Abstract
Purpose
Extrusion of the medial meniscus evaluated on magnetic resonance imaging (MRI) has been described as indirect radiological sign for meniscus root tears. However, ultrasound detectable dynamic extrusion is observed in normal physiological settings. The aim of the present study was to analyze the dynamic meniscal extrusion using ultrasound (US) examination in patients with MRI-confirmed meniscal root tears. The hypothesis was that dynamic meniscus extrusion is reduced in patients with medial root tear but not in the healthy meniscus.
Methods
Twenty-five patients with a medial root lesion of the meniscus (group I) and 25 healthy controls (group II) were enrolled in this study. The medial meniscus extrusion (MME) of the index knee was determined using ultrasound (US) in supine position and under full weight bearing. Standard knee MRI was used for determining whether the patients were eligible for this study according to the inclusion and exclusion criteria, respectively.
Results
In group I, the mean MME was 3.6 mm (± 1.0 mm) in supine position and 3.7 mm (± 0.9 mm) under full weight bearing according to US measurements. The mean Δ-extrusion was 0.1 mm (± 0.2 mm) and the ratio was 1.0 (± 0.1). Mean medial meniscus extrusion on MRI was 3.9 mm (± 0.9 mm). In group II, mean MME was 1.3 mm (± 0.3 mm) in supine position (US) and 2.3 mm (± 0.4 mm) under full weight bearing (US). The mean Δ-extrusion was 1.0 mm (± 0.4 mm) and the extrusion ratio was 1.8 (± 0.4). In this group, mean extrusion in MRI was 1.4 mm (± 0.7 mm). The difference in mean ultrasound Δ-extrusion, ratio, and MRI extrusion between both groups was statistically significant (p < 0.001).
Conclusions
Based on the results of dynamic ultrasound examination of the medial meniscus, medial root tear leads to significantly decreased dynamic medial displacement of the meniscus compared to healthy meniscus status. The absence of dynamic meniscus extrusion may be an indicator for medial meniscus root injury and could be detected using ultrasound (“dead meniscus sign”).
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The wedge-shaped menisci improve the congruity of femur and tibia and provide uniform distribution of load across the articular surfaces, wherein the roots of the menisci play an important role [9, 10, 20, 22, 31]. The normal forces applied to the menisci tend to cause radial meniscus extrusion [20]. The menisci are unable to extrude radially, since the four chondral insertion sites firmly attach the medial and lateral meniscus, respectively, to the anterior and posterior tibial intercondylar region. By this mechanism, the radially acting normal forces are transmitted in a circular hoop stress which is transferred to the insertions of the menisci [20, 22].
A root tear is defined as a complete radial lesion typically observed at the posterior insertion zones of the medial and lateral meniscus [21, 22, 30]. This lesion interrupts the circular hoop tension and leads to extrusion of the meniscus [22]. Radial extrusion of the meniscus is considered to increase the peak contact pressure within the joint. Allaire et al. [2] demonstrated that, in the medial compartment, a posterior root tear of the medial meniscus caused a 25% increase in peak contact pressure compared with that found in the intact condition. This effect was comparable to a total medial meniscectomy [2].
Meniscus extrusion is a typical finding in magnetic resonance imaging (MRI) of patients with medial root tears [22]. The meniscus is considered extruded when it extends beyond the tibial margin. Moreover, meniscus extrusion is not a specific sign for a medial meniscus root tear. Substantial medial meniscus extrusion (> 3 mm) is associated with severe meniscal degeneration, extensive tear, complex tear, or large radial tears, respectively [6]. Numerous researchers consider MRI as the gold standard for evaluation of meniscus extrusion [5, 6, 8, 13, 14, 22], although meniscus extrusion can be detected using ultrasound [1]. A previous study demonstrated that meniscus extrusion may not always be a pathological finding. In knees of healthy volunteers, a mean meniscus extrusion of 1.1 mm was detected in supine position [1]. During full weight bearing, mean medial meniscus extrusion increased to 1.9 mm [1]. The difference in extrusion (Δ-extrusion 0.8 mm) between supine and standing position was described as dynamic extrusion [1]. An explanation for this phenomenon can be observed in the viscoelasticity of the meniscal tissue [20]. In specific, axial load causes a temporal limited, reversible deformation of the meniscus [7]. The collagenous fibers of the meniscus elongate like a spring and subsequently increase the hoop stress [1]. After unloading, the meniscus returns back to its original position. Therefore, not only an increased meniscus extrusion may be regarded as pathologic, but also a decreased or absent functional adaption reaction of the meniscus [1]. The literature provides little data in terms of dynamic meniscus extrusion under pathological conditions such as a root tear. This raises the question of whether the dynamic extrusion is restricted as a consequence to insufficient fixation of the menisci at the tibial plateau. To cast a light on this matter, the present study investigated dynamic meniscus extrusion in knees of patient with MRI-confirmed medial root tears and a healthy matched control group. Based on the findings of previous MRI studies, it was hypothesized that patients with a medial meniscus root tear will display increased meniscus extrusion in the supine and standing position, but a smaller dynamic meniscus extrusion. The detection of meniscus extrusion using ultrasound could improve the early diagnosis of root tear lesions as well as evaluation following surgical repair or replacement.
Materials and methods
From March 2017 till December 2017, patients with medial root tear on MRI were enrolled in this prospective study. Inclusion criteria comprise age > 18 years and the radiological proof of a medial meniscus root lesion on MRI. The ghost sign, also known as empty meniscus sign [25], was chosen as radiological criteria for a root lesion, since it can indicate a complete disruption of the circular meniscus fibers (Fig. 1). Exclusion criteria comprise radiological signs of osteoarthritis > grade 2 according to Kellgren and Lawrence classification [12], clinical signs of severe valgus deformity (> 2 cm malleolar distance), and patients with German language barrier. Furthermore, patients diagnosed with other meniscus lesions (> Stoller III) or ligament instability were also excluded [26, 27]. Twenty-five patients consisting of 11 female and 14 male were included in the study. Age-matched healthy volunteers with no history of knee pain and > 18 years, facing the same exclusion criteria, served as control group, comprising 12 female and 13 male. For age matching, 4 age groups were defined (50–54, 55–59, 60–64 and 65–70 years, respectively). Healthy was defined as no episode of knee pain during the last 3 months and no previous knee surgery. The distribution of age, gender, and body mass index (BMI) between root tear group (group I) and healthy control group (group II) is presented in Table 1.
Clinical examination
For the healthy controls, age, weight, and length measurements were obtained and BMI was calculated subsequently. All patients were examined according to the International Knee Documentation Committee (IKDC). Menisci were evaluated by joint space tenderness and McMurray test. Examination of ligamentous instability included testing of the anterior and posterior cruciate ligament as well as medial (MCL) and lateral (LCL) collateral ligaments, respectively. Lower limb alignment was assessed clinically by measuring the distance between the condyles, respectively between both ankles with the patient standing upright. The distance between medial condyles and medial malleoli was measured by a single investigator with the caliper method. A malleolar distance of more than 2 cm was interpreted as valgus deformity. This method has been evaluated by Hinman et al. [10]. The authors have shown that the caliper method, that is quantifying the intercondylar and intermalleolar distances with a caliper, is a valid measuring method of the mechanical axis with a good correlation to the mechanical axis measured on whole-leg radiographs [10].
Ultrasound imaging (US)
The extrusion of the medial meniscus on the index knee was examined using ultrasound, which has previously been described by Achtnich et al. [1]. Previously, an intraclass correlation (ICC) for US measurements of 0.783 (CI [0.625; 0.872]; p < 0.001) in supine position and 0.900 (CI [0.820; 0.942]; p < 0.001) for full weight bearing in healthy human knees was demonstrated [1].
For this purpose, the medial femoral epicondyle of the patient was palpated and a favorable setting at the medial joint space was initially selected in the supine patient. A linear scanner of a 13.5 MHz ultrasound device (Sonosite, Siemens, Bothell, WA, USA) was placed parallel to the fiber orientation of the MCL. The meniscus presented as a hypo-echoic triangular structure between the femoral and tibial cortex. The proximal tibia impressed with a reflection phenomenon with sound cancelation. Extrusion was defined as the distance between a tangent line parallel to the fiber orientation of the MCL at the margin of the medial tibial cortex and the outermost edge of the medial meniscus previously described by Nogueira-Barbosa et al. (Fig. 2) [18]. The position of the receiving transducer was marked on the skin and the patient was, thereafter, asked to stand upright with balanced weight bearing on both legs. The transducer was again placed at the previously marked position and the meniscus extrusion was measured in the above described method. The difference of extrusion was calculated as well as the ratio by dividing the above-mentioned determined extrusion in standing position by the medial meniscus extrusion in supine position in millimeters (mm). The ultrasound device was able to show the measurements with two digits behind the comma.
Unloaded ultrasound image of the medial meniscus of a patient with a posterior root lesion. One dotted line is positioned at the border of the medial tibial cortex and one at the outermost edge of the medial meniscus. Meniscus extrusion is defined as the distance between both lines (distance e, A–A′). 1 = femur, 2 = tibia
Magnetic resonance imaging (MRI)
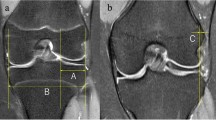
Digital MRI images were used to detect medial meniscus root lesion and additional injuries of the joint or degenerative changes. All acquired images of the knee were evaluated on picture archiving and communication system workstations (PACS, Agfa, Ridgefield Park, NJ, USA). For measurements, coronal proton density-weighted images with spectral fat suppression were chosen where the medial femoral epicondyle was fully visible. Calculation of the extrusion of the medial meniscus was performed according to Costa et al. [5]. One vertical line was placed at the outermost edge of the medial meniscus and one vertical line at the margin of the medial tibial plateau. The distance between both lines was quantified and defined as the meniscus extrusion in millimeter (mm) (Fig. 3).
Measurement of meniscus extrusion on a coronal “MRI” section in a patient with a medial meniscus root tear. One dotted line is positioned at the border of the medial tibia and one at the outermost edge of the medial meniscus. Meniscus extrusion is defined as the distance between both lines (e). In this patient, a tibial bone marrow edema is visible (white arrow)
The MRI images were scanned for other typical findings in patients with medial root lesions such as bone marrow edema (Fig. 3), effusion, cartilage damage, and linear defect. Cartilage damage was evaluated using a modified Outerbridge classification for MRI [27].
US images and MRI were evaluated in the above described methods by the senior author who is experienced in this field of area (WP).
The study was approved by the institutional review board of Technical University Munich, (no. 370/16 S) and conducted according to the Declaration of Helsinki. All subjects gave their written informed consent to participate in this investigation.
Statistical analysis
Statistical analysis was performed by Ulrike von Hehn (medistat, Kiel, Germany) using SPSS software (SPSS, Chicago, IL). For all statistical tests, p values less than 0.05 were considered as significant. A power analysis was performed based on a previous study [1] using G*Power 3.1.9.2 (medistat, Kiel, Germany). Mean extrusion for supine and loaded condition and standard deviation (SD) were calculated. With an effect size of 0.74, an α of 0.05, and a minimum of 22 subjects, the power of the current study is 0.8. For the description of the patient collective, the t test for independent samples was used for age, the Mann–Whitney U test was used for BMI and the Chi-square test for gender. Descriptive statistics are presented as mean ± SD if not otherwise stated. For comparison of the ultrasound findings between the groups, the Kolmogorov–Smirnov and Shapiro–Wilk tests were used to confirm normal distribution. The t test for independent samples was used to detect possible group differences of extrusion. The Mann–Whitney U test was used to detect group difference in the measurements of extrusion for supine position, Δ-extrusion, and ratio between the groups.
Results
Ultrasound
In the root tear group, mean MME was 3.6 mm (± 1.0 mm) in the supine position. In the standing position, mean MME increased to 3.7 mm (± 0.9 mm). The mean Δ-extrusion was 0.1 mm (± 0.2 mm) and the ratio was 1.0 (± 0.1).
In the control group, mean MME was 1.3 mm (± 0.3 mm) in the supine position and increased to 2.3 mm (± 0.4 mm) under bipedal standing with full weight bearing (Fig. 4). The mean Δ-extrusion in this group was 1.0 mm (± 0.4 mm) and the extrusion ratio was 1.8 (± 0.4) (Fig. 5). The difference in mean ultrasound Δ-extrusion and ratio between the root tear and control group was statistically significant (p < 0.001).
Mean ultrasound meniscus extrusion in the unloaded (a) and loaded (b) state of the medial root tear and the control group. a Significant group difference (*) was detected in the measurement of extrusion in supine position (U test, p < 0.001). b Significant group difference (*) was also confirmed in the measurements of extrusion standing (t test for independent samples, p < 0.001)
MRI
All patients of the root tear group presented with a posterior ghost sign on MRI (Fig. 1). In the majority of patients of the root tear group, meniscus extrusion of more than 3 mm could be detected on MRI with a mean MME of 3.9 mm (± 0.9 mm). Eighteen patients of the root tear group had bone marrow edema on the proximal tibia and/or distal femur (Fig. 3). In the control group, no patient presented with a ghost sign and mean extrusion in MRI was 1.4 mm (± 0.7 mm). No subchondral edema was observed in the control group. The difference in mean extrusion between the root tear group and the control group was statistically significant (p < 0.001) (Fig. 6).
Discussion
The most important finding of the present study is that medial meniscal root tear leads to significantly increased medial meniscus extrusion by overall reduced radial mobility of the meniscus compared to healthy meniscus status. Patients with medial root tears (group I) demonstrated a significantly higher absolute meniscus extrusion compared to healthy patients (group II), whereas no significant dynamic extrusion (Δ-extrusion) was detectable. In group II, meniscus extrusion was significantly lower in supine position as compared with the standing position.
Originally, meniscus extrusion was described as a phenomenon in MRI observed in patients with knee osteoarthritis (OA) [4, 8]. On MRI, an extrusion > 3 mm is considered pathological [1, 6, 22]. Several studies indicate that pathological medial meniscus extrusion is a predictor for progression of knee OA [4, 8, 11, 19].
It is widely accepted that medial meniscus extrusion is associated with meniscus root tears [9, 10, 13,14,15, 22, 30]. The roots of the menisci play an important role in maintaining circumferential hoop tension and preventing medial displacement [10, 13,14,15, 22]. If the meniscus root is completely detached from the tibia plateau, the medial meniscus is displaced medially under load [3, 28]. Therefore, pathological extrusion is considered to be an indirect MRI sign of a root tear [22]. Furthermore, the ghost sign is a typical finding on MRI in patients with a root tear lesion of the meniscus [25] (Fig. 1). Costa et al. [6] detected root tears in 42% of patients having a major medial extrusion > 3 mm MRI. In the study by Choi et al. [5], the mean meniscus extrusion on MRI for root tears was 3.8 mm ± 1.4 mm. This value is comparable to the 3.9 mm ± 0.9 mm extrusion on MRI found in the present study.
The biomechanical consequence of medial meniscus displacement is a significant increase in loads in the medial compartment as described by Allaire et al. [2]. The clinical consequence of this overload is bone marrow edema in the subchondral bone of the femur and tibia [22] (Fig. 3). Some studies have shown that posterior medial root tears and extrusion are associated with spontaneous osteonecrosis of the knee [23, 27].
In addition, the literature provides information of meniscus extrusion in physiological setting. Subsequently, meniscus extrusion should not always be regarded as a pathological finding [1, 11, 19, 24]. In specific, a certain degree of meniscal extrusion occurs with knee joint movement in the physiological state [29]. Rowland et al. [24] used ultrasound to assess the lateral meniscus in cadaver knees in unloaded and static axial load (70 kg) conditions, respectively. In this study, significant differences in extrusion were noted between loaded and unloaded state. Using ultrasound measurements, Achtnich et al. [1] demonstrated that medial meniscus extrusion is an age-dependent phenomenon in the healthy knee and depends on the load-bearing condition. They found that the mean medial meniscus extrusion was 1.1 mm in supine and 1.9 mm in the standing position [1]. With increasing age and BMI, a significant increased medial meniscus extrusion could be observed [1]. Medial meniscus on US is significantly extruded by weight bearing in healthy knees and in knees with severe osteoarthritis [11]. However, in knees with grade 4 OA, no dynamic displacement is observed [11]. Patel et al. [19] evaluated meniscal extrusion in loaded and unloaded open MRI. These authors included patients with a mean age of 53 years and no radiological signs of osteoarthritis. They found that the medial meniscus during unloaded conditions had an extrusion of 1.0 mm with increasing medial meniscus extrusion to 1.6 mm under loading [19]. These results suggest that dynamic meniscus extrusion is most likely a physiological phenomenon [1, 11]. Achtnich et al. [1] interpreted this difference as a functional reaction of the medial meniscus on load. The elastic properties of the meniscal tissue allow a certain radial displacement under axial load. However, this physiological extrusion is prevented by the circular hoop stresses, which arise as a consequence to the attachment site of the meniscal roots on the tibia plateau [1, 22].
From this point of view, not just an absolute increased meniscus extrusion might be indicative for a dysfunction, but rather an increased or absent functional adaption reaction [1]. The present study demonstrates that loss of dynamic extrusion can be used to highlight meniscus lesions with biomechanical relevance.
In contrast to other structures in the knee joint, ultrasound is rarely used as a diagnostic tool for meniscal injuries, although ultrasound imaging, compared to MRI, has the advantage of dynamic evaluation of the knee joint [1]. One possible reason for the rare application of ultrasound in the diagnosis of meniscal pathologies is that the reliability varies considerably and is regarded as not satisfactory [16]. Nevertheless, Mureşan et al. [17] demonstrated in a prospective study with athletes that static ultrasound examination of medial meniscal lesions by an experienced examiner has a specificity of 77.7% and a sensitivity of 88.8%.
A previous study by Verdonk et al. [30] examined dynamic meniscus extrusion in patients after meniscus transplantation. They used ultrasound and MRI to compare lateral meniscal extrusion under different loading conditions. Verdonk et al. [30] state that both US and MRI are adequate measurement devices for evaluating laterally directed extrusion of the normal and transplanted lateral meniscus. In line with the previous findings, we demonstrate that healthy controls have load-dependent meniscus extrusion.
The current study has some limitations which should be addressed. First, the ultrasound examinations were only performed by one examiner. This approach was due to practicality. Patient recruitment and ultrasound examination were performed during the routine consultations. It is well established that US is a highly operator-dependent imaging method, though the previous studies show that extrusion measurement by ultrasound has a good intraclass correlation coefficient [1, 18]. Furthermore, the extrusion results of the US examination did not differ significantly from the extrusion evaluated with MRI. Second, meniscus extrusion was only measured as radial displacement on coronary plane [5, 6, 22]. The anterior-to-posterior direction was not assessed. Medial meniscal root tears are most frequently observed in the elderly [22], but the results from our study might also be applicable for different subsets of patients. In contrast, lateral root tears are more likely to appear in younger patients in combination with a cruciate ligament tear [22]. Furthermore, measurement of the mechanical axis would have been desirable, because this method allows a precise evaluation of the mechanical axis. It is well known that medial root tears are associated with varus deformity [22]. The majority of patients of the root tear group had whole-leg radiographs, but not in the control group. It would be unethical to expose healthy knees to ionizing radiation without any medical indication. Therefore, the caliper method (measuring the intercondylar and intermalleolar distances with a caliper) was used to exclude study participants with valgus deformity. Hinman et al. [10] have shown that the caliper method is a valid measure of the mechanical axis with a good correlation to the mechanical axis measured on whole-leg radiographs.
Ultrasound imaging is a favorable method due to the ubiquitous availability and user-friendly handling. While the measurement of total extrusion might be dependent on the investigator, greater extrusions can easily be detected. Therefore, US imaging of meniscus extrusion might be an alternative method to detect root tear lesions and furthermore might be a feasible option to evaluate meniscus function following root repair or meniscus transplant surgery.
Conclusion
The present study demonstrates that medial root tear of the meniscus leads to significantly increased medial meniscus extrusion with an extended extrusion also under unloaded condition. Therefore, the absent of dynamic extrusion component might be an indicator for medial root injury and could be easily detected using ultrasound. The “dead meniscus sign” can be a useful term for this finding.
References
Achtnich A, Petersen W, Willinger L, Sauter A, Rasper M, Wörtler K, Imhoff AB, Diermeier T (2018) Medial meniscus extrusion increases with age and BMI and is depending on different loading conditions. Knee Surg Sports Traumatol Arthrosc 26(8):2282–2288
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Jt Surg Am 90(9):1922–1931
Bathia S, LaPrade CM, Ellman MB, LaPrade RF (2014) Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 42(12):3016–3030
Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonté F, Beaudoin G, Bloch DA, Choquette D, Haraoui B, Altman RD, Hochberg M, Meyer JM, Cline GA, Pelletier JP (2005) Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 64(4):556–563
Choi C-J, Choi Y-J, Lee J-J, Choi C-H (2010) Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 26:1602–1606
Costa CR, Morrison WB, Carrino JA (2004) Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol 183(1):17–23
Doral MN, Bilge O, Huri G, Turhan E, Verdonk R (2018) Modern treatment of meniscal tears. EFORT Open Rev 3(5):260–268
Emmanuel K, Quinn E, Niu J, Guermazi A, Roemer F, Wirth W, Eckstein F, Felson D (2016) Quantitative measures of meniscus extrusion predict incident radiographic knee osteoarthritis-data from the Osteoarthritis Initiative. Osteoarthr Cartil 24(2):262–269
Forkel P, Reuter S, Sprenker F, Achtnich A, Herbst E, Imhoff A, Petersen W (2015) Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc 23(1):112–118
Hinman RS, May RL, Crossley KM (2006) Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Rheum 55:306–313
Kawaguchi K, Enokida M, Otsuki R, Teshima R (2012) Ultrasonographic evaluation of medial radial displacement of the medial meniscus in knee osteoarthritis. Arthritis Rheum 64(1):173–180
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16(4):494–502
Koo JH, Choi SH, Lee SA, Wang JH (2015) Comparison of medial and lateral meniscus root tears. PLoS One 10(10):e0141021
Koenig JH, Ranawat AS, Umans HR, Difelice GS (2009) Meniscal root tears: diagnosis and treatment. Arthroscopy 25(9):1025–1032
Lee DW, Ha JK, Kim JG (2014) Medial meniscus posterior root tear: a comprehensive review. Knee Surg Relat Res 26(3):125–134
Lefevre N, Naouri JF, Herman S, Gerometta A, Klouche S, Bohu Y (2016) A current review of the meniscus imaging: proposition of a useful tool for its radiologic analysis. Radiol Res Pract 2016:8329296. https://doi.org/10.1155/2016/8329296
Mureşan S, Mureşan M, Voidăzan S, Neagoe R (2017) The accuracy of musculoskeletal ultrasound examination for the exploration of meniscus injuries in athletes. J Sports Med Phys Fit 57(5):589–594
Nogueira-Barbosa MH, Gregio-Junior E, Lorenzato MM, Guermazi A, Roemer FW, Chagas-Neto FA, Crema MD (2015) Ultrasound assessment of medial meniscal extrusion: a validation study using MRI as reference standard. AJR Am J Roentgenol 204(3):584–588
Patel R, Eltgroth M, Souza R, Zhang CA, Majumdar S, Link TM, Motamedi D (2006) Loaded versus unloaded magnetic resonance imaging (MRI) of the knee: effect on meniscus extrusion in healthy volunteers and patients with osteoarthritis. Eur J Radiol Open 3:100–107
Petersen W, Tillmann B (1998) Collagenous fibril texture of the human knee joint menisci. Anat Embryol (Berl) 197(4):317–324
Petersen W, Zantop T (2006) Avulsion injury to the posterior horn of the lateral meniscus. Technique for arthroscopic refixation. Unfallchirurg 109(11):984–987
Petersen W, Forkel P, Feucht MJ, Zantop T, Imhoff AB, Brucker PU (2014) Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg 134(2):237–255
Robertson DD, Armfield DR, Towers JD, Irrgang JJ, Maloney WJ, Harner CD (2009) Meniscal root injury and spontaneous osteonecrosis of the knee: an observation. J Bone Jt Surg Br 91(2):190–195
Rowland G, Mar D, McIff T, Nelson J (2016) Evaluation of meniscal extrusion with posterior root disruption and repair using ultrasound. Knee 23(4):627–630
Saad SS, Gorbachova T, Saing M (2015) Meniscal tears: scanned, scoped, and sculpted. Radiographics 35(4):1138–1139
Stoller DW, Martin C, Crues JV 3rd, Kaplan L, Mink JH (1987) Meniscal tears: pathologic correlation with MR imaging. Radiology 163(3):731–735
Suh JS, Lee SH, Jeong EK, Kim DJ (2001) Magnetic resonance imaging of articular cartilage. Eur Radiol 11:2015–2025
Sung JH, Ha JK, Lee DW, Seo WY, Kim JG (2013) Meniscal extrusion and spontaneous osteonecrosis with root tear of medial meniscus: comparison with horizontal tear. Arthroscopy 29(4):726–732
Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T (2018) Medial meniscal extrusion: detection, evaluation and clinical implications. Eur J Radiol 102:115–124
Verdonk P, Depaepe Y, Desmyter S, De Muynck M, Almqvist KF, Verstraete K (2004) Normal and transplanted lateral knee menisci: evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc 12:411–419
Zantop T, Petersen W (2011) Avulsionsverletzungen “root tears”. Arthroskopie 24(1):48–56
Funding
No external funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All other authors declare that they have no conflict of interest related to this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Karpinski, K., Diermeier, T., Willinger, L. et al. No dynamic extrusion of the medial meniscus in ultrasound examination in patients with confirmed root tear lesion. Knee Surg Sports Traumatol Arthrosc 27, 3311–3317 (2019). https://doi.org/10.1007/s00167-018-5341-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5341-4