.1000188
Ihara H, Miwa M, Deya K, Torisu K (1996) MRI of anterior cruciate ligament healing. J Comput Assist Tomogr 20:317–321
Jonkergouw A, van der List JP, DiFelice GS (2019) Arthroscopic primary repair of proximal anterior cruciate ligament tears: outcomes of the first 56 consecutive patients and the role of additional internal bracing. Knee Surg Sports Traumatol Arthrosc 27:21–28
Kiapour AM, Murray MM (2014) Basic science of anterior cruciate ligament injury and repair. Bone Joint Res 3:20–31
Kösters C, Glasbrenner J, Spickermann L, Kittl C, Domnick C, Herbort M, Raschke MJ, Schliemann B (2020) Repair with dynamic intraligamentary stabilization versus primary reconstruction of acute anterior cruciate ligament tears: 2-year results from a prospective randomized study. Am J Sports Med 48:1108–1116
Krismer AM, Gousopoulos L, Kohl S, Ateschrang A, Kohlhof H, Ahmad SS (2017) Factors influencing the success of anterior cruciate ligament repair with dynamic intraligamentary stabilisation. Knee Surg Sports Traumatol Arthrosc 25:3923–3928
Lai CCH, Ardern CL, Feller JA, Webster KE (2018) Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med 52:128–138
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
van der List JP, DiFelice GS (2017) Primary repair of the anterior cruciate ligament: a paradigm shift. Surgeon 15:161–168
Van Der List JP, Mintz DN, DiFelice GS (2019) Postoperative magnetic resonance imaging following arthroscopic primary anterior cruciate ligament repair. Adv Orthop 2019:5940195
van der List JP, Vermeijden HD, Sierevelt IN, DiFelice GS, van Noort A, Kerkhoffs GMMJ (2019) Arthroscopic primary repair of proximal anterior cruciate ligament tears seems safe but higher level of evidence is needed: a systematic review and meta-analysis of recent literature. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05697-8
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154
Mahapatra P, Horriat S, Anand BS (2018) Anterior cruciate ligament repair—past, present and future. J Exp Orthop 5:20
Ohsawa T, Kimura M, Chikuda H (2020) Patient-reported evaluation on giving way is important for return to preinjury activity level after Anterior Cruciate Ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06111-4
Ortmaier R, Fink C, Schobersberger W, Kindermann H, Leister I, Runer A, Hepperger C, Blank C, Mattiassich G (2020) Return to sports after anterior cruciate ligament injury: a matched-pair analysis of repair with internal brace and reconstruction using hamstring or quadriceps tendons. Sportverletz Sportschaden. https://doi.org/10.1055/a-1019-0949
Osti M, El Attal R, Doskar W, Höck P, Smekal V (2019) High complication rate following dynamic intraligamentary stabilization for primary repair of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 27:29–36
Rousseau R, Labruyere C, Kajetanek C, Deschamps O, Makridis KG, Djian P (2019) Complications after anterior cruciate ligament reconstruction and their relation to the type of graft: a prospective study of 958 cases. Am J Sports Med 47:2543–2549
Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I (1991) The long-term followup of primary anterior cruciate ligament repair: Defining a rationale for augmentation. Am J Sports Med 19:243–255
De Smet E, Heusdens CHW, Parizel PM, Van Dyck P (2019) MRI following primary repair of the anterior cruciate ligament. Clin Radiol 74:649 e641-649 e610
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. https://doi.org/10.1016/j.crad.2019.03.014
Wilson WT, Hopper GP, Byrne PA, MacKay GM (2016) Anterior cruciate ligament repair with internal brace ligament augmentation. Surg Technol Int 29:273–278
Funding
No funding was available for this study.
Author information
Authors and Affiliations
Contributions
This manuscript has been written by Dr. Heusdens who treated study patients, collected study data, and who was a major contributor to the writing of the manuscript, Karen Blockhuys who was a major contributor to the writing of the manuscript, Ella Roelant who performed statistical analyses on the study data and helped editing the manuscript, Dr. Dossche who treated study patients, collected study data, and helped editing the manuscript, Prof. Van Glabbeek who helped editing the manuscript, and Prof. Van Dyck who interpreted MRI scans of study participants and helped editing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Christiaan Heusdens: none; Karen Blockhuys: none; Ella Roelant: none; Lieven Dossche: none; Francis Van Glabbeek: none; Pieter Van Dyck: none.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee of the Antwerp University Hospital (B300201525523, 15/32/330) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Heusdens, C.H.W., Blockhuys, K., Roelant, E. et al. Suture tape augmentation ACL repair, stable knee, and favorable PROMs, but a re-rupture rate of 11% within 2 years. Knee Surg Sports Traumatol Arthrosc 29, 3706–3714 (2021). https://doi.org/10.1007/s00167-020-06399-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06399-2