Abstract
Introduction
To achieve the most desirable post-operative results, operation techniques and procedures for total knee arthroplasty (TKA) are highly standardized. However, debates persist whether patients having undergone a gap balancing technique (GB) perform better than those having undergone measured resection (MR) technique. Therefore, a meta-analysis study was conducted to investigate advantages of GB compared to the MR. The focus of the present study was on clinical and functional scores, radiological measurements and further complications.
Materials and methods
The present meta-analysis was conducted according to the PRISMA checklist. In November 2019, literature search was performed. All clinical studies comparing measured resection technique versus gap balancing technique for primary total knee arthroplasty were considered for inclusion. Only articles reporting quantitative data under the outcomes of interest were eligible for inclusion. The methodological quality assessment and statistical analyses were performed through the Review Manager Software version 5.3 (The Cochrane Collaboration, Copenhagen).
Results
Data from 25 clinical trials (2971 procedures) were collected. Patient baseline demonstrated a good comparability. No difference among the two cohorts was found in terms of SF-12 Mental and Physical, ROM, KSS, KSS Function, OKS, WOMAC. No difference was found in the alignment of mechanical axis and femoral rotation. During the knee motion, no difference was found between the medial and lateral gaps among the two techniques. The GB showed a significant elevated joint line (P < 0.0001), along with a longer duration of the operating time (P = 0.001). No differences were found in terms of revision surgery, aseptic loosening or prosthetic infections.
Conclusion
GB and MR achieve similar outcomes for TKA. In the GB group, a proximalisation of the joint line and extended operating time was detected. Regarding the additional outcomes of interest, the present analysis showed comparability between both groups, MR and GB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) yields high satisfaction rate among selected patients [1]. TKA restores physiological joint biomechanics and improves patients quality of life [2]. Surgical techniques and procedures for TKA are highly standardized to achieve the best outcome. However, debates persist whether gap balancing (GB) performs better than the measured resection (MR) technique [3]. In the GB technique, an initial soft tissue release followed by bone resection is performed to obtain gap balancing over flexion and extension [4, 5]. Differently, in the MR technique, a direct bony resection following the anatomical landmarks (e.g., anteroposterior and transepicondylar axis) is performed, with subsequent soft tissue release [4, 6]. Several topic-related scientific reviews have been conducted [7,8,9,10]. However, whether any technique provides better implant alignment and surgical outcome is subject of current discussion [11,12,13]. Despite recent publications of clinical studies, consensus is still lacking and debates are ongoing [3, 14,15,16]. Therefore, a meta-analysis of current evidence was performed. The purpose of the present study was to update current evidences and investigate possible advantages of GB compared to the MR in terms of clinical scores, radiological measurements and complications.
Materials and methods
Search strategy
The present meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA checklist [17]. The endpoints of the initial research were:
-
P (population): total knee arthroplasty;
-
I (intervention): measured resection;
-
C (comparison): gap balancing;
-
O (outcomes): clinical scores, radiological measurements, complications.
Literature search
Two independent authors (FM, AD) performed the literature search. In November 2019, the main online databases were accessed: Pubmed, Google Scholar, Scopus, Embase. The following keywords were used in combination: total knee arthroplasty, replacement, prosthesis, measured, resection, gap, balancing, compared, versus, KSS, lateral, medial, component, rotation, axis, condyle, femur, tibia, joint line, radiography, outcomes, scores, KSS, SF-12, ROM, flexion, extension. The full-text of the articles of interest were accessed. The bibliographies of the included studies were also screened. Disagreements between the authors were mutually debated and solved by a third author (JE).
Eligibility criteria
All clinical studies comparing measured resection versus gap balancing operating techniques for primary total knee arthroplasty were considered for inclusion. According to the authors’ language capabilities, only articles in English, Italian, German, Spanish, French were included. According to the Oxford Centre of Evidenced-Based Medicine [18], articles level of evidence I to IV were included in the present work. Only articles published in the last 10 years were included. Reviews, case reports, expert opinions, letters, editorials were excluded. Animal, in vitro, cadaveric and biomechanics studies were also excluded. Articles treating TKA in revision setting were excluded. Both mobile and fixed bearing were included. Only articles reporting quantitative data were considered for inclusion. Missing data under the outcomes of interest warranted the exclusion from the present study.
Outcomes of interest
Two independent authors (FM, AD) performed data extraction. The following data were collected for each study: author and year of publication, type of study, number of TKAs, mean age of the samples, percentage of female study population and mean BMI (kg/m2). The outcomes of interest were the analysis of the post-operative clinical scores (KSS, KSFS, SF-12 Physical and Mental, ROM, OKS, WOMAC), operating time, radiological measurements of the medial and lateral joint gaps during the knee motion, the mechanical axis, external rotation of femoral component implant. Further complications were collected: infections, aseptic loosening and revision rate.
Methodological quality assessment
The methodological quality assessment was performed through the risk of bias summary of the Review Manager Software version 5.3 (The Cochrane Collaboration, Copenhagen). To evaluate the quality, the following bias were investigated: selection, detection, attrition, reporting and other not-reported sources of possible bias.
Statistical analysis
The statistical analysis was performed by one author (FM). The Review Manager Software version 5.3 was used for the present investigation. Continuous variables were analysed through the inverse variance statistical method with the standardized mean difference (SMD) effect measure. Dichotomic variables were analysed through the Mantel–Haenszel statistical method with the odd ratio (OR) effect measure. Heterogeneity was evaluated through the \(\chi\)2 and Higgins I2 test. If \(\chi\)2 > 0.5 and I2 > 60% high level of heterogeneity was detected. A fixed effect analysis model was set in all the comparisons. If high data heterogeneity was evidenced, a random effect analysis model was adopted. The confidence interval was set at 95% in all the comparisons. Values of P < 0.05 were considered statistically significant.
Results
Search result
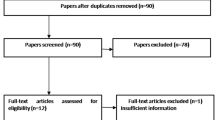
The initial literature search resulted in 355 publications of which only 82 compared directly the 2 surgical techniques MR versus GB for TKA. Of them, 23 studies were duplicates, therefore excluded. A further 23 publications did not match the eligibility criteria, 11 because lack of quantitative data under the outcomes of interest. This last selection process left 25 studies for inclusion: 11 randomized clinical trials, 8 prospective and 6 retrospective cohort studies. The flowchart of the literature search is shown in Fig. 1.
Methodological quality assessment
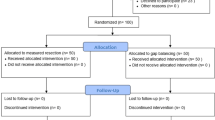
The Cochrane risk of bias summary tool detected some limitations. There was a moderate risk of selection and detection bias. This was attributable to the reduced number of the studies providing samples randomization (40%) and blinding (45%). The risk of attrition and reporting bias were low. Similar, also the risk of unknown source of bias scored low. Concluding, the quality of the methodological assessment was good. The risk of bias summary if shown in Fig. 2.
Patient demographic
Data from a total of 2971 TKAs were analysed. The mean follow-up was 32.53 ± 28.7 months. The MR group included 1470 samples (64% female). The mean age of this cohort was 69.99 ± 3.6 years, the mean BMI 29.45 2.1 kg/m2. The GB group included 1501 samples (67% female). The mean age of this cohort was 69.55 ± 4.5 years, the mean BMI 29.64 2.0 kg/m2. No differences were found among the groups concerning age (P = 0.4), gender (P = 0.3) and BMI (P = 0.4). The demographic generalities of patients included are shown in Table 1.
Outcomes of interest
Any noteworthy differences among the two cohort were found in terms of the analysis of several scores; SF-12 Mental (SMD − 0.05; 95% CI − 0.29, 0.19; Higgins I2 44%; P = 0.7), SF-12 Physical (SMD − 0.41; 95% CI − 0.65, − 0.17; Higgins I2 0%; P = 0.06), ROM (SMD − 0.10; 95% CI − 0.32, 0.13; Higgins I2 72%; P = 0.4), KSS (SMD − 0.11; 95% CI − 0.23, 0.01; Higgins I2 24%; P = 0.06), KSS Function (SMD − 0.20; 95% CI − 0.46, 0.06; Higgins I2 76%; P = 0.1; Fig. 3), OKS (SMD − 0.11; 95% CI − 0.42, 0.21; Higgins I2 61%; P = 0.5), WOMAC (SMD 0.01; 95% CI − 0.18, 0.20; Higgins I2 58%; P = 0.9). A quicker surgical procedure was detected in the MR group (SMD − 1.14; 95% CI − 1.54, − 0.74; Higgins I2 68%; P = 0.001).
No differences were found in terms of revision surgery at a mean of 62.55 months follow-up (OR: 1.32; 95% CI 0.59, 2.99; Higgins I2 0%; P = 0.6), 75.40 months (OR 1.24; 95% CI 0.53, 2.89; Higgins I2 0%; P = 0.6), and 95.10 months (OR 1.54; 95% CI 0.58, 4.10; Higgins I2 0%; P = 0.4). Similarly, no differences were found in terms of aseptic loosening (OR 1.67; 95% CI 0.64, 4.35; Higgins I2 0%; P = 0.3) and infections (OR 0.71; 95% CI 0.19, 2.64; Higgins I2 0%; P = 0.6). The GB cohort achieved insignificant more accurate restoration of mechanical axis (SMD 0.27; 95% CI − 0.10, 0.63; Higgins I2 78%; P = 0.2) and increased femoral rotational alignment (SMD − 0.02; 95% CI − 0.39, 0.035; Higgins I2 82%; P = 0.9, Fig. 4) but a significant elevated joint line (SMD − 0.48; 95% CI − 0.70, − 0.27; Higgins I2 62%; P < 0.0001).
No statistically significant difference was found between the gaps: medial gap extension (SMD 0.26; 95% CI 0.02, 0.49; Higgins I2 38%; P = 0.3), lateral gap extension (SMD 0.42; 95% CI 0.19, 0.65; Higgins I2 0%; P = 0.7), medial gap flexion (SMD 0.37; 95% CI 0.14, 0.60; Higgins I2 38%; P = 0.06), lateral gap flexion (SMD 0.22; 95% CI − 0.25, 0.69; Higgins I2 76%; P = 0.4). Mean flexion gaps (SMD 1.43; 95% CI 0.56, 2.31; Higgins I2 94%; P = 0.1), mean extension gaps (SMD − 1.07; 95% CI − 4 to 45, 2.30; Higgins I2 100%; P = 0.5).
Table 2 reports the main findings of the comparisons.
Discussion
According to the main findings of the present meta-analysis, the GB group demonstrated a proximalisation of the joint line and required longer operating time. Mechanical axis and femoral rotational alignment showed high data heterogeneity and no differences between the groups were detected. The analysis of clinical scores, flexion and extension gaps detected no statistically significant difference. Surgical revision rate, aseptic loosening and infections did not show any worthy difference between the two techniques. The present analysis showed comparability between MR and GB technique. Indeed, at mean follow-up of approximately 5, 6 and 8 years, no difference concerning surgical revision rate between both groups have been detected concluding that both techniques, MR and GP are safe and feasible.
The goal of TKA is to achieve mechanical axis alignment in the range of 180° (± 3°). According to the Higgins I2 test, heterogeneity was moderate, and the final effect showed that mechanical axes were comparable among the two cohorts. In fact, these two techniques should not affect the coronal alignment. Femoral rotation alignment is defined as the difference between the femoral component and the transepicondylar axis of the knee [41]. In the present study, no differences among the groups were detected. Femoral rotation alignment is crucial to obtain a rectangular balanced flexion gap, optimal joint kinematics and patellofemoral tracking and soft tissue balancing [42, 43]. Indeed, excessive implants intra- or extra-rotation may result in anterior knee pain, instability infection and patellar fracture [44]. Rotational alignment was hardly debated. MR-TKA alignment is more dependent on surgeon’s experience in locating anatomical landmarks and axes around the knee [45]. This can improve the risk of component malposition [46, 47]. Fehring et al. [44] reported that rotational errors through bony landmarks > 3° occurred in 45% of patients. A cadaveric study conducted by Katz et al. [48] reported no significant differences in component rotation between MR and GB technique. Theoretically, GB-TKA promoting exact gaps tension during the range of motion, offer more accurate rotational alignment. However, results from the present study clearly stated similarity among the techniques. Even though this comparison was affected by high heterogeneity, the final effect was close to the no-effect line and the test for overall significance found no difference between the two techniques in terms of femoral rotational alignment.
The comparison of joint line positioning was characterized by low value of heterogeneity and statistically significant higher position in favour of the GB group. This comparison showed high reliability. Resecting bone tissue according to margin gaps symmetry and to the soft tissue balancing, the final result will be over resection of the femoral bone compared to the MR technique. Changes in the position of the joint line are prevalent in revision setting and can lead to soft tissue disbalance and patellofemoral instability [49, 50]. A biomechanical study of Fornalski et al. [51] found that position of joint line affects the patellofemoral joint and the tibial implants, and may result in a reduced ROM, anterior knee pain and finally component wear. In 2019, Van Lieshout et al. performed a systematic review involving 1255 primary TKAs. They found analysed that a higher joint line can negatively influence the KSS. Recent meta-analyses found similar result, attesting clinical relevance to this outcome [8,9,10].
To obtain soft tissue balancing, surgeons try to implement symmetrical, equivalent and rectangular gaps. It has been stated that for acceptable GB, gaps in both, full extension and 90° flexion have to be ≤ 3 cm. This circumstance may explain the prolonged time of surgery reported in the GB group. In the present meta-analysis, we found no significant difference among medial and lateral gap balancing during extension and 90° of flexion drawing the conclusion that MR achieves sufficient gap balancing. Similar results have been reported by high-quality meta-analyses [10].
Analysis of the clinical scores, complications detected no statistically significant difference. Similar results have been found by Li et al. [9] in over 2259 samples. Conversely, Huang et al. [10] reported improved score results in the GB cohort in approximately 300 TKAs. Hence, more precise investigations and further high-quality studies are required.
The main limitation of the present study is the reduced number of studies included and related samples considered for analysis. Furthermore, the studies included differed for type of implant and surgical approach, and especially the gaps tensions of the GB studies differed. These factors may explain, at least partially, some of the heterogeneities in evidence in the present study. Further high-quality studies with longer follow-up are required to investigate long-term survivorships among the two techniques.
Conclusion
According to the main findings of the present meta-analysis, GB and MR achieve similar outcomes in TKA. The GB group presented a proximalisation of the joint line and required longer operating time. Regarding further outcomes of interest, the present analysis demonstrates comparability between MR and GB.
References
Migliorini F, Eschweiler J, Tingart M, Rath B (2019) Posterior-stabilized versus cruciate-retained implants for total knee arthroplasty: a meta-analysis of clinical trials. Eur J Orthop Surg Traumatol 29(4):937–946. https://doi.org/10.1007/s00590-019-02370-1
Migliorini F, Tingart M, Niewiera M, Rath B, Eschweiler J (2019) Unicompartmental versus total knee arthroplasty for knee osteoarthritis. Eur J Orthop Surg Traumatol 29(4):947–955. https://doi.org/10.1007/s00590-018-2358-9
Hernandez-Hermoso JA, Nescolarde-Selva L, Rodriguez-Montserrat D, Martinez-Pastor JC, Garcia-Oltra E, Lopez-Marne S (2019) Different femoral rotation with navigated flexion-gap balanced or measured resection in total knee arthroplasty does not lead to different clinical outcomes. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05591-3
Daines BK, Dennis DA (2014) Gap balancing vs. measured resection technique in total knee arthroplasty. Clin Orthop Surg 6(1):1–8. https://doi.org/10.4055/cios.2014.6.1.1
Dennis DA, Komistek RD, Kim RH, Sharma A (2010) Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 468(1):102–107. https://doi.org/10.1007/s11999-009-1112-3
Mantas JP, Bloebaum RD, Skedros JG, Hofmann AA (1992) Implications of reference axes used for rotational alignment of the femoral component in primary and revision knee arthroplasty. J Arthroplasty 7(4):531–535. https://doi.org/10.1016/s0883-5403(06)80075-6
Riviere C, Iranpour F, Auvinet E, Howell S, Vendittoli PA, Cobb J, Parratte S (2017) Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res 103(7):1047–1056. https://doi.org/10.1016/j.otsr.2017.07.010
Moon YW, Kim HJ, Ahn HS, Park CD, Lee DH (2016) Comparison of soft tissue balancing, femoral component rotation, and joint line change between the gap balancing and measured resection techniques in primary total knee arthroplasty: a meta-analysis. Medicine (Baltimore) 95(39):e5006. https://doi.org/10.1097/MD.0000000000005006
Li S, Luo X, Wang P, Sun H, Wang K, Sun X (2018) Clinical outcomes of gap balancing vs measured resection in total knee arthroplasty: a systematic review and meta-analysis involving 2259 subjects. J Arthroplasty 33(8):2684–2693. https://doi.org/10.1016/j.arth.2018.03.015
Huang T, Long Y, George D, Wang W (2017) Meta-analysis of gap balancing versus measured resection techniques in total knee arthroplasty. Bone Joint J 99-B(2):151–158. https://doi.org/10.1302/0301-620X.99B2.BJJ-2016-0042.R2
Blakeney W, Beaulieu Y, Kiss MO, Riviere C, Vendittoli PA (2019) Less gap imbalance with restricted kinematic alignment than with mechanically aligned total knee arthroplasty: simulations on 3-D bone models created from CT-scans. Acta Orthop 90(6):602–609. https://doi.org/10.1080/17453674.2019.1675126
Shalhoub S, Lawrence JM, Keggi JM, Randall AL, DeClaire JH, Plaskos C (2019) Imageless, robotic-assisted total knee arthroplasty combined with a robotic tensioning system can help predict and achieve accurate postoperative ligament balance. Arthroplast Today 5(3):334–340. https://doi.org/10.1016/j.artd.2019.07.003
Riviere C, Iranpour F, Harris S, Auvinet E, Aframian A, Chabrand P, Cobb J (2017) The kinematic alignment technique for TKA reliably aligns the femoral component with the cylindrical axis. Orthop Traumatol Surg Res 103(7):1069–1073. https://doi.org/10.1016/j.otsr.2017.06.016
Aunan E, Rohrl SM (2018) No detrimental effect of ligament balancing on functional outcome after total knee arthroplasty: a prospective cohort study on 129 mechanically aligned knees with 3 years' follow-up. Acta Orthop 89(5):548–554. https://doi.org/10.1080/17453674.2018.1485283
Cidambi KR, Robertson N, Borges C, Nassif NA, Barnett SL (2018) Intraoperative comparison of measured resection and gap balancing using a force sensor: a prospective, randomized controlled trial. J Arthroplasty 33(7S):S126–S130. https://doi.org/10.1016/j.arth.2018.02.044
Kim CW, Lee CR, Gwak HC, Kim JH, Kwon YU, Kim DY (2019) The Effects of Surgical technique in total knee arthroplasty for varus osteoarthritic knee on the rotational alignment of femoral component: gap balancing technique versus measured resection technique. J Knee Surg. https://doi.org/10.1055/s-0038-1676766
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Howick J CI, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford levels of evidence. Oxford Centre for Evidence-Based Medicine. Available at https://www.cebmnet/indexaspx?o=5653. Accessed Nov 2019
Babazadeh S, Dowsey MM, Vasimalla MG, Stoney JD, Choong PFM (2018) Gap balancing sacrifices joint-line maintenance to improve gap symmetry: 5-year follow-up of a randomized controlled trial. J Arthroplasty 33(1):75–78. https://doi.org/10.1016/j.arth.2017.08.021
Babazadeh S, Dowsey MM, Stoney JD, Choong PF (2014) Gap balancing sacrifices joint-line maintenance to improve gap symmetry: a randomized controlled trial comparing gap balancing and measured resection. J Arthroplasty 29(5):950–954. https://doi.org/10.1016/j.arth.2013.09.036
Baier C, Fitz W, Craiovan B, Keshmiri A, Winkler S, Springorum R, Grifka J, Beckmann J (2014) Improved kinematics of total knee replacement following partially navigated modified gap-balancing technique. Int Orthop 38(2):243–249. https://doi.org/10.1007/s00264-013-2140-x
Becker R, Malzdorf M, Starke C, Randolf P, Lohmann C (2012) No difference between tibia-first and femur-first techniques in TKA using computer-assisted surgery. Knee Surg Sports Traumatol Arthrosc 20(10):2011–2016. https://doi.org/10.1007/s00167-012-1928-3
Churchill JL, Khlopas A, Sultan AA, Harwin SF, Mont MA (2018) Gap-balancing versus measured resection technique in total knee arthroplasty: a comparison study. J Knee Surg 31(1):13–16. https://doi.org/10.1055/s-0037-1608820
Clement ND, Makaram N, Bell J, Tiemessen CH, Mehdi SA, Livingston SJ (2017) Columbus(R) computer navigated total knee arthroplasty: gap balancing versus measured resection. Knee 24(6):1442–1447. https://doi.org/10.1016/j.knee.2017.08.004
Hommel H, Kunze D, Hommel P, Fennema P (2017) Small improvements in postoperative outcome with gap balancing technique compared with measured resection in total knee arthroplasty. Open Orthop J 11:1236–1244. https://doi.org/10.2174/1874325001711011236
Hommel H, Abdel MP, Perka C (2017) Kinematic femoral alignment with gap balancing and patient-specific instrumentation in total knee arthroplasty: a randomized clinical trial. Eur J Orthop Surg Traumatol 27(5):683–688. https://doi.org/10.1007/s00590-016-1865-9
Jawhar A, Hutter K, Scharf HP (2016) Outcome in total knee arthroplasty with a medial-lateral balanced versus unbalanced gap. J Orthop Surg (Hong Kong) 24(3):298–301. https://doi.org/10.1177/1602400305
Lee DH, Park JH, Song DI, Padhy D, Jeong WK, Han SB (2010) Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc 18(3):381–387. https://doi.org/10.1007/s00167-009-0983-x
Lee HJ, Lee JS, Jung HJ, Song KS, Yang JJ, Park CW (2011) Comparison of joint line position changes after primary bilateral total knee arthroplasty performed using the navigation-assisted measured gap resection or gap balancing techniques. Knee Surg Sports Traumatol Arthrosc 19(12):2027–2032. https://doi.org/10.1007/s00167-011-1468-2
Lee SY, Lim HC, Jang KM, Bae JH (2017) What factors are associated with femoral component internal rotation in TKA using the gap balancing technique? Clin Orthop Relat Res 475(8):1999–2010. https://doi.org/10.1007/s11999-017-5319-4
Luyckx T, Peeters T, Vandenneucker H, Victor J, Bellemans J (2012) Is adapted measured resection superior to gap-balancing in determining femoral component rotation in total knee replacement? J Bone Joint Surg Br 94(9):1271–1276. https://doi.org/10.1302/0301-620X.94B9.28670
Matsumoto T, Muratsu H, Kawakami Y, Takayama K, Ishida K, Matsushita T, Akisue T, Nishida K, Kuroda R, Kurosaka M (2014) Soft-tissue balancing in total knee arthroplasty: cruciate-retaining versus posterior-stabilised, and measured-resection versus gap technique. Int Orthop 38(3):531–537. https://doi.org/10.1007/s00264-013-2133-9
Nagai K, Muratsu H, Kanda Y, Tsubosaka M, Kamenaga T, Miya H, Matsushita T, Niikura T, Kuroda R, Matsumoto T (2018) Intraoperative soft tissue balance using novel medial preserving gap technique in posterior-stabilized total knee arthroplasty: comparison to measured resection technique. Knee Surg Sports Traumatol Arthrosc 26(11):3474–3481. https://doi.org/10.1007/s00167-018-4945-z
Nikolaides AP, Kenanidis EI, Papavasiliou KA, Sayegh FE, Tsitouridis I, Kapetanos GA (2014) Measured resection versus gap balancing technique for femoral rotational alignment: a prospective study. J Orthop Surg (Hong Kong) 22(2):158–162. https://doi.org/10.1177/230949901402200208
Pang HN, Yeo SJ, Chong HC, Chin PL, Ong J, Lo NN (2011) Computer-assisted gap balancing technique improves outcome in total knee arthroplasty, compared with conventional measured resection technique. Knee Surg Sports Traumatol Arthrosc 19(9):1496–1503. https://doi.org/10.1007/s00167-011-1483-3
Sabbioni G, Rani N, Del Piccolo N, Ben Ayad R, Carubbi C, Tigani D (2011) Gap balancing versus measured resection technique using a mobile-bearing prosthesis in computer-assisted surgery. Musculoskelet Surg 95(1):25–30. https://doi.org/10.1007/s12306-011-0110-2
Singh VK, Varkey R, Trehan R, Kamat Y, Raghavan R, Adhikari A (2012) Functional outcome after computer-assisted total knee arthroplasty using measured resection versus gap balancing techniques: a randomised controlled study. J Orthop Surg (Hong Kong) 20(3):344–347. https://doi.org/10.1177/230949901202000316
Stephens BF, Hakki S, Saleh KJ, Mihalko WM (2014) Clinical alignment variations in total knee arthroplasty with different navigation methods. Knee 21(5):971–974. https://doi.org/10.1016/j.knee.2014.03.001
Teeter MG, Perry KI, Yuan X, Howard JL, Lanting BA (2017) Contact kinematic differences between gap balanced vs measured resection techniques for single radius posterior-stabilized total knee arthroplasty. J Arthroplasty 32(6):1834–1838. https://doi.org/10.1016/j.arth.2016.12.054
Tigani D, Sabbioni G, Ben Ayad R, Filanti M, Rani N, Del Piccolo N (2010) Comparison between two computer-assisted total knee arthroplasty: gap-balancing versus measured resection technique. Knee Surg Sports Traumatol Arthrosc 18(10):1304–1310. https://doi.org/10.1007/s00167-010-1124-2
Witoolkollachit P, Seubchompoo O (2008) The comparison of femoral component rotational alignment with transepicondylar axis in mobile bearing TKA. CT-scan study J Med Assoc Thai 91(7):1051–1058
Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y (2001) Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg 14(3):152–156
Harman MK, Banks SA, Kirschner S, Lutzner J (2012) Prosthesis alignment affects axial rotation motion after total knee replacement: a prospective in vivo study combining computed tomography and fluoroscopic evaluations. BMC Musculoskelet Disord 13:206. https://doi.org/10.1186/1471-2474-13-206
Fehring TK (2000) Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res 380:72–79. https://doi.org/10.1097/00003086-200011000-00010
Whiteside LA, Arima J (1995) The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res 321:168–172
Dennis DA (2008) Measured resection: an outdated technique in total knee arthroplasty. Orthopedics 31(9):940. https://doi.org/10.3928/01477447-20080901-08(943–944)
Arima J, Whiteside LA, McCarthy DS, White SE (1995) Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone Joint Surg Am 77(9):1331–1334. https://doi.org/10.2106/00004623-199509000-00006
Katz MA, Beck TD, Silber JS, Seldes RM, Lotke PA (2001) Determining femoral rotational alignment in total knee arthroplasty: reliability of techniques. J Arthroplasty 16(3):301–305. https://doi.org/10.1054/arth.2001.21456
ten Ham AM, Wymenga AB, Jacobs WC (2005) The use of the knee joint-line balancer to control patella position in revision total knee arthroplasty. Knee 12(2):89–92. https://doi.org/10.1016/j.knee.2004.05.004
Singerman R, Heiple KG, Davy DT, Goldberg VM (1995) Effect of tibial component position on patellar strain following total knee arthroplasty. J Arthroplasty 10(5):651–656. https://doi.org/10.1016/s0883-5403(05)80210-4
Fornalski S, McGarry MH, Bui CN, Kim WC, Lee TQ (2012) Biomechanical effects of joint line elevation in total knee arthroplasty. Clin Biomech (Bristol, Avon) 27(8):824–829. https://doi.org/10.1016/j.clinbiomech.2012.05.009
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Migliorini, F., Eschweiler, J., Mansy, Y.E. et al. Gap balancing versus measured resection for primary total knee arthroplasty: a meta-analysis study. Arch Orthop Trauma Surg 140, 1245–1253 (2020). https://doi.org/10.1007/s00402-020-03478-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03478-4