Abstract
Purpose
To compare the position and direction of femoral and tibial tunnels for both the anteromedial bundle (AMB) and posterolateral bundle (PLB) among three different femoral tunnel drilling techniques, transtibial (TT), transportal (TP), and outside-in (OI) techniques, in anatomic double-bundle ACL reconstruction to clarify advantages and disadvantages of each technique.
Methods
One-hundred and thirty-nine patients underwent primary ACL reconstruction with an autologous semitendinosus tendon in our institution between 2014 and 2016. Thirteen patients were excluded according to the exclusion criteria. Of the 126 patients, 98 patients agreed to be included in this study. Patients were then randomized into three groups according to the femoral tunnel drilling technique; the TT, TP, and OI groups. Femoral and tibial tunnel angles and positions were measured using three-dimensional computed tomography.
Results
Of patients who agreed to be included in this study, eight patients (seven in TT and one in OI) were excluded since the femoral tunnel could not be created at the intended position. Eighty-six patients (29 in TT, 29 in TP, and 28 in OI) were included for the analyses. Tunnel angles, as well as tunnel lengths, had significant differences among different techniques depending on each technique’s characteristics. In terms of tunnel position, femoral tunnel positions of both the AMB and PLB in the TT group were significantly higher than those in the TP group (AMB: p = 0.003, PLB: p = 0.001), and the PLB tunnel position in the TP group had significantly smaller vaciance than that in the TT group (p = 0.004) and OI group (0.002).
Conclusions
The femoral tunnel positions created by the TT technique were significantly higher, with larger variance, than the TP technique in double-bundle ACL reconstruction, although the positions seemed to be within anatomical footprint. In addition, there were several cases in which femoral tunnels could not be created at the intended position by the TT technique.
Level of evidence
I
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although the recent concept of anatomic anterior cruciate ligament (ACL) reconstruction has been advanced and surgical techniques have improved, the procedure still suffers from impingement, graft maturation, tunnel widening, and tunnel malposition. One of the biggest reasons for failure of ACL reconstruction is non-anatomical tunnel replacement. It has been known that non-anatomical tunnel placement causes increasing graft stress and leads to graft loosening [30]. Therefore, accurate tunnel placements for both the femur and tibia are essential to obtain good clinical outcomes. It has been shown that the femoral tunnel position affects graft tension and isometricity more significantly than the tibial tunnel position [16, 37, 51], and that the femoral tunnel positioning is correlated with clinical outcomes after ACL reconstruction [1, 20, 34, 47]. Besides, tibial tunnel position is also important in terms of knee stability, revision rate, meniscus preservation and risk of graft impingement [4, 9, 21, 43].
There are three common techniques used to create femoral tunnels: the transtibial (TT) technique, transportal (TP) technique, and outside-in (OI) technique for double-bundle ACL reconstruction. Some surgeons adopted the TT technique due to the ease of the procedure, reduction in surgical time, rigid fixation, and low rate of graft failure [2, 46, 48]. However, some studies have reported on the difficulty of anatomical femoral tunnel placement with use of the TT technique if the knee flexion angle is not controlled during drill guide positioning, as femoral tunnel position is strictly regulated by tibial tunnel position and angle [3, 7, 11, 13, 18, 19, 30, 38, 42, 49, 52]. The TP technique allows more flexibility for anatomic femoral tunnel placement, whereas it suffers from difficulty in visualization, short femoral tunnel length, and acute graft tunnel angle [45]. The OI technique allows better visualization and independent femoral tunnel creation from the tibial tunnel position with longer femoral tunnel length, whereas the graft-bending angle in a knee extended position at the intra articular aperture is more acute with the OI technique than with the TP technique [23].
To the best of our knowledge, there has been no study comparing three femoral tunnel drilling techniques in a prospective randomized controlled trial with the same concept in tunnel positions. The purpose of this study was to compare the position and direction of femoral and tibial tunnels for both the anteromedial bundle (AMB) and posterolateral bundle (PLB) among three different femoral tunnel drilling techniques in anatomic double-bundle ACL reconstruction using a three-dimensional computed tomography (3D-CT), to clarify advantages and disadvantages of each technique. The hypotheses underlying this study were that tunnel angles would differ among different techniques, and it would be comparatively more difficult to create femoral tunnels at the anatomic position using the TT technique than others.
Materials and methods
Collection of the baseline data was made at Tokyo Medical and Dental University between 2014 and 2016. The inclusion criterium was primary isolated ACL reconstruction with an autologous semitendinosus tendon. Exclusion criteria included concomitant ligament tears, history of injuries in the ipsilateral knee, history of ligamentous injuries in the contralateral knee, and knees with osteoarthritis that showed obvious joint space narrowing in the preoperative radiographs (Kellgren–Lawrence grade 3 and 4) [24]. Patients were then randomized by a fellow surgeon, by means of a computer-generated list of random numbers, into three groups based on the femoral tunnel drilling technique, the TT technique (TT group), TP technique (TP group) and OI technique (OI group). Patients were blinded to the surgical procedure. This study was part of a randomized controlled trial comparing clinical outcomes after ACL reconstruction among three different femoral tunnel drilling techniques.
Surgical technique
The ACL reconstruction procedure was performed by two attending surgeons or under their supervision. There were no significant differences regarding distribution of the surgeons among the groups (n.s.).
A standard arthroscopic examination was performed via anteromedial and anterolateral portals. A ruptured ACL was confirmed arthroscopically, and meniscal injury was managed according to the injury status. Only the semitendinosus tendon was harvested, and the harvested tendon was cut into halves and folded, creating two double-stranded bundles of 5.5 cm or more in length looped with EndoButton CL-BTB (Smith & Nephew Endoscopy, Andover, MA). There were no significant differences among the three groups in graft diameter of both femoral and tibial sides for the AMB and PLB. In each technique, the remnant tissue of the ruptured ACL at the tibial side was not removed at all for tibial tunnel creation. For femoral tunnel creation, we used the behind-remnant approach, in which the femoral tunnel creation was performed without any removal of the remnant tissue with arthroscopic observation behind the remnant tissue from the anteromedial portal [29, 35, 36]. The guide wire for the PLB was aimed at the distal end and posterior border of the direct insertion of the remnant tissue with approximately a 5-mm margin from the articular surface distally and posteriorly. The guide wire for the AMB was aimed at the posterior border of the direct insertion of the remnant tissue with approximately a 5-mm margin from the articular surface proximally and posteriorly.
Transtibial technique
Two tibial guide wires were inserted from the anteromedial surface of the tibia at approximately 10 mm above the tibia tubercle level with anatomical landmarks of the ruptured ACL remnant and medial intercondylar eminence using ACUFEX Director Tip Aimer (Smith & Nephew Endoscopy). For the AMB tunnel, the tibial aimer was set at an angle of 50°, and the guide wire was aimed 3 mm posterior to the anterior margin of the ACL remnant and just lateral to the medial intercondylar eminence at an angle of 60° from the joint line in the anterior–posterior radiographic view. For the PLB tunnel, the tibial aimer was set at an angle of 45°, and the guide wire for the PLB was aimed just anterior and lateral to the spine of the medial intercondylar eminence at an angle of 50° from the joint line in the anterior–posterior radiographic view. The angles and directions of the tibial tunnels were extremely critical for achieving the anatomic femoral position using the TT technique.
Guide wires for the femoral drill holes were inserted via the transtibial tunnel approach in the figure-of-four position. For both the AMB and PLB guide wire insertion, the insertion point was identified and the tip of the guide wire was inserted with the knee at 90° flexion, and the guide wire was advanced through the lateral cortex at 110° flexion to avoid the posterior blowout of the lateral femoral condyle. 4.5-mm-diameter tunnels with 25-mm-long femoral sockets were then created. Both grafts were inserted and were fixed with the EndoButton CL-BTB. Each graft was fixed to an anchor staple with sutures at the tibial site at 20° of flexion. Applied tension to each graft was adjusted to be on a basis of 25 N per 6 mm diameter, so that both bundles had equal-stress tension [10, 28].
Transportal technique
A medial accessory portal was made as inferior (close to the meniscofemoral border of the medial meniscus) and as medial (without the risk of cartilage damage on the medial femoral condyle) as possible. Guide wires for the femoral drill holes were inserted via the medial accessory portal in the figure-of-four position. For both guide wire insertions, the insertion point was identified and the tip of the guide wire was inserted with the knee at 90° flexion, and the guide wire was advanced through the lateral cortex at 130° flexion [38]. Femoral tunnel creation was then made in the same manner as in the TT technique. Tibial tunnels were created after femoral tunnel creation, in the same manner as in the TT technique, except for the angles of the tibial aimer. The tibial aimer was set at an angle of 60° for the AMB and 55° for the PLB to avoid the risk of cartilage damage on the medial tibial plateau. Graft introduction and fixation were made in the same manner as in the TT technique.
Outside-in technique
For femoral guide wire insertion, an Antero-Lateral Entry Femoral Aimer (Smith and Nephew Endoscopy) was used and was set at an insertion angle of 10° for the AMB and 0° for the PLB. The angle of the femoral tunnel in relation to the joint line was aimed at 40° for the AMB and 30° for the PLB in the axial plane. For both AMB and PLB tunnels, with the knee at 90° flexion, a guide wire was introduced from the lateral femoral cortex, overdrilled using an EndoDrill, and replaced by a FlipCutter (Arthrex, Naples, FL), creating a femoral socket with a diameter matched with the graft diameter. Tibial tunnel creation along with graft introduction and fixation were made in the same manner as in the TP technique.
Femoral tunnel length
During surgery, femoral tunnel length for each technique was measured using a depth gauge in 1 mm increments after femoral tunnel creation. The femoral tunnel length was then compared among the groups. As there was no significant difference in height of the patients (Table 1), absolute values of the femoral tunnel length were compared, instead of normalized values by height of the patients.
Radiological assessments
Three weeks after the surgery, axial computed tomography (CT) scans with coronal, sagittal, and three-dimensional (3D) reconstructions of the operated knee in an extended position were obtained to assess the bone tunnel location. All radiological measurements were performed by two orthopaedic surgeons who were blinded to the surgical procedures.
Femoral and tibial tunnel angles
Bone tunnel angles of each tunnel in the coronal, sagittal, and axial planes were measured on the CT images in 0.1° increments. In each plane, an image that showed the tunnel aperture and subsequent tunnel was selected for both femur and tibia. In the coronal planes of the femur and the tibia, the angles between the AMB and PLB tunnels and each joint surface were measured (Fig. 1a). In the sagittal plane of the femur, the angles between the femoral shaft axis and the AMB and PLB tunnels were measured. In the sagittal plane of the tibia, the angles between the tibial joint surface and the AMB and PLB tunnels were measured (Fig. 1b). In the axial planes of the femura and the tibia, the angles between the AMB and PLB tunnels and the line that linked each posterior condyle were measured (Fig. 1c) [22]. Analysis of inter-observer reliability yielded an intra-class correlation coefficient of 0.974 (95% confidence interval 0.946–0.988) for the femoral tunnel angle and 0.931 (95% confidence interval; 0.855–0.967) for the tibial tunnel angle.
Femoral tunnel positions
The sagittal view of the 3D-CT with neutral rotation of the lateral femoral condyle was used, and the centers of the femoral tunnels of the AMB and PLB were assessed according to the quadrant method described by Bernad et al. [6]. The total sagittal diameter of the lateral condyle along Blumensaat's line and maximum intercondylar notch height were measured. The distance from the center of the AMB and PLB to the most dorsal subchondral contour of the lateral femoral condyle (depth) and the distance from the center of the AMB and PLB to Blumensaat's line (height) were expressed in percentages in 0.1% increments (Fig. 2a). Analysis of inter-observer reliability yielded an intra-class correlation coefficient of 0.922 (95% confidence interval 0.769–0.974) for the femoral tunnel position.
Tunnel positions. A Femoral tunnel position. Height and depth of the tunnel position were assessed by 3D-CT according to the quadrant method. a, the distance from the center of the tunnel to the most dorsal subchondral contour of the lateral femoral condyle; b, the distance from the center of the tunnel to Blumensaat's line; c the total sagittal diameter of the lateral condyle along Blumensaat's line; d, maximum intercondylar notch height. B Tibial tunnel position. The anterior-to-posterior and medial-to-lateral tunnel positions were determined by 3D-CT. e, the distance from the anterior border of the tibial plateau to the center of the tunnel; f, the distance from the anterior border to the posterior border of the tibial plateau; g, the distance from the medial border of the tibial plateau to the center of the tunnel; h, the distance from the medial border to the lateral border of the tibial plateau
Tibial tunnel positions
With use of a true proximal-to-distal view on the tibial plateau of 3D-CT, the anterior-to-posterior and medial-to-lateral tunnel positions were determined as shown in Fig. 2b in 0.1% increments. Anterior-to-posterior positions were calculated as percentages of the distance from the anterior border to the posterior border of the tibial plateau per the distance from the anterior border of the tibial plateau to the center of each tunnel. Medial-to-lateral positions were calculated as percentages of the distance from the medial border to the lateral border of the tibial plateau per the distance from the medial border of the tibial plateau to the center of each tunnel [13]. Analysis of inter-observer reliability yielded an intra-class correlation coefficient of 0.986 (95% confidence interval 0.965–0.994) for the tibial tunnel position.
This study was approved by the institutional review board of Tokyo Medical and Dental University (Research protocol identification number: 1842) and was registered at UMIN-CTR (Study identification number: UMIN000015515). Informed consent was obtained from all individual participants included in the study.
Statistical analysis
Statistical analysis was performed using the SPSS 21.0 software package (SPSS Inc., Chicago, IL) and Graphpad prism (GraphPad Software, San Diego, CA). Between-group differences of the means were calculated by the Kruskal–Wallis test and Dunn’s multiple comparisons test, and frequency distributions by the χ2 test. The Bartlett’s test was used to compare the variances of the femoral tunnel position among the three groups, and the F test was used for between-group comparison. Case 2 intra-class correlation coefficients were used to evaluate the inter-observer reliability. As already mentioned, this study was part of a randomized controlled trial comparing clinical outcomes after ACL reconstruction among three different femoral tunnel drilling techniques; therefore, statistical power was first calculated base on the clinical outcome. Power analysis, with a power of 80% and an alpha of 0.05, demonstrated that a sample size of 24 patients in each group was needed for a 1.0-mm difference with 1.2-mm standard deviation in KT measurements. Considering 20% of lost follow-up, the number of patients in each group was set to 30. Particularly for this study, post hoc power analysis revealed that, with an alpha of 0.05, a power of 0.95 was achieved for the differences in the height of the AMB, and a power of 0.97 was achieved for the differences in the height of the PLB. For all analyses, statistical significance was set at p < 0.05. All data were reported as mean ± standard deviation (SD), unless indicated otherwise.
Results
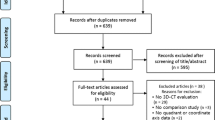
A total of 139 consecutive patients met the inclusion criteria, and 13 patients were excluded according to the exclusion criteria. Of the 126 patients, 98 patients agreed to be included in this randomized controlled trial; they were randomized into 3 groups based on the femoral tunnel drilling technique as shown in Fig. 3. However, eight patients were excluded because of the technical failure; femoral tunnels could not be created at the intended position by the TT technique in seven patients (changed to the TP technique in four patients and to the OI technique in three patients), and by the OI technique in one patient (changed to the TP technique). Technical failure rate in the TT group was significantly higher than other groups (p = 0.009). Among them, four were lost to obtain CT (1, 1, and 2 in the TT, TP, and OI groups, respectively) and were excluded for the analysis (Fig. 3). There were no significant differences in the demographic data and surgical time (from tunnel creation to femoral side graft fixation) among the three groups, as shown in Table 1.
Femoral tunnel length
Femoral tunnel lengths for both the AMB and PLB in the TP group were significantly shorter than those in other groups (Table 2).
Tunnel angles
Mean angles of the AMB and PLB tunnels in the femur and tibia are shown in Tables 3, 4 and 5. In the coronal plane (Table 3), femoral tunnel angle of the AMB in the TT group was significantly larger than that in other groups. On the other hand, tibial tunnel angles of both the AMB and PLB in the TT group were significantly smaller than those in the OI group. In the sagittal plane (Table 4), femoral tunnel angles of both the AMB and PLB in the TP group were significantly smaller than those in other groups. On the other hand, tibial tunnel angles of both the AMB and PLB in the TT group were significantly smaller than those in other groups. In the axial plane (Table 5), femoral tunnel angles of both the AMB and PLB in the TP group were significantly smaller than those in other groups.
Femoral tunnel positions
Femoral tunnel positions of the AMB and PLB are shown in Table 6 and Fig. 4. Tunnel positions of both the AMB and PLB in the TT group were significantly higher than those in the TP group. Comparison of the variances showed that the PLB tunnel position in the TT group had significantly larger variance than that in the TP group.
Average tunnel positions of the AMB and PLB in the transtibial (TT), transportal (TP) and outside-in (OI) groups. a Femoral tunnel positions. Tunnel positions of both the AMB and PLB in the TT group were significantly higher than those in the TP group, and the PLB tunnel position in the TT group had significantly larger variance than that in the TP group. b Tibial tunnel positions. Tunnel positions of both the AMB and PLB in the TT group were significantly more anterior than those in other groups
Tibial tunnel positions
Tibial tunnel positions of the AMB and PLB are shown in Table 7 and Fig. 4. Tunnel positions of both the AMB and PLB in the TT group were significantly more anterior than those in other groups.
Discussion
The most important findings of the current study were that the femoral tunnel positions created by the TT technique tended to be higher than other techniques, although the positions seemed to be within anatomical footprint on the CT images. In addition, there were several cases in which femoral tunnels could not be created at the intended position by the TT technique.
This is the first study investigating tunnel positions and angles among the three different femoral tunnel drilling techniques in a prospective randomized controlled trial with the same concept in tunnel positions. Therefore, the intended positions for both the femur and tibia were supposed to be consistent in this study. In particular, we created the tibial tunnels by the TT technique with smaller angles in sagittal and coronal planes to create femoral tunnels within anatomic position, since femoral tunnel position was strictly regulated by tibial tunnel position and angle. Nevertheless, femoral tunnel positions of both the AMB and PLB in the TT group were significantly higher than those in the TP group, and the PLB tunnel position in the TT group had significantly larger variance than that in the TP group. In addition, in 7 out of 37 cases, femoral tunnels could not be created at the intended position by the TT technique, and we had to change to other techniques to achieve anatomic femoral tunnel position. Although femoral tunnel positions by the TT technique in the current study were not shallower than other techniques and seemingly were still within anatomical footprint of the native ACL [14, 26, 31, 39, 50], these results are in good agreement with previous studies, showing that femoral tunnel position by the TT technique tended to be higher and shallower compared to other techniques [14, 39, 41]. These findings suggest that the TT technique is the most technically demanding, and sometimes it is difficult to create femoral tunnel at the anatomic position by the TT technique.
The TP technique is the most flexible technique to create femoral tunnels, since femoral and tibal tunnels are independent. However, in the current study, use of the TP technique resulted in shorter femoral tunnel length with smaller angles in all three planes compared to other techniques. The TP technique is apt to have a shorter femoral tunnel length compared to the TT [5, 15, 17, 32] and the OI [26, 40] techniques without deep knee flexion during tunnel creation, especially in small patients [12, 38, 44], leading to insufficient length of graft insertion in the femoral tunnel with unstable fixation using buttons [27]. In addition, smaller femoral tunnel angles by the TP technique can lead to posterior-wall blowout and potential damage to the posterior articular cartilage [8, 14, 25, 40].
The OI technique is the most adjustable technique with wider selection for tunnel positioning. Advantages of this technique enable femoral tunnel positions to be created within anatomic ACL footprint [33, 41]. On the other hand, since this technique requires more complicated steps than other techniques, surgeons should be familiar with detailed tips and pitfalls of this technique. Sometimes the outside-in guide shape does not fit to the intercondylar notch, leading to difficulty in stabilizing the guide. Also, the guide wire could be placed at an unintended position. In the current study, femoral tunnels could not be created at the intended position by the the OI technique in one patient and had to be changed to the TP technique.
There are several limitations in this study. First, in some radiographic images, there was difficulty in plotting the central position of femoral aperture. Most of the tunnels in the CT slice were in the shape of an ellipse and the center of the tunnel on the image was plotted, but it might not have been exactly in the middle depending on the shape of the bone. However, analysis of inter-observer reliability yielded an intra-class correlation coefficient of 0.922 for the femoral tunnel position and 0.986 for the tibial tunnel position, although intra-observer reliability was not evaluated. Second, this study only determined tunnel positions just after the surgery. This model does not consider any tunnel expansion or translation that might occur after the surgery. Third, this model does not consider any clinical findings. Further follow-up study investigating the effects of femoral tunnel drilling technique on clinical findings are necessary, and this study is actually a part of a randomized controlled trial.
For clinical relevance, it is important to recognize advantages and disadvantages of each technique for femoral tunnel drilling. Optimally, surgeons should be familiar with all the techniques so that the most appropriate technique can be applied to each patient to take full advantage of the technique.
Conclusions
The femoral tunnel positions created by the TT technique tended to be higher, with larger variance, than the TP and OI techniques in double-bundle ACL reconstruction, although the positions seemed to be within anatomical footprint. In addition, there were several patients in which femoral tunnels could not be created at the intended position by the TT technique.
References
Abebe ES, Kim JP, Utturkar GM et al (2011) The effect of femoral tunnel placement on ACL graft orientation and length during in vivo knee flexion. J Biomech 44:1914–1920
Ahn JH, Lee SH, Yoo JC, Ha HC (2007) Measurement of the graft angles for the anterior cruciate ligament reconstruction with transtibial technique using postoperative magnetic resonance imaging in comparative study. Knee Surg Sports Traumatol Arthrosc 15:1293–1300
Arnold MP, Kooloos J, van Kampen A (2001) Single-incision technique misses the anatomical femoral anterior cruciate ligament insertion: a cadaver study. Knee Surg Sports Traumatol Arthrosc 9:194–199
Bedi A, Maak T, Musahl V et al (2011) Effect of tibial tunnel position on stability of the knee after anterior cruciate ligament reconstruction: is the tibial tunnel position most important? Am J Sports Med 39:366–373
Bedi A, Musahl V, Steuber V et al (2011) Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy 27:380–390
Bernard M, Hertel P, Hornung H, Cierpinski T (1997) Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg 10:14–21
Cha PS, Brucker PU, West RV et al (2005) Arthroscopic double-bundle anterior cruciate ligament reconstruction: an anatomic approach. Arthroscopy 21:1275
Chang MJ, Chang CB, Won HH, Je MS, Kim TK (2013) Anteromedial portal versus outside-in technique for creating femoral tunnels in anatomic anterior cruciate ligament reconstructions. Arthroscopy 29:1533–1539
Chiba D, Tsuda E, Tsukada H, Iio K, Ishibashi Y (2017) Tunnel malpositions in anterior cruciate ligament risk cartilaginous changes and bucket-handle meniscal tear: arthroscopic survey in both primary and revision surgery. J Orthop Sci 22:892–897
Conner CS, Morris RP, Vallurupalli S, Buford WL Jr, Ivey FM (2008) Tensioning of anterior cruciate ligament hamstring grafts: comparing equal tension versus equal stress. Arthroscopy 24:1323–1329
Dargel J, Schmidt-Wiethoff R, Fischer S, Mader K, Koebke J, Schneider T (2009) Femoral bone tunnel placement using the transtibial tunnel or the anteromedial portal in ACL reconstruction: a radiographic evaluation. Knee Surg Sports Traumatol Arthrosc 17:220–227
Farrow LD, Liu RW (2010) Lateral anatomic structures at risk during transepiphyseal anterior cruciate ligament reconstruction. J Knee Surg 23:209–213
Forsythe B, Kopf S, Wong AK et al (2010) The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Jt Surg Am 92:1418–1426
Gadikota HR, Sim JA, Hosseini A, Gill TJ, Li G (2012) The relationship between femoral tunnels created by the transtibial, anteromedial portal, and outside-in techniques and the anterior cruciate ligament footprint. Am J Sports Med 40:882–888
Geng Y, Gai P (2018) Comparison of 2 femoral tunnel drilling techniques in anterior cruciate ligament reconstruction. A prospective randomized comparative study. BMC Musculoskelet Disord 19:454
Giron F, Cuomo P, Aglietti P, Bull AM, Amis AA (2006) Femoral attachment of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 14:250–256
Guglielmetti LGB, Shimba LG, do Santos LC et al (2017) The influence of femoral tunnel length on graft rupture after anterior cruciate ligament reconstruction. J Orthop Traumatol 18:243–250
Harner CD, Honkamp NJ, Ranawat AS (2008) Anteromedial portal technique for creating the anterior cruciate ligament femoral tunnel. Arthroscopy 24:113–115
Heming JF, Rand J, Steiner ME (2007) Anatomical limitations of transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med 35:1708–1715
Hosseini A, Lodhia P, Van de Velde SK et al (2012) Tunnel position and graft orientation in failed anterior cruciate ligament reconstruction: a clinical and imaging analysis. Int Orthop 36:845–852
Inderhaug E, Raknes S, Ostvold T, Solheim E, Strand T (2017) Increased revision rate with posterior tibial tunnel placement after using the 70-degree tibial guide in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 25:152–158
Inoue M, Tokuyasu S, Kuwahara S et al (2010) Tunnel location in transparent 3-dimensional CT in anatomic double-bundle anterior cruciate ligament reconstruction with the trans-tibial tunnel technique. Knee Surg Sports Traumatol Arthrosc 18:1176–1183
Kambara S, Nakayama H, Yamaguchi M et al (2017) Comparison of transportal and outside-in techniques for posterolateral femoral tunnel drilling in double-bundle ACL reconstruction -three-dimensional CT analysis of bone tunnel geometry. J Orthop Sci 22:481–487
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kim JG, Chang MH, Lim HC, Bae JH, Ahn JH, Wang JH (2013) Computed tomography analysis of the femoral tunnel position and aperture shape of transportal and outside-in ACL reconstruction: do different anatomic reconstruction techniques create similar femoral tunnels? Am J Sports Med 41:2512–2520
Kim JG, Wang JH, Lim HC, Ahn JH (2012) Femoral graft bending angle and femoral tunnel geometry of transportal and outside-in techniques in anterior cruciate ligament reconstruction: an in vivo 3-dimensional computed tomography analysis. Arthroscopy 28:1682–1694
Kim KI, Lee SH, Bae C, Bae SH (2017) Three-dimensional reconstruction computed tomography evaluation of the tunnel location and angle in anatomic single-bundle anterior cruciate ligament reconstruction: a comparison of the anteromedial portal and outside-in techniques. Knee Surg Relat Res 29:11–18
Koga H, Muneta T, Yagishita K et al (2015) Effect of initial graft tension on knee stability and graft tension pattern in double-bundle anterior cruciate ligament reconstruction. Arthroscopy 31:1756–1763
Koga H, Muneta T, Yagishita K et al (2015) Evaluation of a behind-remnant approach for femoral tunnel creation in remnant-preserving double-bundle anterior cruciate ligament reconstruction—comparison with a standard approach. Knee 22:249–255
Kopf S, Forsythe B, Wong AK et al (2010) Nonanatomic tunnel position in traditional transtibial single-bundle anterior cruciate ligament reconstruction evaluated by three-dimensional computed tomography. J Bone Jt Surg Am 92:1427–1431
Larson AI, Bullock DP, Pevny T (2012) Comparison of 4 femoral tunnel drilling techniques in anterior cruciate ligament reconstruction. Arthroscopy 28:972–979
Lubowitz JH (2009) Anteromedial portal technique for the anterior cruciate ligament femoral socket: pitfalls and solutions. Arthroscopy 25:95–101
Lubowitz JH, Akhavan S, Waterman BR, Aalami-Harandi A, Konicek J (2013) Technique for creating the anterior cruciate ligament femoral socket: optimizing femoral footprint anatomic restoration using outside-in drilling. Arthroscopy 29:522–528
Markolf KL, Hame S, Hunter DM et al (2002) Effects of femoral tunnel placement on knee laxity and forces in an anterior cruciate ligament graft. J Orthop Res 20:1016–1024
Muneta T, Koga H, Nakamura T, Horie M, Watanabe T, Sekiya I (2016) Behind-remnant arthroscopic observation and scoring of femoral attachment of injured anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 24:2906–2914
Muneta T, Koga H, Nakamura T et al (2015) A new behind-remnant approach for remnant-preserving double-bundle anterior cruciate ligament reconstruction compared with a standard approach. Knee Surg Sports Traumatol Arthrosc 23:3743–3749
Muneta T, Yamamoto H, Sakai H, Ishibashi T, Furuya K (1993) Relationship between changes in length and force in in vitro reconstructed anterior cruciate ligament. Am J Sports Med 21:299–304
Nakamae A, Ochi M, Adachi N, Deie M, Nakasa T (2012) Clinical comparisons between the transtibial technique and the far anteromedial portal technique for posterolateral femoral tunnel drilling in anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 28:658–666
Nakamura T, Koga H, Otabe K et al (2019) Comparison of three approaches for femoral tunnel during double-bundle anterior cruciate ligament reconstruction: a case controlled study. J Orthop Sci 24:147–152
Park JS, Park JH, Wang JH et al (2015) Comparison of femoral tunnel geometry, using in vivo 3-dimensional computed tomography, during transportal and outside-in single-bundle anterior cruciate ligament reconstruction techniques. Arthroscopy 31:83–91
Robert HE, Bouguennec N, Vogeli D, Berton E, Bowen M (2013) Coverage of the anterior cruciate ligament femoral footprint using 3 different approaches in single-bundle reconstruction: a cadaveric study analyzed by 3-dimensional computed tomography. Am J Sports Med 41:2375–2383
Robin BN, Jani SS, Marvil SC, Reid JB, Schillhammer CK, Lubowitz JH (2015) Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: a systematic review. Arthroscopy 31:1412–1417
Saito K, Hatayama K, Terauchi M, Hagiwara K, Higuchi H, Takagishi K (2015) Clinical outcomes after anatomic double-bundle anterior cruciate ligament reconstruction: comparison of extreme knee hyperextension and normal to mild knee hyperextension. Arthroscopy 31:1310–1317
Siebold R, Axe J, Irrgang JJ, Li K, Tashman S, Fu FH (2010) A computerized analysis of femoral condyle radii in ACL intact and contralateral ACL reconstructed knees using 3D CT. Knee Surg Sports Traumatol Arthrosc 18:26–31
Takeda Y, Iwame T, Takasago T et al (2013) Comparison of tunnel orientation between transtibial and anteromedial portal techniques for anatomic double-bundle anterior cruciate ligament reconstruction using 3-dimensional computed tomography. Arthroscopy 29:195–204
Volpi P, Denti M (2008) Double-bundle reconstruction of the anterior cruciate ligament using the transtibial technique. Arthroscopy 24:1190–1194
Xu Y, Ao Y, Wang J, Yu J, Cui G (2011) Relation of tunnel enlargement and tunnel placement after single-bundle anterior cruciate ligament reconstruction. Arthroscopy 27:923–932
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22:240–251
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Zantop T, Wellmann M, Fu FH, Petersen W (2008) Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med 36:65–72
Zavras TD, Race A, Amis AA (2005) The effect of femoral attachment location on anterior cruciate ligament reconstruction: graft tension patterns and restoration of normal anterior-posterior laxity patterns. Knee Surg Sports Traumatol Arthrosc 13:92–100
Zelle BA, Vidal AF, Brucker PU, Fu FH (2007) Double-bundle reconstruction of the anterior cruciate ligament: anatomic and biomechanical rationale. J Am Acad Orthop Surg 15:87–96
Acknowledgments
We thank Atsushi Okawa, MD, PhD for continuous support, Miyoko Ojima for management of our department and Ronald G. Berisle for English correction.
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Tokyo Medical and Dental University institutional review board (Research protocol identification number: 1842) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakamura, K., Nakamura, T., Horie, M. et al. Anatomic femoral tunnel placement is difficult by the transtibial technique: comparison of three different femoral tunnel drilling techniques in double-bundle anterior cruciate ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 28, 584–593 (2020). https://doi.org/10.1007/s00167-019-05740-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05740-8