Abstract
Purpose
This study was conducted to compare the efficacy between the oval femoral tunnel technique and the conventional round femoral tunnel technique in ACL reconstruction using an autologous hamstring tendon on the basis of the postoperative clinical outcomes and ACL graft tendon maturity. The hypothesis was that ACL reconstruction performed using the oval femoral tunnel technique was better than that performed using the round femoral tunnel technique in clinical functions and graft maturity.
Methods
One hundred and eight patients who underwent anatomical single-bundle ACL reconstruction were included in this study and the follow-up period was at least 2 years. Thirty-nine patients admitted between February and August in 2016 were included in the oval femoral tunnel group and 69 patients admitted between September 2016 and March 2017 were included in the round femoral tunnel group. The Lachman test result, pivot-shift test result, Lysholm score, IKDC score, and VAS score were used for the clinical evaluation. An objective assessment of anteroposterior stability was performed using a KT1000 arthrometer. Postoperative MRI was conducted to compare the ACL graft maturity differences between the oval femoral tunnel group and round femoral tunnel group, where the signal/noise quotient (SNQ) was calculated. In addition, second-look arthroscopy was conducted to compare the graft status and synovial coverage at 24 months postoperatively.
Results
All the patients presented with significant improvement in all clinical scores from the preoperative period to the 24-month follow-up. During the postoperative follow-up period, no statistically significant differences were found between the two groups in terms of the VAS score, knee ROM, Lachman test results, and graft status determined in the second-look arthroscopic evaluation. The Lysholm score was 97.1 ± 3.9 and 94.8 ± 5.6 in the oval femoral tunnel group and round femoral tunnel group, respectively, at the 24-month follow-up (p = 0.031). The IKDC subjective score was 92.0 ± 2.6 and 89.0 ± 3.6 in the oval femoral tunnel group and round femoral tunnel group, respectively, at the end of the follow-up period (p < 0.001). Significantly more patients with 1-degree positive pivot-shift test results were observed in the round femoral tunnel group (10/65) than in the oval femoral tunnel group (1/37) at the end of the follow-up period (p = 0.048). The mean SNQ of the oval femoral tunnel group was 2.7 ± 0.9, which was significantly lower than that of the round femoral tunnel group (3.6 ± 1.1) at the 24-month postoperative follow-up (p < 0.001).
Conclusions
Based on the clinical evaluations, MRI findings and second-look arthroscopy results of the two groups, the oval femoral tunnel technique yielded significantly better knee function and knee laxity restoration and more mature ACL grafts than the round femoral tunnel technique, whereas no significant differences were found at the second-look arthroscopy.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction surgery has been widely performed worldwide to treat ACL injuries [12, 31]. In recent years, numerous studies have indicated that conventional single-bundle ACL reconstruction cannot fully restore rotatory stability, biomechanical properties, and functional knee kinematics [15, 22]. The goal of ACL reconstruction is to achieve anatomical restoration of the native ACL footprint and functional knee kinematics [7, 10, 20, 30]. However, the technical details of ACL reconstructions still remain controversial, especially the tunnel placement, which has been shown to be a critical factor for ACL reconstruction [8, 10, 36]. Previous studies have reported that an ACL consists of an anteromedial bundle and a posterolateral bundle and double-bundle ACL reconstruction has been performed to restore the ACL anatomy [2, 11, 17], but the clinical results are controversial. Several studies have also showed no superiority of double-bundle ACL reconstruction over the single-bundle technique, when the graft was placed in the proper anatomical position at the ACL insertion point [1, 3, 5, 13, 19]. In addition, there are more concerns about the double-bundle technique than the single-bundle technique due to its highly invasive nature, high surgical skill requirements, and complex revision surgery [1, 15, 32]. Therefore, the focus has shifted back to anatomical single-bundle ACL reconstruction, where grafts are placed at the anatomical footprint. Recently, some studies have introduced the flat ribbon concept for the femoral insertion of the ACL, which has been gaining popularity [35, 36]. Sasaki et al. [29] showed that the proximal ACL fibres spread in a fanlike manner on the medial aspect of the lateral femoral condyle and that the femoral insertion is shaped like an oval. In recent studies, the oval femoral tunnel (OFT) technique used in ACL reconstruction has been attempted to restore the ACL anatomic structure and precisely mimic the femoral footprint [23, 24, 26].
Thus, the surgical methods used in previous studies were suboptimal and some studies did not include comprehensive postoperative follow-ups and evaluations. The signal/noise quotient (SNQ) has been used to evaluate ACL graft maturity in recent years. The lower the SNQ value is, the lower the water content of the graft and the higher the maturity of the ACL graft is [18, 37]. This non-randomized prospective controlled study was conducted to compare the differences in ACL graft maturity and clinical outcomes between a conventional round femoral tunnel (RFT) group and an OFT group. The OFT technique was considered biomimetic to the native ACL and the hypothesis was that the OFT group had better clinical outcomes and graft maturity than the RFT group. The OFT technique provided a better option for ACL reconstruction and has the potential to replace the RFT technique as an ideal surgical procedure for ACL reconstruction.
Materials and methods
Ethical approval was obtained from the Institutional Review Board (IRB) of the First Affiliated Hospital of Chongqing Medical University (ID 2016-178). In this prospective non-randomized controlled study, informed consent was obtained from all the patients regarding the details of the study and all possible complications related to the study.
The subjects included in the study were selected from a group of patients who underwent ACL reconstruction in the First Affiliated Hospital of Chongqing Medical University between February 2016 and March 2017. The inclusion criteria were as follows: individuals who were aged between 16 and 60 years; had isolated ACL injuries; had no previous history of knee surgery; and were scheduled to undergo arthroscopic single-bundle ACL reconstruction with hamstring tendon autografts. The exclusion criteria were as follows: patients who had an Outerbridge classification [34] of cartilage damage more severe than grade II; underwent a total meniscectomy; were obese and had a significantly restricted flexion angle; had a mental disorder; or had significant co-morbidities.
Forty-two patients admitted between February and August in 2016 were assigned to the OFT group (group 1) and 74 patients admitted between September 2016 and March 2017 were categorized as the RFT group (group 2). A total of eight patients were excluded from this study. In group 1, one patient had grade III cartilage damage and two patients underwent a total meniscectomy. In group 2, two patients declined to participate, while three other patients underwent a total meniscectomy. All the above factors were part of the exclusion criteria. Therefore, of the remaining 108 patients, 39 were included in group 1 and 69 were included in group 2. Two participants in group 1 and four in group 2 were lost to follow-up due to the inaccessibility of the follow-up center. Only 19 patients in group 1 and 31 in group 2 underwent second-look arthroscopy at the end of the follow-up period. No significant differences with regards to the demographic characteristics were detected between the two groups (ns). Thirty patients were female and 78 were male. The age of the participants ranged from 16 to 57 years, with an average age of 31.3 years in group 1 and 29.8 in group 2. The average body mass index (BMI) was 23.4 kg/m2 and 23.3 kg/m2 in group 1 and group 2, respectively. There were no significant differences between the two groups in concomitant injuries and co-morbidities. The mean diameter of the grafts was 8.2 ± 0.5 mm in group 1 and 8.2 ± 0.5 mm in group 2, with no significant difference (Table 1).
Surgical technique
Diagnostic knee arthroscopy was performed under epidural anesthesia. A 3-cm oblique incision was made on the medial aspect of the tibial tubercle and it was used to harvest both the gracilis and semitendinosus tendons with a tendon harvester. The end of each graft was reinforced with No. 2 Ethibond sutures to 30 millimeters using the whipstitch technique. The two strands of the grafts were looped over the RIGIDLOOP to create the 4-strand construct.
Femoral tunnel creation
The anterior medial approach was established prior to femoral tunnel drilling. In the RFT group, the anatomical landmarks for femoral tunnel drilling were based on the ACL femoral footprint and Petersen and Zantop’s study [27]. The footprints of the ACL were accurately visualized, a 4.5 mm hollow drill aided by a femoral guide pin was used to drill the lateral femoral cortex, and then a special reamer (6–10 mm, dependent on the graft diameter) was used to create the blind round tunnel (Fig. 1).
OFT creation: To create the oval-shaped tunnel, special oval dilatators that are available in different sizes were used and this technique was similar to the technique used by Peterson et al. [26]. The OFT was gradually dilatated by percussive compression. The femoral guide pin was drilled through the lateral femoral cortex via the anteromedial portal aimer. The specially selected and matched oval dilatator was gradually hammered into the femur to an approximate depth of 25–30 mm over a guide pin. The lateral femoral condylar cortex was then drilled with a 4.5 mm hollow drill, while the guide pin was held in position (Fig. 2, Video 1).
Tibial tunnel placement
The remaining part of the ACL was preserved to promote graft growth and localize the tibial tunnel. The anteromedial approach was used to position the anchor point of the tibial guide arm aimer in the center of the ACL stump. Details from Petersen and Zantop’s study [27] were used to identify the ACL tibial footprints, if no residual ACL was available. A guide pin was inserted and a 6–10 mm hollow reamer was introduced through the initial graft harvest incision to create the tibia round tunnel.
Graft fixation
Once the two tunnels were created, the ACL graft was passed through the tibial tunnel to the femoral tunnel with the help of the graft line that was attached to the ACL graft. The RIGIDLOOP and the ACL graft were inserted into the femoral tunnel via the tibial tunnel. The RIGIDLOOP was inverted and fixed, after it was passed through the lateral femoral cortex. Once the RIGIDLOOP was fixed, the knee joint was adjusted to 20 degrees of flexion, while the tibial end of the graft was retracted for manual tensioning. The tibial side of the graft was tightened at 20–30° of knee flexion, and Bio-Intrafix was inserted in the middle of the four tendons to a depth of 30 millimeters and fixed with a Milagro screw (Video 2).
Clinical evaluations
All the clinical evaluations were performed preoperatively and at 3 months, 6 months, 1 year, and 2 years after surgery. The clinical follow-ups were conducted by an independent examiner who was blinded to the study design. Passive knee ROM, which was expressed as a deficit in extension and flexion compared with the contralateral side, was measured with a goniometer preoperatively and at the 24-month follow-up. All participants were asked to complete the self-reported knee function surveys, including the Lysholm knee score questionnaire [38, 40] and the International Knee Documentation Committee (IKDC) questionnaire [9, 39]. Anteroposterior stability was objectively evaluated with the Lachman test and laxity was assessed using a KT1000 arthrometer and formulas to calculate the side–to-side anterior tibial translation difference (STSD) on the operative and contralateral knee at manual maximum tension and at 30° of flexion; the STSD results were categorized according to the IKDC guidelines (A 0–2 mm; B 3–5 mm; C 6–10 mm; D > 10 mm) [4, 28]. Rotational instability was evaluated by the pivot-shift test before surgery and at the 3-, 6-, 12-, and 24-month follow-ups after surgery [6].
Radiographic evaluation and magnetic resonance imaging evaluation
The position and shape of the femoral and tibial tunnels were evaluated by the 3D-CT reconstruction images 1 day after surgery.
MRI was necessary to assess the maturity of the graft; the SNQ between the two groups at the 6-month, 1-year, and 2-year follow-ups was compared. All patients underwent MRI examinations using the same 1.5 T MRI scanner (GE Healthcare, USA) and the examinations were performed by the same technician. Signal intensity in three regions-of-interest (ROIs) of the ACL graft was measured independently in the sagittal oblique MR images: a. the proximal or femoral region, b. the middle or intra-articular region, and c. the distal or tibial region (area of each ROI circle = 0.05 cm2 by freehand). The background site was placed approximately 2 cm anterior to the patellar tendon. Each SNQ of the three ROIs was calculated by the following formula: SNQ = (signal of ROI – signal of quadriceps tendon)/signal of background. In addition, the mean SNQ of the graft was calculated by the following formula: SNQ g = (SNQ a + SNQ b + SNQ c)/3, which represented the maturity of the graft. A lower SNQ g value indicated lower water content in the graft, which indicated a more mature ACL graft [18, 37].
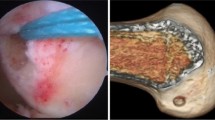
Second-look arthroscopic evaluation
Second-look arthroscopy was suggested at 2 years after surgery to compare the graft status and synovial coverage. The ACL graft evaluations were performed in accordance with the classification system described by Kondo and Yasuda [14], where the status was classified as A (intact), B (partial tear), or C (total tear) and the synovium coverage of the graft was graded as A (completely covered), B (partially covered), or C (barely covered).
Statistical analysis
Dichotomous or categorical variables were compared using the Chi-squared test. Student’s t-test was used for the analysis of the continuous variables after it was confirmed that the data met the normal distribution and homogeneity of variance assumptions. SPSS 24.0 (IBM SPSS Statistics 24) and bilateral test were used for the statistical analysis (p < 0.05). The results were expressed as the mean ± standard deviation (SD) or number (percent). An a priori sample size calculation was performed using software G-Power 3.1 (effect size 0.8, α-error 0.05, power 0.95) and a minimum of 35 subjects per group were recommended. To reach the recommended value, the size of the control group was increased considerably and the total sample size was also increased to account for any losses to follow-up.
Results
The clinical scores and knee stability in the two groups were significantly improved at the last postoperative follow-up, but there were some differences observed between the two groups. No significant difference was found in the preoperative IKDC score and Lysholm score between the two groups (ns). At the end of the follow-up period, the average Lysholm score was 97.1 in group 1, which was better than that in group 2 (94.8) (p = 0.031). The average IKDC subjective score was 92.0 and 89.0 in groups 1 and 2, respectively, at the end of the follow-up period (p < 0.001). Even though the preoperative KT1000 showed no significant difference between the two groups, the postoperative outcome was better in group 1 than in group 2 (p < 0.05). Both the preoperative and postoperative pain scores (visual analog scale, VAS) showed no statistically significant differences between the two groups and there was no use of analgesics among the participants in both groups during the follow-up period. At 1-year postoperatively, all the patients were able to flex their knees beyond 120 degrees and achieve full extension. At 2 years postoperatively, the ROM was same as that of the contralateral knee (ns) (Table 2).
No statistically significant differences were found in relation to the Lachman test between the two groups, even though there were more 1 + positive patients in group 2. More patients with 1-degree positive pivot-shift test results were observed in group 2 (10/65) than in group 1 (1/37) at the end of the follow-up period (p = 0.048) (Table 3).
While, the MRI scans showed no significant difference between the two groups at 6 months, significant differences were observed at 12 months and 24 months postoperatively. At the last postoperative follow-up, the mean SNQ of group 1 was 2.7 ± 0.9, which was significantly lower than that of group 2 (3.6 ± 1.1) (p = 0.000). A lower SNQ value indicated a more mature graft (Table 4).
Second-look arthroscopic evaluation
With respect to the graft status, in group 1, the ACL graft was graded as an A in 18 patients (94.7%) and a B in one patient (5.3%), while in group 2, it was graded as an A in 27 patients (87.1%) and a B in four patients (12.9%). The synovium coverage of group 1 was graded as an A in 17 patients (89.5%) and a B in two patients (10.5%) and in group 2, it was graded as an A in 24 patients (77.4%), a B in six patients (19.4%), and a C in one patient (3.2%). No significant differences between group 1 and 2 were found when evaluating the graft status or synovium coverage since some patients refused to receive second-look arthroscopy.
No complications, such as posterior femoral tunnel fractures, wound infections, cartilage lesions, difficult graft passage, or neurovascular injuries, occurred in either of the two groups. Two patients in group 1 and five in group 2 presented with redness and swelling of the surgical site and were managed conservatively. One patient in group 2 sustained a tibial tunnel fracture, which was immobilized with plaster and resumed rehabilitation 4 weeks later. One patient in group 1 had postoperative stiffness that later resolved with physiotherapy. There were no re-rupture cases at the last follow-up, as confirmed by the MRI scans. The entrance of the femoral tunnel in both groups was within the ACL anatomical footprint, as confirmed by 3D-CT (Fig. 3).
Discussion
The main finding of the present study was that the OFT technique was significantly superior to the conventional RFT technique regarding both the clinical outcomes and the MRI evaluations. The patients in the OFT group had better knee function and knee stability, which were consistent with the research findings of Noh et al. [24]. A lower SNQ value indicated a more mature graft in this study and the SNQ in group 1 was significantly lower than that in group 2.
In recent years, extensive research on ACL anatomy has been conducted; consequently, the flat ribbon concept for ACL and oval femoral footprints has been introduced. This is closely related to anatomical ACL reconstruction [22, 25, 29, 35, 36]. Siebold et al. found that the ACL has a flat and thin appearance and its cross section resembled a ribbon-like ligament with a mean width of 9.9 mm and thickness of 3.9 mm [33]. Sasaki et al. found that the proximal ACL fibers spread in a fanlike manner on the medial aspect of the lateral femoral condyle and that the femoral insertion had an oval shape [29]. Mochizuki et al. also reported that these fanlike extension fibers adhere to the femoral surface, on which the oval attachment margin is located [22]. Oshima et al. conducted a cadaveric study on semitendinosus tendon grafts and found that the cross-sectional shape of the femoral insertion side of the graft was an oval; therefore, the oval-tunnel technique proved to be superior to the round tunnel technique [25]. Studies have been conducted on the oval-tunnel technique in recent years to find a simple, safe, and effective surgical method for anatomical ACL reconstruction. Nakase et al. introduced an elliptically rounded rectangle femoral dilator used in single-bundle anatomic ACL reconstruction and the femoral tunnel entrance was confined within the ACL anatomical footprint [23]. Petersen et al. also presented a medial portal aimer and oval dilatators in the oval-tunnel ACL reconstruction technique. They found that the oval-tunnel matched the ACL anatomic insertion better than the round tunnel, but the authors did not include a clinical control group [26]. Noh et al. research showed that the Lysholm score in the oval-tunnel group was better than that in the conventional group at the end of the follow-up period; however, the precision to which the oval-tunnel technique was performed was not adequate [24].
In comparison to previous studies, this research has improved the surgical procedures and provided better follow-up information on clinical outcomes, MRI evaluations, and second-look arthroscopy. The clinical functional scores, knee stability, and ACL graft maturity were statistically superior in the oval-tunnel group than in the round-tunnel group at the 2-year postoperative follow-up. For graft maturity, the early follow-ups showed no significant difference between the two groups; however, the 1-year and 2-year follow-ups showed better graft maturity in the oval group than in the round group.
The following four theories were inferred and summarized to explain the superiority of the OFT technique to the conventional RFT technique. First, for the same diameter graft, the circumference of an oval graft is longer than a round graft, which provides a larger surface area for better blood supply from adjacent cancellous bone surrounding the femoral tunnel. Second, OFT closely resembles ACL anatomic femoral insertion and restores natural ACL morphology, as confirmed by the previous studies. Third, according to the principles of geometry, the grafts used in OFT should not easily rotate like the grafts used in RFT do, which can lead to instability and affect the tendon-bone healing process. This can be avoided by adapting the OFT to provide better rotational stability of the knee, as confirmed by the pivot-shift test results in this study. Forth, fixation of hamstring tendon grafts in the femoral tunnel is not only dependent on the RIGIDLOOP, but also on the compression of the graft against the cancellous bone of the femoral tunnel. OFT was gradually dilated by percussive compression, which ensured maximum preservation of cancellous bone, which was not supported by RFT. Because of the technical differences, the grafts used in OFT acquired better compression against the peri-tunnel cancellous bone and hence, there was better mechanical stability and a smaller possibility of tunnel widening [16, 21].
However, there were still some limitations in this study. First, this trial was a prospective non-randomized controlled study and the allocation of participants to groups was based on their hospital arrival time, which can increase the risk of bias. Second, the postoperative follow-up period was 2 years and did not account for long-term complications such as osteoarthritis and other possible complications. Third, the number of participants was relatively small, which reduces the reliability of the results of the experiment, especially for the graft evaluation in second-look arthroscopy. Forth, the graft tunnel position and shape were not identical to the ACL natural anatomy, even though the oval footprint was better than the round footprint in restoring the ACL femoral anatomy. Finally, although fractures of the posterior femoral tunnel did not occur in any of the participants, the gradual dilation of the oval tunnel by percussive compression was still a concern with the oval technique.
Conclusions
The hypothesis was supported by the results in this study; the oval femoral tunnel technique was superior to the round femoral tunnel technique clinically and radiologically. The results showed statistically significant differences between groups; nevertheless, both techniques provided good clinical and radiological outcomes. Based on the clinical evaluations, MRI findings and second-look arthroscopy results of the two groups, the oval femoral tunnel technique yielded significantly better knee function and knee laxity restoration and more mature ACL grafts than the round femoral tunnel technique, whereas no significant differences were found at the second-look arthroscopy.
References
Aga C, Kartus JT, Lind M, Lygre SHL, Granan LP, Engebretsen L (2017) Risk of revision was not reduced by a double-bundle acl reconstruction technique: results from the scandinavian registers. Clin Orthop Relat Res 475:2503–2512
Ahn JH, Kim JD, Kang HW (2015) Anatomic placement of the femoral tunnels in double-bundle anterior cruciate ligament reconstruction correlates with improved graft maturation and clinical outcomes. Arthroscopy 31:2152–2161
Bjornsson H, Andernord D, Desai N, Norrby O, Forssblad M, Petzold M et al (2015) No difference in revision rates between single- and double-bundle anterior cruciate ligament reconstruction: a comparative study of 16,791 patients from the Swedish national knee ligament register. Arthroscopy 31:659–664
Branch TP, Mayr HO, Browne JE, Campbell JC, Stoehr A, Jacobs CA (2010) Instrumented examination of anterior cruciate ligament injuries: minimizing flaws of the manual clinical examination. Arthroscopy 26:997–1004
Chen H, Chen B, Tie K, Fu Z, Chen L (2018) Single-bundle versus double-bundle autologous anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials at 5-year minimum follow-up. J Orthop Surg Res 13:50
Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM (2011) Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 63(Suppl 11):S208–S228
Dhawan A, Gallo RA, Lynch SA (2016) Anatomic tunnel placement in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 24:443–454
Fu FH, van Eck CF, Tashman S, Irrgang JJ, Moreland MS (2015) Anatomic anterior cruciate ligament reconstruction: a changing paradigm. Knee Surg Sports Traumatol Arthrosc 23:640–648
Grevnerts HT, Terwee CB, Kvist J (2015) The measurement properties of the IKDC-subjective knee form. Knee Surg Sports Traumatol Arthrosc 23:3698–3706
Hofbauer M, Muller B, Murawski CD, van Eck CF, Fu FH (2014) The concept of individualized anatomic anterior cruciate ligament (ACL) reconstruction. Knee Surg Sports Traumatol Arthrosc 22:979–986
Irarrazaval S, Albers M, Chao T, Fu FH (2017) Gross, Arthroscopic, and radiographic anatomies of the anterior cruciate ligament: foundations for anterior cruciate ligament surgery. Clin Sports Med 36:9–23
Kaeding CC, Leger-St-Jean B, Magnussen RA (2017) Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med 36:1–8
Komzak M, Hart R, Feranec M, Smid P, Kocova R (2018) In vivo knee rotational stability 2 years after double-bundle and anatomic single-bundle ACL reconstruction. Eur J Trauma Emerg Surg 44:105–111
Kondo E, Yasuda K (2007) Second-look arthroscopic evaluations of anatomic double-bundle anterior cruciate ligament reconstruction: relation with postoperative knee stability. Arthroscopy 23:1198–1209
Kraeutler MJ, Wolsky RM, Vidal AF, Bravman JT (2017) Anatomy and biomechanics of the native and reconstructed anterior cruciate ligament: surgical implications. J Bone Joint Surg Am 99:438–445
Lopes OV Jr, de Freitas SL, Leite LHC, Buzzeto BQ, Saggin PRF, Kuhn A (2017) Femoral tunnel enlargement after anterior cruciate ligament reconstruction using RigidFix compared with extracortical fixation. Knee Surg Sports Traumatol Arthrosc 25:1591–1597
Lu W, Zhu W, Peng L, Fen W, Li H, Ou Y et al (2015) Femoral footprint variation of the posterolateral bundle of the anterior cruciate ligament and double-bundle reconstruction. Knee 22:169–173
Ma Y, Murawski CD, Rahnemai-Azar AA, Maldjian C, Lynch AD, Fu FH (2015) Graft maturity of the reconstructed anterior cruciate ligament 6 months postoperatively: a magnetic resonance imaging evaluation of quadriceps tendon with bone block and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc 23:661–668
Mayr HO, Benecke P, Hoell A, Schmitt-Sody M, Bernstein A, Suedkamp NP et al (2016) Single-bundle versus double-bundle anterior cruciate ligament reconstruction: a comparative 2-year follow-up. Arthroscopy 32:34–42
McLean SG, Mallett KF, Arruda EM (2015) Deconstructing the anterior cruciate ligament: what we know and do not know about function, material properties, and injury mechanics. J Biomech Eng 137:020906
Mermerkaya MU, Atay OA, Kaymaz B, Bekmez S, Karaaslan F, Doral MN (2015) Anterior cruciate ligament reconstruction using a hamstring graft: a retrospective comparison of tunnel widening upon use of two different femoral fixation methods. Knee Surg Sports Traumatol Arthrosc 23:2283–2291
Mochizuki T, Fujishiro H, Nimura A, Mahakkanukrauh P, Yasuda K, Muneta T et al (2014) Anatomic and histologic analysis of the mid-substance and fan-like extension fibres of the anterior cruciate ligament during knee motion, with special reference to the femoral attachment. Knee Surg Sports Traumatol Arthrosc 22:336–344
Nakase J, Toratani T, Kosaka M, Ohashi Y, Numata H, Oshima T et al (2016) Technique of anatomical single bundle ACL reconstruction with rounded rectangle femoral dilator. Knee 23:91–96
Noh JH, Yang BG, Roh YH, Kim SW, Kim W (2011) Anterior cruciate ligament reconstruction using 4-strand hamstring autograft: conventional single-bundle technique versus oval-footprint technique. Arthroscopy 27:1502–1510
Oshima T, Nakase J, Numata H, Takata Y, Tsuchiya H (2016) The cross-sectional shape of the fourfold semitendinosus tendon is oval, not round. J Exp Orthop 3:28
Petersen W, Forkel P, Achtnich A, Metzlaff S, Zantop T (2013) Technique of anatomical footprint reconstruction of the ACL with oval tunnels and medial portal aimers. Arch Orthop Trauma Surg 133:827–833
Petersen W, Zantop T (2007) Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res 454:35–47
Pugh L, Mascarenhas R, Arneja S, Chin PY, Leith JM (2009) Current concepts in instrumented knee-laxity testing. Am J Sports Med 37:199–210
Sasaki N, Ishibashi Y, Tsuda E, Yamamoto Y, Maeda S, Mizukami H et al (2012) The femoral insertion of the anterior cruciate ligament: discrepancy between macroscopic and histological observations. Arthroscopy 28:1135–1146
Schillhammer CK, Reid JB 3rd, Rister J, Jani SS, Marvil SC, Chen AW et al (2016) Arthroscopy up to date: anterior cruciate ligament anatomy. Arthroscopy 32:209–212
Sepulveda F, Sanchez L, Amy E, Micheo W (2017) Anterior cruciate ligament injury: return to play, function and long-term considerations. Curr Sports Med Rep 16:172–178
Shimizu R, Adachi N, Ishifuro M, Nakamae A, Ishikawa M, Deie M et al (2017) Bone tunnel change develops within two weeks of double-bundle anterior cruciate ligament reconstruction using hamstring autograft: a comparison of different postoperative immobilization periods using computed tomography. Knee 24:1055–1066
Siebold R, Schuhmacher P, Fernandez F, Smigielski R, Fink C, Brehmer A et al (2015) Flat midsubstance of the anterior cruciate ligament with tibial "C"-shaped insertion site. Knee Surg Sports Traumatol Arthrosc 23:3136–3142
Slattery C, Kweon CY (2018) Classifications in brief: outerbridge classification of chondral lesions. Clin Orthop Relat Res 476:2101–2104
Smigielski R, Zdanowicz U, Drwiega M, Ciszek B, Ciszkowska-Lyson B, Siebold R (2015) Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: a cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc 23:3143–3150
Smigielski R, Zdanowicz U, Drwiega M, Ciszek B, Williams A (2016) The anatomy of the anterior cruciate ligament and its relevance to the technique of reconstruction. Bone Joint J 98-b:1020–1026
Tanaka Y, Yonetani Y, Shiozaki Y, Kanamoto T, Kita K, Amano H et al (2014) MRI analysis of single-, double-, and triple-bundle anterior cruciate ligament grafts. Knee Surg Sports Traumatol Arthrosc 22:1541–1548
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
van Meer BL, Meuffels DE, Vissers MM, Bierma-Zeinstra SM, Verhaar JA, Terwee CB et al (2013) Knee injury and Osteoarthritis Outcome Score or International Knee Documentation Committee Subjective Knee Form: which questionnaire is most useful to monitor patients with an anterior cruciate ligament rupture in the short term? Arthroscopy 29:701–715
Wang W, Liu L, Chang X, Jia ZY, Zhao JZ, Xu WD (2016) Cross-cultural translation of the Lysholm knee score in Chinese and its validation in patients with anterior cruciate ligament injury. BMC Musculoskelet Disord 17:436
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Ethical approval
Ethical approval was obtained from the Institutional Review Board (IRB) of the First Affiliated Hospital of Chongqing Medical University (ID 2016-178).
Informed consent
In this prospective non-randomized controlled study, informed consent was obtained from all the patients regarding the details of the study and all possible complications related to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 18911 kb)
Supplementary file2 (MP4 14711 kb)
Rights and permissions
About this article
Cite this article
Wen, Z., Zhang, H., Yan, W. et al. Oval femoral tunnel technique is superior to the conventional round femoral tunnel technique using the hamstring tendon in anatomical anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 28, 2245–2254 (2020). https://doi.org/10.1007/s00167-019-05809-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05809-4