Abstract
Purpose
Meniscus extrusion has always been described as an indirect sign of meniscus pathology and is associated with a loss of function of the affected meniscus. The current cut-off value of 3 mm displacement is indicated as abnormal and has been determined on magnetic resonance images (MRI) and ultrasound (US). However, it has to be considered that there is no description of the physiological meniscus extrusion in healthy knees depending on age or different weight-bearing conditions. It was hypothesized that in healthy knees there is a physiological age and BMI dependent meniscal extrusion, and meniscus extrusion depends on different loading conditions.
Methods
Healthy volunteers with non-symptomatic knee, and no history of knee injuries or operations were included in this prospective cross-sectional study. Exclusion criteria were age < 18years, subjective or objective instability, malalignment and positive medial meniscus test. Secondary exclusion criteria were osteoarthritis ICRS grade 3–4 or signs of meniscus tear on MRI. Every patient underwent standard knee examination following measurement of medial meniscus extrusion (MME) using US. In US extrusion was determined in supine position (unloaded) and in standing position with full weight-bearing and 20° of flexion (loaded). MRI was performed in a neutral knee position to compare ultrasound measurements with the current gold standard. Based on the power calculation of preliminary results a minimum of 70 volunteers was needed.
Results
75 patients were enrolled to this study. The mean US MME was 1.1 mm ± 0.5 mm in supine position and 1.9 mm ± 0.9 mm under full weight-bearing. The mean US Δ-extrusion was 0.8 mm ± 0.6 mm. With rising age, a significant increased MME in US and MRI could be demonstrated (p < 0.001). Furthermore, elevated BMI was significantly correlated to increased US MME under full weight-bearing (p = 0.002) and to US Δ-extrusion (p = 0.003).
Conclusion
Based on the results of this study, medial meniscus extrusion is an age-depending phenomenon in healthy knees and depends on various load-bearing conditions. Ultrasound examination of the MME might be favorable compared to MRI due to the ability of dynamic evaluation. As a consequence, the current cut-off value of 3 mm for meniscus pathologies should be reconsidered.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The current gold standard for radiologic investigation of the meniscus is magnetic resonance images (MRI) [17]. Compared to ultrasound (US), images are static without consideration of dynamic [8, 16]. Therefore, MRI might be not suitable for illustrating load-depended changes of the meniscus. In recent years, available research on the phenomenon of meniscus extrusion has centered on pathologic findings of the meniscus on MRI.
According to the geometry and structure, the meniscus improves the congruity between the femur and the tibia and works like a load distributor [31]. In terms of pathologic changes, this alters knee biomechanics and kinematics and the transmission of circumferential hoop stresses is impaired. Choi et al. [4] detected in case of medial meniscus root tears or severe radial tears a meniscus extrusion > 3 mm of the medial meniscus in MRI. In addition Allaire et al. [1] demonstrated in their biomechanical investigation significant changes in contact pressure and knee joint kinematics due to a posterior root tear of the medial meniscus. In the literature, there is a concern that significant meniscus extrusion dramatically inhibits meniscus function, and therefore, leads to a condition comparable with a total meniscectomy. Though, meniscus extrusion is strongly related to root tears, several authors also showed an increased radial meniscal displacement for other meniscus lesions or severe osteoarthritis [5, 6].
Today’s description of meniscus extrusion is based on static MRI images [5, 14, 26]. MRI is performed in supine position, and therefore, meniscus function under load bearing could not be evaluated. One alternative imaging method is ultrasound, which is already used for assessing meniscus extrusion. Nogueira-Barbosa et al. [21] demonstrated reliable measurements of medial meniscus extrusion in supine position in ultrasound compared to MRI. According to the physiological function of the meniscus, an anterior-to-posterior translation and also a radial displacement can be observed in normal knee kinematics [27]. Therefore, evaluation of the meniscus function should be assessed dynamically. Verdonk et al. [29], as one of the first, evaluated meniscus extrusion under different loading conditions using US to assess results of lateral meniscus allografts. Extrusion was defined as the distance, measured from the border of the femoral condyle or tibia plateau to the outer edge of the meniscus. Furthermore, they also compared results of MRI and US and stated that both are adequate to measure meniscus extrusion. Kawaguchi et al. [13] investigated medial meniscus extrusion in knee osteoarthritis using US with and without weight-bearing. An increased radial displacement with weight-bearing could be observed. This finding was time dependent. Based on their results, the authors suggested a close correlation between meniscus extrusion and progression of osteoarthritis (OA).
Currently, there are only studies available investigating the association between meniscus pathologies and meniscus extrusion. However, on the basis of the meniscus function, there is no description of the physiological radial displacement of the meniscus in healthy knees. The purpose of this study was to evaluate the influence of BMI, age and load on medial meniscus extrusion of healthy volunteers using ultrasound. It was hypothesized that there is a physiological age- and BMI-dependent meniscal extrusion, and meniscus extrusion depends on different loading conditions.
Materials and methods
From November 2016 till May 2017 healthy volunteers were included in this prospective cross-sectional study. The study was registered on the German Clinical Trial Register (DRKS: 00010963). Subjects with no history of knee injuries and knee pain and age > 18 years of age were enrolled. Exclusion criteria were severe valgus or varus leg deformity, subjective or objective ligament instability or previous knee operations. Further exclusion criteria were signs of tenderness in medial joint space or positive meniscus test during clinical examination. Secondary exclusion criteria were signs of severe osteoarthritis (ICRS grade 3–4) or meniscus tear on MRI.
Subgroup analysis concerning gender, age, body mass index (BMI) and load was performed.
The study was approved by the institutional review board of the Technical University of Munich (No. 370/16 S) and conducted according to the Declaration of Helsinki. All subjects gave their written informed consent to participate in this investigation.
Clinical examination
All volunteers underwent clinical examination of the knee, based on the International Knee Documentation Committee (IKDC) form. The gold standard in assessing lower limb alignment is weight-bearing long axis radiographs [7, 23]. However, since only healthy subjects without knee-related symptoms were included in this study, such radiographs would not be in accordance with the ethical standards. Therefore, lower limb alignment was only evaluated clinically in a similar way as described by Hinman et al. [10]. Subjects were positioned in an upright position with balanced weight-bearing on both legs and fully adducted feet. Then distances between medial condyles and medial malleoli were measured by a single investigator. A distance of more then two finger—breadths in condyle—distance or malleoli—distance (corresponds to a distance of more than 3.0 cm) was interpreted as severe leg deformity. Examination of the ligament stability included testing the laxity of the medial collateral ligament (MCL) and lateral collateral ligament (LCL), as well as the anterior and posterior cruciate ligament. Meniscus was evaluated by joint space tenderness, McMurray test [19] and Thessaly test [12]. Only one knee of each subject was included.
Radiological evaluation
US examination was performed by a musculoskeletal radiologist with at least 3 years of experience in musculoskeletal imaging. All acquired images of the knees were evaluated on picture archiving and communication system PACS workstations (Agfa, Ridgefield Park, NJ, USA).
Ultrasound (US)
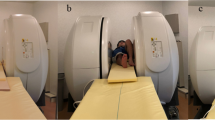
For evaluation of the medial meniscus a 13.5 MHz linear transducer (Siemens ACUSON Antares, Erlangen, Germany) was used. Subjects were positioned supine with a small roll of towel under the knee. At the 20° bended knee the medial epicondyle was palpated and the transducer was placed in the longitudinal direction parallel to the fiber orientation of the MCL. Then the medial meniscus was visible as a triangular, echogenic structure between the medial femoral condyle and the tibial plateau. Then the position of the transducer was marked on the skin. Afterwards patients were placed in an upright standing position with also 20° bended knees (loaded). Feet were placed in neutral position and body trunk and pelvis position were controlled for balanced weight-bearing on both legs. The transducer was placed in longitudinal direction at the previously marked position. The ultrasound examinations were performed by a single investigator with at least 20 years of experience in musculoskeletal radiology.
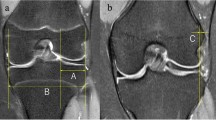
Medial meniscus extrusion in ultrasound was measured as published by Nogueira-Barbosa et al. [21]. Extrusion was defined as the distance between a tangent line parallel to the fiber orientation of the MCL at the margin of the medial tibial cortex and the outermost edge of the medial meniscus (Fig. 1). Additionally the medial displacement index (MDI) for supine and standing position was calculated as reported by Kawaguchi et al. [13]. Meniscus width was measured in MRI on coronary plane were the medial femoral epicondyle was visible. The values of meniscal extrusion in ultrasound for standing and supine position were then divided by the meniscal width and multiplied by 100 to receive the MDI. Δ-MDI was defined as the difference between MDI in standing and lying position [20].
Magnetic resonance images (MRI)
For MRI evaluation a clinical 3.0 T MR scanner (Ingenia, Philips Healthcare, Best, The Netherlands) was used. In each case, MR imaging was performed within 1 week after the initial ultrasound examination. A dedicated 16-channel knee coil was used for signal reception. Coronal proton density weighted images with spectral fat suppression were acquired with the following pulse sequence parameters: TR 4150 ms, TE 50 ms. Acquired voxel size was 0.35 × 0.46 × 2.5 mm, FOV was 160 × 160 mm. Parallel imaging (SENSE, factor 2) was enabled for faster image acquisition.
On coronal images, where the medial femoral epicondyle was visible, medial meniscus extrusion was calculated as reported by Costa et al. [5]. One vertical line was placed at the margin of the medial tibial plateau and a second one at the outermost edge of the medial meniscus. Meniscus extrusion in MRI was defined as the distance between both lines.
Statistical analysis
Statistical analysis was performed by use of SPSS software (SPSS, Chicago, IL, USA). For all statistical tests, p values less than 0.05 were considered as significant.
US images and MRI were evaluated in above described way by one orthopedic surgeon (rater 1) and one musculoskeletal radiologist (rater 2).
Descriptive statistics are presented as mean ± standard deviation (SD). Kolmogorov–Smirnov univariate normality test was used for continuous variables to confirm data normality. Correlation between US extrusion (USE) and age, respectively, BMI were assessed by Spearman’s Rho test. Correlation between USE and gender was assessed by Mann–Whitney U test.
An a priori power analysis based on the results of a pilot study was performed with G*Power 3.1.9.2 (Franz Paul, Kiel, Germany). Mean extrusion for supine and loaded condition and SD were calculated. With an effect size of 0.74, an α of 0.05 and a minimum of 70 subjects, the power of the current study is 0.8.
Results
A total of 75 healthy subjects with average age of 39.6 ± 13.5 years (range 20–70 years) were enrolled in this cross- sectional study. None of the included subjects was secondary excluded because of severe osteoarthritis or meniscal tears on coronary MRI.
Intraclass correlation (ICC) for US measurements in supine position was 0.783, CI [0.625; 0.872] (p < 0.001), and 0.900 CI [0.820; 0.942] (p < 0.001) for full weight-bearing. ICC for MRI extrusion was 0.767 CI [0.489; 0.881] (p < 0.001).
Gender
In total 58 female and 17 male were included. A significant difference between genders was evident for USE in supine position (p = 0.009), but not for USE under full weight-bearing (NS) or for US Δ-extrusion (NS). Also no significant difference between genders in MRI was visible (NS) (Table 1).
BMI
Calculated average BMI was 23.6 ± 3.9 kg/m2 (range 17.6–36.1). Average BMI for male was 23.1 ± 4.0 kg/m2 (range 17.6–32.7) and for female 25.1 ± 3.1 kg/m2 (range 21.9–36.1). A significant correlation between meniscus extrusion in loaded US and BMI (p = 0.002) was determined. Otherwise, no significant correlation for BMI and extrusion in unloaded US (NS) or MRI (NS) was evident (Fig. 2a–c).
Load
Measurements for loaded and unloaded US are summarized in Table 2. Significant difference between USE in supine position and under full weight-bearing was demonstrated (p < 0.001, Wilcoxon-Test). Likewise, significant difference between USE in supine position and extrusion in MRI was determined. Measurements for MDI are summarized in Table 3.
Age
For subgroup analysis based on age-included patients were divided into three different age groups: group (1) age 18–30 years (n = 25); group (2) age 30–50 years (n = 25); group (3) age > 50 years (n = 25). Mean age in group I was 24.4 ± 2.4 years (range 20–29), in group II 38.9 ± 6.2 years (range 30–49) and 55.5 ± 4.7 years (range 50–70) in group III. Extrusion in US and MRI are summarized in Table 4. Significant correlation between age and loaded and unloaded US measurements were demonstrated (p < 0.001). Likewise, extrusion in MRI was also significant correlated to age (p < 0.001) (Fig. 3a–c).
Discussion
The most important finding of the present study is that healthy medial meniscus showed an age-dependent ultrasonographic quantifiable extrusion depending on age and weight-bearing status. Also significant differences between genders were evident. Therefore, the concept of meniscus extrusion as a merely sign for meniscal lesions or severe osteoarthritis must be reconsidered.
Initially, meniscus extrusion received attention as an indirect sign on MRI for progression of osteoarthritis. Berthiaume et al. [2] analysed 32 patients with symptomatic knee osteoarthritis for cartilage loss in MRI in correlation to meniscal extrusion and tears. At final follow-up of 2 years, a strong correlation between medial meniscus extrusion and cartilage loss in the medial compartment was evident. Hunter et al. [11] confirmed in a similar study a strong correlation between meniscal damage and cartilage loss. In contrast to our US evaluation method, analyses on MRI are usually static. Based on the results of the present study an absolute elevated MME with increasing age was demonstrated. Nevertheless, also in older people a difference between extrusion under full weight-bearing and supine position in US was still evident. This difference could be interpreted as a functional reaction of the medial meniscus on load. One explanation for this functional adaption reaction could be found in the microstructure of the meniscus. Collagen fibers in the meniscus are oriented in a circumferential way with woven radial fibers in between [3]. The radial fibers act like tie fibers to resist longitudinal splitting. If axial load is applied, the fibers of the meniscus elongate and hoop stress is increasing. To prevent further radial displacement axial load is converted into tensile strain within the meniscus [11]. Therefore, not just an absolute increased meniscus extrusion might be indicative for a malfunction, but rather an increased or absent functional adaption reaction. Supporting the idea of a mechanical adaption reaction, Patel et al. [24] evaluated meniscal extrusion in loaded and unloaded MRI. Similar to the present study, the authors included patients with a mean age of 53 years and no radiological signs of osteoarthritis. They could show under unloaded condition a MME of 1.0 mm ± 0.7 mm, with increasing MME to 1.6 mm ± 0.9 mm under loading (p < 0.001).
Another issue, where meniscus extrusion gained more interest, is the increasing number of meniscus allograft transplantations [15, 30]. Due to the limited significance of clinical examinations, second-look arthroscopy is performed in almost 50% of the studies after meniscus transplantation [22]. During follow-up after transplantation MRI has only a minor role. As demonstrated by van Arkel et al. [28] meniscus allografts could have a variable signal intensity in MRI. An increased signal intensity was seen for scar tissue, revascularization and also in meniscal tears. Therefore, MRI as static imaging modality is not the optimal method for evaluation of meniscus allografts. To assess meniscus transplants in a more dynamic way, Verdonk et al. [29] compared meniscal extrusion in MRI and ultrasound under different loading conditions. To compare the results of the transplanted meniscus also 10 normal lateral menisci were measured. Although the lateral meniscus was evaluated in this study, variable meniscus extrusion according to different loading conditions was also visible. Regarding this results, Verdonk et al. [29] demonstrated, as one of the first, reliable results for dynamic measurement of meniscus extrusion in US.
The current focus of interest for meniscal extrusion in MRI is meniscal root tear. Costa et al. [5] evaluated retrospectively 105 MRIs and demonstrated a significant correlation between an elevated MME and different meniscal tears. 42% of the subjects with a major medial extrusion (> 3 mm) had a meniscal root tear. Choi et al. [4] confirmed a strong correlation between medial meniscus extrusion in MRI and meniscal root lesions. The mean meniscus extrusion for root tears was 3.8 mm ± 1.4 mm. Even 39.4% of subjects with pathologic extrusion (> 3 mm) had a meniscus root lesion, also 13.2% with a minor extrusion (< 3 mm) showed signs of a root tear. On the other hand according to Magee et al. [18] there are also patients with medial meniscus extrusion in MRI, but without signs of root tear in MRI or arthroscopy. This phenomenon is explained by a stretch of the meniscal root rather than a tear. Therefore, also in case of root tears the question arises whether absolute elevated MME is the critical point or is not rather an absent or elevated medial meniscus extrusion under axial load, the decisive point. A tear of the medial meniscus root results in a disruption of the circumferential collagen fibers [9]. Thereby under axial load, the ability to resist hoop stresses is reduced. Normal MRI is performed in supine position without axial load. On the basis of the data of present study also in case of meniscal root tear not an absolute elevated meniscal extrusion is essential, but an increased or absent extrusion of the medial meniscus under axial load.
The current study does have some limitations. First, ICC for US was inferior compared with MRI measurements. US is an highly operator-dependent imaging method, this could explain the moderate to good ICC [25]. Second, the limb alignment was only estimated approximately by clinical examination due to ethical reasons. Furthermore, meniscus extrusion was only measured as radial displacement on coronary plane and not in the anterior-to posterior direction.
Conclusion
In conclusion, present study demonstrates that age, BMI and load-bearing affect medial meniscus extrusion; increasing age, BMI and load were significantly correlated to increased meniscus extrusion. Moreover, data of the current study suggest that ultrasound is a feasible tool in assessing meniscus extrusion dynamically, which allows for a better understanding of the actual meniscus function as compared to static diagnostic methods. Meniscus extrusion by itself, as an indicator for meniscus pathologies, should be reconsidered. The present normative data may further be useful when evaluating patients following meniscus surgery or transplantation with potential abnormal extrusion levels.
References
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Jt Surg Am 90:1922–1931
Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonte F, Beaudoin G, Bloch DA et al (2005) Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 64:556–563
Bullough PG, Munuera L, Murphy J, Weinstein AM (1970) The strength of the menisci of the knee as it relates to their fine structure. J Bone Jt Surg Br 52:564–570
Choi C-J, Choi Y-J, Lee J-J, Choi C-H (2010) Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 26:1602–1606
Costa CR, Morrison WB, Carrino JA (2004) Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol 183:17–23
Crema MD, Roemer FW, Felson DT, Englund M, Wang K, Jarraya M et al (2012) Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the Multicenter Osteoarthritis study. Radiology 264:494–503
Eberbach H, Mehl J, Feucht MJ, Bode G, Sudkamp NP, Niemeyer P (2017) Geometry of the valgus knee: contradicting the dogma of a femoral-based deformity. Am J Sports Med 45:909–914
Friedman L, Finlay K, Jurriaans E (2001) Ultrasound of the knee. Skeletal Radiol 30:361–377
Hajek PC, Gylys-Morin VM, Baker LL, Sartoris DJ, Haghighi P, Resnick D (1987) The high signal intensity meniscus of the knee. Magnetic resonance evaluation and in vivo correlation. Invest Radiol 22:883–890
Hinman RS, May RL, Crossley KM (2006) Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Rheum 55:306–313
Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M et al (2006) The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum 54:795–801
Karachalios T, Hantes M, Zibis AH, Zachos V, Karantanas AH, Malizos KN (2005) Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. J Bone Jt Surg Am 87:955–962
Kawaguchi K, Enokida M, Otsuki R, Teshima R (2012) Ultrasonographic evaluation of medial radial displacement of the medial meniscus in knee osteoarthritis. Arthritis Rheum 64:173–180
Kenny C (1997) Radial displacement of the medial meniscus and Fairbank’s signs. Clin Orthop Relat Res 339:163–173
Kim J-M, Lee B-S, Kim K-H, Kim K-A, Bin S-I (2012) Results of meniscus allograft transplantation using bone fixation: 110 cases with objective evaluation. Am J Sports Med 40:1027–1034
Lee D, Bouffard JA (2001) Ultrasound of the knee. Eur J Ultrasound 14:57–71
Lefevre N, Naouri JF, Herman S, Gerometta A, Klouche S, Bohu Y (2016) A current review of the meniscus imaging: proposition of a useful tool for its radiologic analysis. Radiol Res Pract 2016:8329296
Magee T (2008) MR findings of meniscal extrusion correlated with arthroscopy. J Magn Reson Imaging 28:466–470
McMurray T (1942) The semilunar cartilages. Br J Surg 29:407–414
Murakami T, Enokida M, Kawaguchi K, Otsuki R, Nagashima H (2017) Useful ultrasonographic evaluation of the medial meniscus as a feature predicting the onset of radiographic knee osteoarthritis. J Orthop Sci 22:318–324
Nogueira-Barbosa MH, Gregio-Junior E, Lorenzato MM, Guermazi A, Roemer FW, Chagas-Neto FA et al (2015) Ultrasound assessment of medial meniscal extrusion: a validation study using MRI as reference standard. AJR Am J Roentgenol 204:584–588
Oh KJ, Sobti AS, Yoon JR, Ko YB (2015) Current status of second-look arthroscopy after meniscal allograft transplantation: review of the literature. Arch Orthop Trauma Surg 135:1411–1418
Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A (1994) Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin N Am 25:425–466
Patel R, Eltgroth M, Souza RB, Zhang CA, Majumdar S, Link TM et al (2016) Loaded versus unloaded magnetic resonance imaging (MRI) of the knee: effect on meniscus extrusion in healthy volunteers and patients with osteoarthritis. Eur J Radiol Open 3:100–107
Scheel AK, Schmidt WA, Hermann KA, Bruyn GA, D’Agostino M-A, Grassi W et al (2005) Interobserver reliability of rheumatologists performing musculoskeletal ultrasonography: results from a EULAR “Train the trainers” course. Ann Rheum Dis 64:1043–1049
Sugita T, Kawamata T, Ohnuma M, Yoshizumi Y, Sato K (2001) Radial displacement of the medial meniscus in varus osteoarthritis of the knee. Clin Orthop Relat Res 387:171–177
Thompson WO, Thaete FL, Fu FH, Dye SF (1991) Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med 19:210–216
van Arkel ER, Goei R, de Ploeg I, de Boer HH (2000) Meniscal allografts: evaluation with magnetic resonance imaging and correlation with arthroscopy. Arthroscopy 16:517–521
Verdonk P, Depaepe Y, Desmyter S, De Muynck M, Almqvist KF, Verstraete K et al (2004) Normal and transplanted lateral knee menisci: evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc 12:411–419
Verdonk PC, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R (2005) Transplantation of viable meniscal allograft: survivorship analysis and clinical outcome of one hundred cases. J Bone Jt Surg Am 87:715–724
Walker PS, Erkiuan MJ (1975) The role of the menisci in force transmission across the knee. Clin Orthop Relat Res 109:184–192
Funding
This study was funded by Deutsche Arthrose Hilfe e.V.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All other authors declare that they have no conflict of interest related to this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Achtnich, A., Petersen, W., Willinger, L. et al. Medial meniscus extrusion increases with age and BMI and is depending on different loading conditions. Knee Surg Sports Traumatol Arthrosc 26, 2282–2288 (2018). https://doi.org/10.1007/s00167-018-4885-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4885-7