Abstract
Purpose
The Attune® Knee System provides new instrumentation to achieve symmetric flexion/extension gaps in total knee arthroplasty (TKA). However, there is limited information on the optimal TKA technique using this system. The aim of this randomised controlled trial was to determine which surgical technique results in better postoperative clinical outcomes after TKA using the contemporary Attune® Knee System: the measured resection or gap balancing technique.
Methods
A prospective randomized controlled trial was conducted with 100 patients undergoing TKA using measured resection (n = 50) or gap balancing (n = 50) technique. The measured femoral sizer was used in the measured resection group, while the balanced femoral sizer was used in the gap balancing group. Functional outcomes and quality of life were assessed preoperatively and at 6 months and 2 years post-surgery, using the Knee Society Function Score (KSFS), Knee Society Knee Score (KSKS), Oxford Knee Score (OKS), the Physical Component Score (PCS) and Mental Component Score (MCS) of Short-Form 36 (SF-36). Using weight-bearing coronal radiographs, the hip-knee-ankle angle (HKA), coronal femoral component angle (CFA), coronal tibial component angle (CTA) and joint line height were also evaluated for each patient.
Results
There were no significant differences in the functional scores or the proportion of patients from each group who were satisfied or had their expectations fulfilled at 6 months or 2 years post-surgery. There was also no significant difference in the number of patients who attained minimum clinically important difference (MCID) postoperatively between the groups. Postoperatively, there was no significant difference in the number of HKA outliers between the groups (p = 0.202). The postoperative CFA (p = 0.265) and CTA (p = 0.479) were similar between the groups. There was also no significant difference in the absolute change (p = 0.447) or proportion of outliers (p = 0.611) for joint line height between the groups.
Conclusion
Both measured resection and gap balancing techniques resulted in comparable functional and quality of life outcomes up to 2 years post-surgery. Both techniques appear to be equally effective in achieving excellent outcomes with the Attune® Knee System.
Level of evidence
I.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Achieving symmetric flexion and extension gaps and optimal soft tissue balancing are crucial for optimal knee kinematics, which can prevent accelerated polyethylene wear, patellofemoral instability [2], anterior knee pain [5], and flexion gap instability [22]. There are currently two different surgical techniques which can be used to achieve this goal: measured resection and gap balancing [29].
Measured resection is the conventional Total Knee Arthroplasty (TKA) technique which uses bony landmarks for setting femoral rotation [27]. Equal and balanced gaps are achieved by bony resection at the distal femur and proximal tibia. However, failure to restore balanced gaps may occur with this technique due to distortion of bony landmarks, making them difficult to identify during surgery [3].
Gap balancing is an alternative surgical technique which relies on optimal soft tissue tensioning [7] to achieve equal and balanced flexion and extension gaps [25]. Using this technique, the femoral component is positioned parallel to the resected proximal tibia with each collateral ligament equally tensioned to obtain a rectangular flexion gap, independent of bony anatomy [5, 24].
Currently, both measured resection and gap balancing techniques can be performed during TKA, depending on the surgeon’s individual preference. In particular, the Attune® Knee System allows for flexion gap balancing using a balanced femoral sizer, which is not universally available in other TKA systems. However, there is a lack of randomised controlled trials directly comparing the measured resection and gap balancing techniques using this system. Hence, it remains unclear as to which is the preferred surgical technique using the Attune® Knee System. The aim of this randomised controlled trial was to determine which surgical technique results in better postoperative clinical outcomes after TKA using the contemporary Attune® Knee System: the measured resection or gap balancing technique. The hypothesis was that the measured resection and gap balancing techniques would result in comparable functional and quality of life outcomes up to 2 years post-surgery.
Material and methods
Patient selection and study design
Approval from the institutional ethics committee (SingHealth CIRB Ref: 2014/2070) and written informed consent from each patient was obtained. The study was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
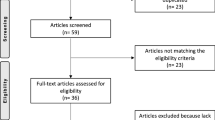
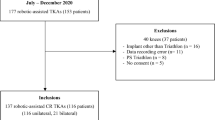
All patients undergoing a unilateral TKA in 2015 at a tertiary hospital were evaluated for eligibility. The inclusion criterion was primary osteoarthritis of the knee. Exclusion criteria included patients with rheumatoid arthritis, previous knee surgery, infection and those who could not be treated with unconstrained cruciate-retaining TKA and a short-stem tibial implant. Thirty-three patients were excluded from the present study as they had previous knee surgery (n = 10) or declined participation (n = 23).
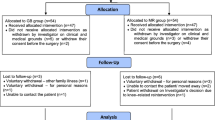
One hundred patients undergoing unilateral primary TKA were eventually recruited into this prospective clinical trial (Fig. 1). Using equal randomisation tables (1:1), the 100 patients were randomized into 2 groups: measured resection group (n = 50) and gap balancing group (n = 50). The patients were blinded to which group they were allocated to. The postoperative team which assessed them was also blinded to which group each patient belonged to. There were no significant differences in baseline patient demographics between the groups in terms of age, gender, side of surgery or preoperative BMI (Table 1).
Surgical techniques
All surgeries were performed via the medial parapatellar approach with patella eversion under tourniquet control. The distal femur resection was done first, followed by the proximal tibia.
All patients underwent TKA using BrainLAB® DASH® Knee Navigation System (BrainLAB®, Munich, Germany) that was designed as an image-free system to restore the mechanical alignment of the lower limb.
After placement of the distal femur intramedullary rod, the reference array was placed firmly into the cutting guide slot and the plane of the cutting guide was verified with navigation. If the value was equal or more than 2° from the mechanical axis of the femur, the cutting guide would be adjusted to within 1° of the mechanical axis. Following this, the distal femur cut was performed. This surgical step was similarly repeated for the proximal tibia cutting guide slot, after placement of the extramedullary tibia cutting guide to the bone.
Verification of rotational orientation of the femur implant could not be determined with this DASH® Knee Navigation System workflow. In the measured resection group, with the knee in 90° of flexion, the measured femoral sizer (with anterior reference option) from the Attune® Knee System was used. The transepicondylar axis was used to determine the rotation of the femoral component. In the gap balancing group, with the knee in 90° of flexion, the balanced femoral sizer (only has anterior reference option) from the Attune® Knee System was used. The femoral rotation was based off the proximal tibial cut to achieve equal and balanced flexion gaps. To assess the ligament tension intraoperatively, the tibia bone was held firmly with one hand and the Tensioning Knob on the balanced femoral sizer was used to apply a varus/valgus stress, while observing for lift off between the foot of the balanced femoral sizer and the proximal tibial cut. The predicted insert thickness will be known to the surgeon, before performing the 4-in-1 cut on the distal femur. All patients received cemented, fixed-bearing, cruciate-retaining Attune TKA with patella resurfacing. No drain was used.
Outcome measures
In addition to range of motion (ROM), functional outcomes and quality of life were assessed preoperatively and at 6 months and 2 years postoperatively, using the Knee Society Function Score (KSFS) [12], Knee Society Knee Score (KSKS) [12], Oxford Knee Score (OKS) [6], Physical Component Score (PCS) and Mental Component Score (MCS) of Short-Form 36 (SF-36) [30]. Postoperative expectation and satisfaction scores at 6 months and 2 years postoperatively were also assessed.
The number of patients who attained minimum clinically important difference (MCID) at 6 months and 2 years post-surgery for each functional score was also evaluated. The MCID of KSFS and KSKS was 6 points for both scores [17] and that of OKS was 5 points [4].
Using weight-bearing coronal radiographs, the hip-knee-ankle angle (HKA), coronal femoral component angle (CFA) and coronal tibia component angle (CTA) were also evaluated for each patient. The HKA was determined by the angle between a line from the center of the femoral head to the center of the knee (mechanical axis of femur) and a line from the center of the knee to the center of the ankle (mechanical axis of tibia) from preoperative and postoperative radiographs. Normal mechanical axis alignment was taken to be 180.0° ± 3.0° varus/valgus in this study; patients who did not fall within this range were considered HKA outliers [18]. The CFA was determined from postoperative radiographs by the angle formed by the femoral component and the mechanical axis of the femur. The CTA was determined from postoperative radiographs by the angle formed by the tibia base plate and the mechanical axis of the tibia.
The joint line height was also evaluated before and after surgery for each patient using the perpendicular distance between the adductor tubercle and the joint line (ATJL). The joint line reference was taken as a line tangent to both distal femoral condyles on preoperative radiographs and as the distal border of the femoral component on postoperative radiographs. Outliers were defined as a joint line elevation of > 4.0 mm, which has been shown to result in worse patient reported outcome measures (PROMs) [28].
Picture archiving and communication systems (PACS) was chosen for radiographic evaluation and measurements as it has been shown to have better inter- and intra-rater reliability than using hard copy radiographs [19]. Two reviewers blinded to the surgical technique performed the measurements on digital radiographic films on two separate occasions.
Statistical analysis
Power analysis was done prior to the conduct of this study. At 2 years after TKA, to detect a difference of 6 points in KSKS from a baseline mean score of 85 with standard deviation of 10, a sample size of 90 patients (with 45 patients in each group) would be required to achieve a power of 0.80. This calculation was performed for a two-sided test, with a Type I error of 0.05. Therefore, this study was designed to include a total of 100 patients (with 50 patients in each group).
Statistical analysis was performed with SPSS statistical software (version 24.0; SPSS, Chicago, Illinois). Univariate analysis was performed with Chi-square or the Fisher’s exact test for comparison of proportions between two categorical data. Student's t-test was used to compare continuous variables. The Mann–Whitney U test was used to compare the non-parametric data between two independent samples. Level of significance was taken as p < 0.05 for all comparisons.
Results
The preoperative ROM, KSFS, KSKS, OKS, PCS and MCS were comparable between the groups. There were no significant differences in the functional scores or the proportion of patients from each group who were satisfied or had their expectations fulfilled at 6 months or 2 years post-surgery. The number of patients who attained MCID for each of the functional scores was also comparable between the groups at each follow-up (Table 2).
The mean value of the postoperative mechanical axis was 177.2° ± 1.6° for the measured resection group and 177.4° ± 2.2° for the gap balancing group. Postoperatively, there was no significant difference in the number of HKA outliers between the groups (p = 0.202). The postoperative CFA (p = 0.265) and CTA (p = 0.479) were similar between the groups. There was also no significant difference in the absolute change (p = 0.447) or proportion of outliers (p = 0.611) for joint line height between the groups (Table 2).
Discussion
The most important finding of the present study was that no significant differences in functional outcome and quality of life scores were observed using both techniques. The present findings corroborate those of several other studies. Babazadeh et al. [1] carried out a randomised controlled trial comparing measured resection and gap balancing techniques using a cemented, total condylar primary prosthesis (PFC Depuy, Warsaw, IN). The authors concluded that gap symmetry was slightly better in the gap balancing group due to the computer navigation algorithm which prioritised gap symmetry and raised the joint line. However, this did not translate into any improvements in functional or quality of life scores, which were comparable between the groups up to 2 years post-surgery. Similarly, in a study of 24 knees, Teeter et al. [26] found no significant differences in both kinematic and functional outcomes between measured resection and gap balancing techniques using fixed-bearing, posterior-stabilized TKA (Triathlon, Stryker, Mahwah, NJ) with cemented fixation. The frequency of condylar lift-off, PCS, MCS, KSS and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores were comparable between the groups at 1 year post-surgery. In a clinical trial of 58 patients using a posterior-stabilized Press Fit Condylar (PFC) Sigma TKA system (Depuy Orthopaedics, Inc., Warsaw, IN), Miozzari et al. [20] found no significant differences between the measured resection and gap balancing groups at 1 year follow-up. In addition, the authors performed 3D gait evaluation and found no differences between the groups in gait parameters including gait velocity and flexion range in the gait cycle. This is in line with the present findings where postoperative ROM and functional outcomes were comparable between the groups.
It is also important to consider the significant variability that exists in anatomy and knee phenotypes across various populations [8,9,10,11]. As per the novel classification system for functional knee phenotypes proposed by Hirschmann et al. [11], the present study population had a lower limb phenotype of VARHKA9°, in contrast to other population which primarily consist of NEUHKA0° phenotype [8,9,10,11]. Hence, a VARHKA9° phenotype with HKA < 172.5° might be the “normal” alignment in the present population and perhaps, should be used as the target alignment for future TKA in such patients to achieve better postoperative functional outcomes.
Another key finding of the present study was that the number of patients who attained MCID at 6 months and 2 years post-surgery was comparable between the groups for all the functional and quality of life scores evaluated. MCID is defined as the smallest difference which patients perceive as beneficial and would justify a change in management [14]. It is an important concept used to determine whether a medical intervention improves perceived outcomes in patients and is believed to be a more rigorous measure of success for an intervention [21]. Hence the present findings suggest that both measured resection and gap balancing technique can be used to achieve equally good functional outcomes using the Attune® Knee System.
Tigani et al. [27] studied 126 patients who underwent TKAs using the measured resection or gap balancing technique and concluded that the measured resection technique resulted in better postoperative joint-line restoration, making it preferable. Using cemented, mobile-bearing implants (Cinetique, Medacta International SA, Castel San Pietro, Swiss), Sabbioni et al. [23] also found that while there was no difference between the groups in term of postoperative mechanical axis, the mean elevation of the joint line was significantly higher in the gap balancing group. However, unlike the present study, these studies lacked data on functional outcome scores and subjective patient satisfaction. Despite such kinematic findings, it has been shown that changing the joint line does not necessarily translate into poorer clinical outcomes [1, 16]. Hence, it is important to determine if the choice of TKA technique influences functional outcomes and quality of life as measured by patient reported outcome measures (PROMs).
Currently, conventional TKA achieves tissue balancing and implant stability by measured resection or gap balancing techniques, with neither method being clearly superior to the other. Balanced soft tissue is essential for optimal knee kinematics, and over-tensioning of ligaments can lead to reduced ROM. Previous studies have suggested that, as compared to measured resection, gap balancing results in significantly less condylar lift-off [7], more accurate gap symmetry [15], raised joint line [27] and better alignment in terms of femoral component rotation [13]. However, the present findings suggest that despite such studies reporting differences in kinematic outcomes between the techniques, there is no significant clinical difference in terms of change in joint line height or functional outcomes using the Attune® Knee System.
One of the strengths of this study is that it is an adequately powered, randomised controlled trial comparing the measured resection and gap balancing techniques. Secondly, this study was done with equal numbers in each group with no missing data and no patients lost to follow-up at 2 years post-surgery. Thirdly, this study considered differences in the number of patients who attained MCID in each group, which is an important measure to determine the clinical significance of an intervention. Fourthly, this is the first randomised controlled trial comparing the measured femoral sizer versus the balanced femoral sizer in the contemporary Attune® Knee System.
There are, however, also several limitations to the present study. Firstly, there was a limited follow-up period of 2 years. Hence while the present findings are applicable to short-term functional outcomes, studies with longer follow-up may be necessary to determine any differences in long-term effects between the techniques. Secondly, this study used pseudo-randomisation for patient allocation to ensure equal numbers in each group, which may have contributed to allocation bias. Thirdly, the present study did not compare intraoperative kinematic data and implant survivorship between the groups, which might support the use of either technique in future studies. Fourthly, postoperative TKA position was not evaluated with Computed Tomography (CT) scans and there was a lack of data on femoral rotation which could not be determined with this DASH® Knee Navigation System workflow. Nonetheless, the present study includes data on the CFA and CTA from postoperative radiographs.
Conclusions
This study found that both measured resection and gap balancing techniques result in comparable functional and quality of life outcomes up to 2 years post-surgery. Both techniques appear to be equally effective in achieving excellent outcomes with the Attune® Knee System, and the choice of which technique to use can be based on the surgeon’s individual preference in daily clinical practice.
Abbreviations
- KSFS:
-
Knee Society Function Score
- KSKS:
-
Knee Society Knee Score
- OKS:
-
Oxford Knee Score
- PCS:
-
Physical Component Score
- MCS:
-
Mental Component Score
- SF-36:
-
Short-Form 36
- MCID:
-
Minimum clinically important difference
- TKA:
-
Total knee arthroplasty
- BMI:
-
Body mass index
- HKA:
-
Hip-knee-ankle angle
- CFA:
-
Coronal femoral component angle
- CTA:
-
Coronal tibial component angle
- ATJL:
-
Adductor tubercle and joint line
- ROM:
-
Range of motion
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
- PROMs:
-
Patient-reported outcome measures
- CT:
-
Computed tomography
References
Babazadeh S, Dowsey MM, Stoney JD, Choong PF (2014) Gap balancing sacrifices joint-line maintenance to improve gap symmetry: a randomized controlled trial comparing gap balancing and measured resection. J Arthroplasty 29:950–954
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199811000-00021144-153
Boldt JG, Stiehl JB, Munzinger U, Beverland D, Keblish PA (2006) Femoral component rotation in mobile-bearing total knee arthroplasty. Knee 13:284–289
Clement ND, MacDonald D, Simpson AH (2014) The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:1933–1939
Daines BK, Dennis DA (2014) Gap balancing vs. measured resection technique in total knee arthroplasty. Clin Orthop Surg 6:1–8
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Jt Surg Br 80:63–69
Dennis DA, Komistek RD, Kim RH, Sharma A (2010) Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 468:102–107
Hess S, Moser LB, Amsler F, Behrend H, Hirschmann MT (2019) Highly variable coronal tibial and femoral alignment in osteoarthritic knees: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:1368–1377
Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB (2019) Phenotyping of hip-knee-ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc 27:1378–1384
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclercq V, Hess S (2019) Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg Sports Traumatol Arthrosc 27:1385–1393
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Katz MA, Beck TD, Silber JS, Seldes RM, Lotke PA (2001) Determining femoral rotational alignment in total knee arthroplasty: reliability of techniques. J Arthroplasty 16:301–305
King MT (2011) A point of minimal important difference (MID): a critique of terminology and methods. Expert Rev Pharmacoecon Outcomes Res 11:171–184
Lee DH, Park JH, Song DI, Padhy D, Jeong WK, Han SB (2010) Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc 18:381–387
Lee HJ, Lee JS, Jung HJ, Song KS, Yang JJ, Park CW (2011) Comparison of joint line position changes after primary bilateral total knee arthroplasty performed using the navigation-assisted measured gap resection or gap balancing techniques. Knee Surg Sports Traumatol Arthrosc 19:2027–2032
Lee WC, Kwan YH, Chong HC, Yeo SJ (2017) The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc 25:3354–3359
Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R (2009) Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty 24:570–578
Marx RG, Grimm P, Lillemoe KA, Robertson CM, Ayeni OR, Lyman S et al (2011) Reliability of lower extremity alignment measurement using radiographs and PACS. Knee Surg Sports Traumatol Arthrosc 19:1693–1698
Miozzari HH, Armand S, Turcot K, Lubbeke A, Bonnefoy-Mazure A (2019) Gait analysis 1 year after primary TKA: no difference between gap balancing and measured resection technique. J Knee Surg. https://doi.org/10.1055/s-0039-3402079
Polascik BW, Bin Abd Razak HR, Chong HC, Lo NN, Yeo SJ (2018) Acceptable functional outcomes and patient satisfaction following total knee arthroplasty in Asians with severe knee stiffness: a matched analysis. Clin Orthop Surg 10:337–343
Romero J, Stahelin T, Binkert C, Pfirrmann C, Hodler J, Kessler O (2007) The clinical consequences of flexion gap asymmetry in total knee arthroplasty. J Arthroplasty 22:235–240
Sabbioni G, Rani N, Del Piccolo N, Ben Ayad R, Carubbi C, Tigani D (2011) Gap balancing versus measured resection technique using a mobile-bearing prosthesis in computer-assisted surgery. Musculoskelet Surg 95:25–30
Springer BD, Parratte S, Abdel MP (2014) Measured resection versus gap balancing for total knee arthroplasty. Clin Orthop Relat Res 472:2016–2022
Tanaka K, Muratsu H, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M (2007) Soft tissue balance measurement in anterior cruciate ligament-resected knee joint: cadaveric study as a model for cruciate-retaining total knee arthroplasty. J Orthop Sci 12:149–153
Teeter MG, Perry KI, Yuan X, Howard JL, Lanting BA (2017) Contact kinematic differences between gap balanced vs measured resection techniques for single radius posterior-stabilized total knee arthroplasty. J Arthroplasty 32:1834–1838
Tigani D, Sabbioni G, Ben Ayad R, Filanti M, Rani N, Del Piccolo N (2010) Comparison between two computer-assisted total knee arthroplasty: gap-balancing versus measured resection technique. Knee Surg Sports Traumatol Arthrosc 18:1304–1310
van Lieshout WAM, Valkering KP, Koenraadt KLM, van Etten-Jamaludin FS, Kerkhoffs G, van Geenen RCI (2019) The negative effect of joint line elevation after total knee arthroplasty on outcome. Knee Surg Sports Traumatol Arthrosc 27:1477–1486
Viskontas DG, Skrinskas TV, Johnson JA, King GJ, Winemaker MJ, Chess DG (2007) Computer-assisted gap equalization in total knee arthroplasty. J Arthroplasty 22:334–342
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
VM, MCL, MHLL and JYC helped in data collection, statistical analysis and drafting the manuscript. HNP, SLC, NNL and SJY conceived the study, study design and carried out the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval from the institutional ethics committee (SingHealth CIRB Ref: 2014/2070) was obtained.
Informed consent
Written consent from each patient was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moorthy, V., Lai, M.C., Liow, M.H.L. et al. Similar postoperative outcomes after total knee arthroplasty with measured resection and gap balancing techniques using a contemporary knee system: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 29, 3178–3185 (2021). https://doi.org/10.1007/s00167-020-06103-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06103-4