Abstract
Purpose
This study examined the influence of the mechanical medial proximal tibial angle (MPTA) on anterior cruciate ligament (ACL) degeneration following open wedge high tibial osteotomy (OWHTO). It was hypothesised that an excessive increase in MPTA would be associated with ACL degeneration following OWHTO.
Methods
Seventy-four knees treated with OWHTO were retrospectively examined. Arthroscopic ACL grading [0 (intact) to 4 (complete rupture)], anterior tibial translation (ATT) test at the time of OWHTO with the index arthroscopy and at plate removal with the second-look arthroscopy, clinical assessments using the Knee Society Score (KSS), and radiographic evaluations of MPTA were performed. The relationship between MPTA and the ACL condition was analysed using Spearman’s correlation.
Results
The time from the index arthroscopy to the second-look arthroscopy was 15.0 ± 4.4 months; the total follow-up was 31.0 ± 6.5 months. ACL grade significantly increased from 0.6 ± 0.8 (index arthroscopy) to 1.1 ± 1.2 (second-look arthroscopy) (p < 0.0018). ATT on the operated side significantly decreased from 7.1 ± 2.6 mm preoperatively to 5.3 ± 2.3 mm at the time of plate removal (p < 0.001). No significant difference was observed in KSS for ACL grades in the steady and progression groups. Changes in MPTA from the preoperative to postoperative period were significantly higher in the progression group (p = 0.0155). Changes in ACL grades were significantly correlated with preoperative MPTA and changes in MPTA (r = − 0.365 and 0.343, respectively; p < 0.01).
Conclusions
Excessively increased MPTA led to ACL degeneration following OWHTO. ACL degeneration was not associated with short-term clinical outcomes. Excessive correction of MPTA should be avoided to prevent ACL degeneration following OWHTO.
Level of evidence
Therapeutic case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medial open wedge high tibial osteotomy (OWHTO) is associated with an unintentional increase in the posterior tibial slope angle (PTSA) [6, 13, 19, 20, 22, 25]. An unintentional increase in PTSA could lead to the anterior translation of the tibial plateau [1, 10, 15, 27]. This could increase the strain on the anterior cruciate ligament (ACL), resulting in ACL degeneration. Because ACL dysfunction is considered to be one of the risk factors for knee osteoarthritis [7], appropriate control of the PTSA could be important for the long-term success of OWHTO. However, recently, it has been reported that OWHTO reduces coronal tibiofemoral subluxation, which is lateral subluxation of the proximal tibia relative to the distal femur during progression of knee osteoarthritis, and that coronal tibiofemoral subluxation is correlated with the mechanical medial proximal tibial angle (MPTA) [4, 24]. When reducing the lateral coronal tibiofemoral subluxation in OWHTO, the distance between the origin and the insertion of the ACL increases in the coronal plane; consequently, the medial–lateral component of the strain on the ACL might increase, resulting in ACL degeneration. However, the influence of MPTA on ACL degeneration following OWHTO has not been investigated. Therefore, this study was designed to analyse the relationship between MPTA and ACL conditions following OWHTO. This clarification could provide knowledge about a permissible range of MPTA in OWHTO from the point of view of the ACL condition. It was hypothesised that an excessive increase in MPTA would be associated with ACL degeneration following OWHTO.
Materials and methods
This retrospective study was approved by the institutional review board of Gifu University Graduate School of Medicine (No. 27–100). Written informed consent for participation in the study was obtained from all patients. Patients who had undergone OWHTO at our institution between October 2014 and August 2016 were eligible for study inclusion. The surgical indications were as follows: medial compartment knee osteoarthritis or spontaneous osteonecrosis of the knee diagnosed via radiography and magnetic resonance imaging; impaired performance of activities of daily living due to persistent knee pain after at least 3 months of conservative treatment; presence of the centre of the deformity around the proximal tibia; < 15° of flexion contracture; and a bony correction angle requirement of < 15°, as calculated preoperatively. The exclusion criteria were complete rupture of the ACL at the index arthroscopy and a lack of second-look arthroscopy evaluations.
Surgical technique and postoperative rehabilitation
The surgical technique and preoperative planning used in the present study were described previously [23]. The postoperative mechanical axis was designed to pass across the knee at the Fujisawa point (a point at 62.5% of the cross-sectional diameter of the tibial plateau) according to Miniaci’s method [9, 18]. Before the OWHTO, arthroscopic microfracture surgery of the knee was used to treat articular cartilage lesions in all patients. The biplanar OWHTO was internally fixed with a TomoFix osteotomy system (DePuy Synthes, Zuchwil, Switzerland) or Tris medial HTO plate system (Olympus Terumo Biomaterials, Tokyo, Japan) with two β-tricalcium phosphate wedge spacers (Osferion60, Olympus Terumo Biomaterials) [14, 30, 31]. The length of the posterior aspect of the medial gap was recorded.
Patients were allowed partial and full weight-bearing on postoperative days 7 and 14, respectively.
Clinical evaluation
Preoperative patient data, including age, sex, and Body Mass Index (BMI), were recorded. Clinical outcomes were evaluated using the Knee Society Score (KSS; total knee score, and total function score) preoperatively and at the latest follow-up examination.
Arthroscopic assessment of ACL
The ACL was arthroscopically graded according to the original ACL grading system created by the authors that ranged from 0 to 4 points (Fig. 1) during the index arthroscopy at OWHTO and during the second-look arthroscopy at the time of plate removal.
Anterior tibial translation test
The anterior tibial translation (ATT) test was performed with a KS Measure Arthrometer (Sigmax Medical, Tokyo, Japan) under general anaesthesia during the index arthroscopy and second-look arthroscopy according to a previously validated method [17]. The relative movement between the patella and tibial tubercle sensor pads was recorded with 30 pounds at 30° of flexion, which was confirmed with a goniometer. One observer performed all of the tests to eliminate interobserver variation. Measurements were performed three times, and the mean value of the three measurements was used.
Radiographic evaluation
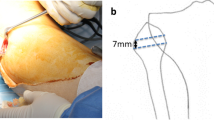
Radiographic parameters, including the percentage of the weight-bearing line (%WBL) [9], MPTA, and Kellgren–Lawrence (K-L) grades [12], were evaluated preoperatively and at the latest follow-up (Fig. 2).
Radiographic assessments. %Weight-bearing line (%WBL): %WBL is a percentage calculated by the formula b/a × 100% on full-length standing anteroposterior radiographs of the lower extremity (a). a: width of the tibial plateau, b: horizontal distance from WBL to the medial edge of the tibial plateau. Mechanical medial proximal tibial angle (MPTA): MPTA is defined as the angle between the tibial plateau and the tibial mechanical axis (b)
Statistical analysis
Two independent observers performed all radiographic measurements twice with an interval of more than 1 day in a blinded manner. The intra-rater and inter-rater reliabilities for determining the radiographic parameters, ACL grade, and ATT test results were expressed as intraclass correlation coefficients (ICC; two-way mixed effects model) that varied from 0 (no agreement) to 1 (total agreement). Statistical comparisons were performed using SPSS version 13.0 (SPSS Inc., Chicago, IL). Tests to determine normality and distribution were performed using the Kolmogorov–Smirnov test. Student’s t test was used to analyse parametric data. Spearman’s correlation analysis was used to assess the correlation between MPTA and the changes in the ACL grade and ATT. A post hoc power analysis for correlation was performed using G*Power version 3.0.3 to determine the statistical power. The statistical power for the correlation analysis between the ACL grade and the radiographic parameters was 0.85, with an effect size of 0.3, an alpha of 0.05, and a sample size of 75. The significance level was set at p < 0.05 for all analyses.
Results
Of 79 consecutive OWHTO from October 2014 to August 2016, 5 were excluded because of complete rupture of the ACL at the index arthroscopy (n = 4) and the absence of plate removal concomitant with second-look arthroscopy (n = 1). Consequently, 74 knees of 67 patients were analysed during this study. The mean period from the index arthroscopy to the second-look arthroscopy was 14.9 ± 4.5 months (range 8–29 months), and the mean total follow-up period was 30.0 ± 6.5 months (range 20–46 months). Age, sex, BMI, and opening gap at the osteotomy site of the patients are summarised in Table 1.
Arthroscopic assessment of the ACL and ATT test
There was no history of any trauma related to the ACL injury for all patients during the study period. The average ACL grade significantly increased from 0.6 ± 0.8 at the index arthroscopy to 1.1 ± 1.2 at the second-look arthroscopy (p = 0.0018). Severe grades of 3 and 4 for partial or complete ACL rupture were found in 9 cases (12.2%) at the second-look arthroscopy compared to one case (1.4%) at the index arthroscopy (Fig. 3). The knees for which the ACL grade increased from the index arthroscopy to second-look arthroscopy by at least one grade (progression group) were compared with knees with no such noted increase (steady group). Although there was no significant difference in the average ACL grade at the index arthroscopy [not significant (NS)], the average ACL grade of the progression group was significantly higher than that of the steady group at the second-look arthroscopy (p < 0.0001) (Table 2). The inter-rater and intra-rater reliability for ACL grading were 0.98 and 0.97, respectively. The average ATT on the operated side significantly decreased from 7.1 ± 2.6 mm preoperatively to 5.3 ± 2.3 mm at the time of plate removal (p < 0.0001); however, no such decrease was noted on the non-operated side (Table 3). There was no significant difference in the change in ATT on the operated side between the preoperative and postoperative periods (NS) or between the steady and progression groups (NS) (Table 2). The intra-rater reliability for the ATT test was 0.92.
KSS
Overall, the KSS (both total knee score and total function score) significantly improved postoperatively (p < 0.0001 for each). However, there was no significant difference in the scores of the steady group and progression group at the latest follow-up (NS) (Table 4).
Radiographic evaluation
The %WBL significantly improved from 13.1 ± 18.7% (range − 45–48%) preoperatively to 60.9 ± 7.8% (range 44–79%) at the latest follow-up (p < 0.0001). MPTA significantly increased from 84.6 ± 2.8° (range 77.9°–91.9°) preoperatively to 93.5 ± 3.3° (range 86.5°–100.9°) postoperatively (p < 0.001). Moreover, the change in MPTA from the preoperative to postoperative period (ΔMPTA) was significantly higher in the progression group than in the steady group (p = 0.0155) (Table 2). There was no significant difference in KL grades for the medial compartment of the knee at the index arthroscopy (3.1 ± 0.6) and at the second-look arthroscopy (3.1 ± 0.8) (NS). Inter-rater reliability more than 0.92 and intra-rater reliability more than 0.89 were obtained for the radiographic measurements.
Correlation of change in the ACL grade and MPTA
Spearman’s correlation analysis showed a significant correlation between the change in the ACL grade (ΔACL grade) and preoperative MPTA (r = − 0.365; p < 0.01) and ΔMPTA (r = 0.343; p < 0.01), but not with postoperative MPTA (NS) (Table 5).
Discussion
The most important finding in this study was that an increase in MPTA was significantly correlated with ACL degeneration following OWHTO. In addition, anteroposterior stability of the tibia significantly increased after OWHTO regardless of MPTA.
Information regarding the influence of OWHTO on ACL is limited. Some biomechanical studies showed that an increase in PTSA can be a major risk factor for ACL rupture [10, 16], suggesting the importance of avoiding an unintentional increase in PTSA during OWHTO. However, the influence of MPTA on ACL degeneration following OWHTO is unclear. OWHTO is a realignment surgery performed for the lower limb; during this surgery, MPTA is increased. Valgus MPTA not only shifts the load distribution from the medial to the lateral compartment of the knee but also reduces lateral coronal tibiofemoral subluxation [4, 24]. With this reduction, the distance between the origin and the insertion of the ACL might increase in the coronal plane; subsequently, the tension on the ACL might increase. This repeated tension effect may explain why the anterior laxity of the tibia was improved after OWHTO, as shown by the ATT test results; furthermore, repeated tension of the ACL may increase anteroposterior stability of the tibia.
The evidence that the degree of MPTA is correlated with the reduction of lateral coronal tibiofemoral subluxation (medial shift of the tibia relative to the femur) [24] strongly implies that MPTA is also correlated with the magnitude of strain on the ACL because reduction of the subluxation directly stretches the ACL in the coronal plane. In fact, in the current study, the ΔMPTA was higher for ACL degeneration in the progression group than in the steady group (Table 2). Furthermore, the ΔACL grade was correlated with the ΔMPTA (Table 5). MPTA increased during OWHTO; subsequently, this might induce the reduction of lateral coronal tibiofemoral subluxation and repeated tension of the ACL. Because the magnitude of the strain on the ACL depends on the degree of MPTA, an excessive increase in MPTA may lead to ACL degeneration. However, because shortening of the medial collateral structure and stretching on the lateral side occurs when a varus deformity exceeds 10° [5], OWHTO might also change the balance of the bilateral collateral ligaments by reducing varus deformity and coronal tibiofemoral subluxation, which might also affect ACL conditions. Unless the ACL ruptures due to strain beyond its limit, it is tense and stabilises the knee during OWHTO. This could be why the ATT test showed significantly stabilised knees after OWHTO; it could also be why OWHTO did not affect the approximately 2.5-year short-term clinical outcomes observed during the present study. However, because patients with an ACL injury are at significantly higher risk for a secondary meniscal tear, osteoarthritis, and total knee arthroplasty [21, 28], excessively high MPTA should be avoided to prevent ACL degeneration following OWHTO to achieve good long-term results.
The ideal postoperative alignment for OWHTO is unknown. Because there are many opinions about the indications for OWHTO [3, 11, 29], postoperative alignment must be customised to the need of the patient [8]. Some studies suggested that marked overcorrection into the valgus might not be necessary because even neutral mechanical alignment leads to decreased loading of the medial compartment [2, 26]. However, our results suggest that excessive valgus correction induces ACL degradation. An individualised decision regarding the minimum amount of valgus correction should be established based on pathology and cartilage conditions.
There were some limitations to this study that must be appreciated when interpreting the findings. First, how ACL grade 4 affects clinical outcomes remains unclear because the follow-up period was short and the number of patients with ACL grade 4 following OWHTO was small. Second, the influence of the degree of PTSA on ACL degeneration was not investigated, which may have affected the ACL conditions. Because high PTSA is a risk factor for ACL degeneration, the effect of the relationship of MPTA and PTSA on ACL conditions should be comprehensively investigated. Third, this study was retrospective. Therefore, further prospective, randomized, clinical trials are warranted.
Conclusion
The magnitude of the MPTA change is correlated with ACL degeneration following OWHTO. However, OWHTO stabilised anterior tibial translation regardless of ACL degeneration, and this degeneration was not associated with short-term clinical outcomes.
References
Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P (2004) Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg 124:575–584
Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P (2007) The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 23(8):852–861
Amis AA (2013) Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):197–205
Akamatsu Y, Ohno S, Kobayashi H, Kusayama Y, Kumagai K, Saito T (2016) Coronal subluxation of the proximal tibia relative to the distal femur after opening wedge high tibial osteotomy. Knee 24:70–75
Bellemans J, Vandenneucker H, Vanlauwe J, Victor J (2010) The influence of coronal plane deformity on mediolateral ligament status: an observational study in varus knees. Knee Surg Sports Traumatol Arthrosc 18(2):152–156
Brouwer RW, Bierma-Zeinstra SM, van Koeveringe AJ, Verhaar JA (2005) Patellar height and the inclination of the tibial plateau after high tibial osteotomy. The open versus the closed-wedge technique. J Bone Jt Surg Br 87:1227–1232
Delincé P, Ghafil D (2012) Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc 20:48–61
Feucht MJ, Minzlaff P, Saier T, Cotic M, Südkamp NP, Niemeyer P, Imhoff AB, Hinterwimmer S (2014) Degree of axis correction in valgus high tibial osteotomy: proposal of an individualised approach. Int Orthop 38(11):2273–2280
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin N Am 10:585–608
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32:376–382
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Jt Surg Am 69(3):332–354
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
LaPrade RF, Oro FB, Ziegler CG, Wijdicks CA, Walsh MP (2010) Patellar height and tibial slope after opening-wedge proximal tibial osteotomy: a prospective study. Am J Sports Med 38:160–170
Lobenhoffer P, Agneskirchner JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11:132–138
Marti CB, Gautier E, Wachtl SW, Jakob RP (2004) Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy 20:366–372
Marouane H, Shirazi-Adl A, Adouni M, Hashemi J (2014) Steeper posterior tibial slope markedly increases ACL force in both active gait and passive knee joint under compression. J Biomech 47:1353–1359
Matsumoto K, Ogawa H, Yoshioka H, Akiyama H (2017) Postoperative anteroposterior laxity influences subjective outcome after total knee arthroplasty. J Arthroplast 32:1845–1849
Miniaci A, Ballmer FT, Ballmer PM, Jakob RP (1989) Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res 246:250–259
Noyes FR, Barber-Westin SD, Hewett TE (2000) High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 28:282–296
Noyes FR, Goebel SX, West J (2005) Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med 33:378–387
Noyes FR, Matthews DS, Mooar PA, Grood ES (1983) The symptomatic anterior cruciate-deficient knee. Part II: the results of rehabilitation, activity modification, and counseling on functional disability. J Bone Jt Surg Am 65:163–174
Ogawa H, Matsumoto K, Akiyama H (2018) New angle measurement device to control the posterior tibial slope angle in medial opening wedge high tibial osteotomy. Arch Orthop Trauma Surg 138:299–305
Ogawa H, Matsumoto K, Akiyama H (2017) The prevention of a lateral hinge fracture as a complication of a medial opening wedge high tibial osteotomy: a case control study. Bone Jt J 99-B:887–893
Ogawa H, Matsumoto K, Akiyama H (2018) Coronal tibiofemoral subluxation is correlated to correction angle in medial opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-4948-9
Ogawa H, Matsumoto K, Ogawa T, Takeuchi K, Akiyama H (2016) Effect of wedge insertion angle on posterior tibial slope in medial opening wedge high tibial osteotomy. Orthop J Sports Med 4:2325967116630748
Riegger-Krugh C, Gerhart TN, Powers WR, Hayes WC (1998) Tibiofemoral contact pressures in degenerative joint disease. Clin Orthop Relat Res 348:233–245
Rodner CM, Adams DJ, Diaz-Doran V, Tate JP, Santangelo SA, Mazzocca AD et al (2006) Medial opening wedge tibial osteotomy and the sagittal plane: the effect of increasing tibial slope on tibiofemoral contact pressure. Am J Sports Med 34:1431–1441
Sanders TL, Pareek A, Kremers HM, Bryan AJ, Levy BA, Stuart MJ et al (2017) Long-term follow-up of isolated ACL tears treated without ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 25:493–500
Smith JO, Wilson AJ, Thomas NP (2013) Osteotomy around the knee: evolution, principles and results. Knee Surg Sports Traumatol Arthrosc 21(1):3–22
Staubli AE, De Simoni C, Babst R, Lobenhoffer P (2003) TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia–early results in 92 cases. Injury 34(Suppl 2):B55–B62
Staubli AE, Jacob HA (2010) Evolution of open-wedge high-tibial osteotomy: experience with a special angular stable device for internal fixation without interposition material. Int Orthop 34:167–172
Funding
No external funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Rights and permissions
About this article
Cite this article
Ogawa, H., Matsumoto, K. & Akiyama, H. ACL degeneration after an excessive increase in the medial proximal tibial angle with medial open wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 27, 3374–3380 (2019). https://doi.org/10.1007/s00167-019-05354-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05354-0