Abstract
Joint surface incongruence resulting from osteochondritis dissecans (OCD) alters the articular physiologic congruence, increasing the contact stress on adjacent joint surfaces and accelerating wear and the cascade of joint degeneration. Accordingly, the restoration of articular surface integrity is of major importance, especially in young adults where, in lesions left untreated or following simple fragment excision, early osteoarthritis can be anticipated. Therefore, the treatment algorithm in unstable knee OCD of the young adult foresees surgical options to restore the articular surface. Several procedures have been proposed, including refixation of the detached fragment bone marrow stimulation, osteochondral autograft implantation, fresh osteochondral allograft transplantation, and cell-based or cell-free regenerative techniques. The aim of this review was to summarize the evidence for these surgical strategies, reporting their results and limitations. The overall evidence documents positive results for each of the assorted surgical procedures applied to treat unstable OCD, thus indicating support for their selected use to treat osteochondral defects paying particular attention to their specific indications for the lesion characteristics. The fixation of a good quality fragment should be pursued as a first option, while unfixable small lesions may benefit from autografts. For large lesions, available cell-based or cell-free osteochondral scaffold are a feasible solution but with limitation in terms of regenerated tissue quality. In this light, fresh allografts may offer articular surface restoration with viable physiologic osteochondral tissue providing a predictably successful outcome, and therefore they may currently represent the most suitable option to treat unstable irreparable OCD lesion in young adults.
Level of evidence
V.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteochondritis dissecans (OCD) is a pathology involving the osteochondral unit, resulting in sequestration of subchondral bone with or without articular cartilage involvement and instability [55]. OCD has been known for centuries [98], even before König coined the term in 1888 [61], which is currently in use despite the lack of clear correspondence of the “osteochondritis” inflammatory influences with current etiopathology hypothesis [5, 49, 98].
OCD has a prevalence of 15–29/100.000 among the general population and an incidence increasing over time [67]. It mostly affects young patients, with a male-to-female ratio of 5:3, mainly between 10 and 20 years old [55]. The age at the time of clinical symptoms onset is recognized to be crucial in determining both prognosis and guiding treatment. In this light, OCD lesions are properly classified, according to the status of the growth plate at the time of diagnosis, as juvenile or adult OCD. Juvenile OCD lesions are characterized by a considerably better overall prognosis than adult OCD [51, 66], and can usually be treated conservatively [4, 91]. Conversely, adult OCD, which mostly affects young adults after metaphyseal closure, rarely heals without operative intervention [31]. In this patient population, the key factor guiding the orthopedic surgeon toward treatment selection is the stability of the OCD fragment, other than the size and location of the lesion. The term “stability” has been referred to as the mechanical integrity of the subchondral lesion: a stable fragment is defined as one that is in situ and immobile; conversely, an unstable fragment is defined as a lesion that may be in situ but mobile, in situ but fragmented, or ex situ [76].
Several classification systems have been published to distinguish between stable and unstable OCD lesions. This may be suggested by OCD features on radiographs [52], MRI [12, 38], and ultimately, arthroscopic evaluation [16, 24]. The most common, the ICRS classification, describes four different grades: I—stable lesions with a continuous area with “softening” covered by intact cartilage; II—lesions with partial discontinuity but still stable when probed; III—lesions with a complete discontinuity that are not yet dislocated (“dead in situ”); IV—dislocated fragment, loose within the bed or empty defect [16]. Since a loose fragment or the excision of an unstable fragment result in articular surface incongruity, the risk of premature osteoarthritis becomes certain [92]. Thus, the treatment algorithm foresees procedures aimed specifically at restoring the articular surface when grade 3–4 lesions are identified. Several options have been proposed to treat such OCD lesions in young adults; including refixation of the detached fragment (reduction and fixation) bone marrow stimulation (enhancing in situ healing), osteochondral autograft implantation, fresh osteochondral allograft transplantation, and cell-based or cell-free regenerative techniques.
The purpose of this review is to summarize the evidence for these surgical strategies, reporting results and limitations, aiming at providing an updated insight on the best option for the treatment of unstable OCD lesions in young adults.
Refixation of the osteochondral fragment
The refixation of the osteochondral fragment is the first option to be considered by an orthopedic surgeon to restore the integrity of the articular surface with the native hyaline chondral layer. The key point of this procedure is to stabilize the fragment, fixing it into original position to obtain an optimal reconstruction of the intact osteochondral unit, for best clinical result [32, 88].
Indication for fragment fixation, or reduction and fixation has evolved over time. Robert et al. [88], in 1998, after a study on 43 patients, concluded that “… fixation can be attempted if the fragment volume is bigger than 1 cm, is in the weight-bearing zone and is partially or totally detached”. Later, Brittberg [14] further restrained the indication, limiting it to when a good bone quality can be appreciated and the overlying cartilage is fairly intact. The bone part of the OCD fragment should be examined carefully. If it is of good quality and fits the underlying bone cavity exactly, it should be re-fixed directly after refreshment of the bony bottom with debridement and drilling. If the bone element is of good quality but no longer fits exactly into the cavity (under sized), autogenous bone grafting can be applied. This is done, following debridement of intervening fibrotic tissue and preparation of the donor site and recipient bone bed, before fragment fixation, with the goal to restore the native articular congruence. If the bone of the OCD fragment is atrophic and/or sclerotic, or the associated cartilage elements are destroyed, there will be little chance of functional survival and different surgical options should be considered.
In terms of surgical technique, the fixation method depends on the individual surgeon’s preferences based on the fragment size. The first published technique foresaw open surgical fragment fixation with thin Kirschner wires [40], but the main problem was the lack of fragment stability, other than the necessity to perform a second surgery to remove the K-wires. Afterwards, the use of metallic cannulated compression screws was widely adopted to fix the osteochondral fragment, reporting good clinical results [32, 88]. Compared with K-wires, the main advantage of cannulated compression screws was the better fragment compression and fixation, but it still required a second surgery to remove the screws [99], with the breakage of the metallic cannulated screws being the most frequent complication [75]. Besides these screws, different metallic devices have been used to fix the osteochondral fragment, such as staples [54] and Herbert screws [62]. To avoid the second surgery to remove the metallic devices, the fixation strategy evolved to bio-absorbable devices, such as poly-l-lactic acid materials, in a pin [36, 81, 107] or nail shape [105]. The published studies have shown good to excellent clinical results, clinically and at arthroscopic second look evaluation, but complications were also reported with inflammatory knee synovitis [81] and implants failures [23].
Results of fixation techniques are generally good, with case series mainly focused on juvenile cases and limited for results specific to AOCD. At short/medium-term follow-up, Trabaddor et al. [97] reported good results on a mixed population of juvenile and adult unstable OCD lesions, with complete healing in 54% and partial healing in 38% radiographs at 19 months after fixation with a poly 96L/4D-lactide copolymer nail. Nakagawa et al. [81] also reported, in a mixed population of eight patients treated with similar “bio-absorbable” pins or alternatively bone pegs, fragment union at radiographic evaluation in seven out of eight cases, with good/excellent Hughston scores and 100% patient satisfaction at 5-years. At the same follow-up, the study of Weckstrom et al. [105] confirmed overall good results in a selected young adult population of 30 knees with closed physes. Interestingly, comparing between “bio-absorbable” pins and nails, they identified better results for the nails. A nail was defined as designed with barb or head, so to give compression capacity and was suggested as explaining why less cases of incomplete bone formation and 73% vs 35% of good or excellent functional results were associated with nailing.
Compression-type titanium Herbert screws were evaluated by Makino et al. [71], showing in a mixed juvenile/adult OCD population with 15 knees; 12 normal, two nearly normal, and one abnormal ICRS scores by second-look arthroscopy at mean 14 weeks. At 50 months, this cohort had a 93% healing rate by MRI, as well as improvements in Lysholm and IKDC scores. At longer follow-up of 9 years, Magnussen et al. [70] reported significant improvements following metallic screw fixation in Marx activity score, and four out of five KOOS subscales with values comparable to age-matched controls. More recently, Barret et al. [7] analyzed 22 skeletally mature patients treated with metal headless compression-type screws, documenting radiographic healing in 82% (four patients required re-operations), with an overall satisfactory activity level and knee function at 8.7 years of follow-up. Finally, Fokter et al. [45] studied retrospectively eight patients at a long follow-up of mean 14.8 years after treatment with metal compression screws. Since all lesions were healed and stable to arthroscopic probing at 3 months, and the mean IKDC subjective score was 89.9 at final follow-up, they concluded supporting fragment fixation by compression technique to best preserve the articular surface.
Bone marrow stimulation techniques and autografts
Various bone marrow stimulation techniques such as microfractures and drilling are used in the clinical practice to treat cartilage or superficial osteochondral defects. The rationale of microfracture is to allow access of potential cartilage precursors from the underlying bone marrow to the articular surface, thus stimulating a healing response in an attempt to fill in the articular defect with an amalgam of bone and fibrocartilage [95]. By contrast, in the process of subchondral or transchondral drilling, the intended effect is to stimulate the region between the native bone and the pathologic OCD lesion to anneal [31].
Drilling is an accepted procedure to treat stable OCD lesions in immature patients after fail of conservative management [13]. The literature describes two types of procedures, antegrade and retrograde drilling, but this terminology has resulted in confusion and misinterpretation regarding the direction of drilling [37]. The use of the terms “transarticular drilling” and “retroarticular drilling” would be clearer and should be preferred. While no comparative studies are available to prove the superiority of one approach over the other, both techniques are well described and have excellent outcomes [2, 3] for the proper indications. However, they are not recommended in the treatment algorithm for unstable adult OCDs, as this level of disease is not capable of in situ healing without fixation [68].
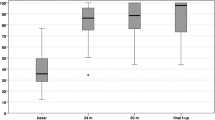
Microfracture represents the most common bone marrow stimulation technique. This approach can be applied for stimulating the remnant bone area from the lesion after osteochondral fragment removal, although capacity for repair is more suited for other articular lesions, without substantive bone loss. Several studies showed that the clot formation after microfracture produces fibrocartilage characterized by a high concentration of type I collagen rather than type II collagen, and the ability of this technique to reproducibly create enough tissue to fill large lesions may be limited. As well, the fibrocartilage typically produced lacks mechanical integrity compared to hyaline cartilage and often deteriorates after a few years. While this is a general limitation for superficial cartilage lesions, an exponential increase of this limit occurs when treating larger osteochondral defect as OCD lesions, where the subchondral bone needs to be restored as well. This is reflected by a lack of evidence about the use of microfractures for OCD, with only sporadic reports [63]. Gudas et al. [50] performed a prospective randomized study comparing the outcome of microfractures with osteochondral autograft transplantation (OAT) for the treatment of OCD [50]. At a mean follow-up of 4.2 years, 83% of the OAT group and 63% of the microfracture group had good or excellent outcomes. Patients in the microfracture group showed substantial deterioration between examinations at 1 and 4 years, and 41% of failures were reported in the microfracture group compared with none in the OAT group at final follow-up.
Osteochondral Autograft Transplant (OAT) is a surgical technique that allows a more physiological restoration of the osteochondral unit. This reconstructive surgical approach involves the harvesting and subsequent implantation of autologous osteochondral plugs in a single-stage surgical procedure. The plugs are harvested through a small incision from a lesser weight-bearing region (often from the same joint), and provides for transfer of viable osteochondral tissue units aiming, to capitalize on bone-to-bone healing. Multiple small diameter osteochondral plugs can be used to reduce donor site morbidity, and invasiveness may be further reduced by the possibility to implant the grafts through an arthroscopic approach [72]. The influence of subchondral bone pathomechanics on the overlying articular cartilage plays a central role in the progression of OCD, and the OAT technique presents the advantage to adapt the depth of the donor plug to have a stable implant and fill the entire defect with viable bone and articular cartilage [72].
Miniaci and Tytherleigh-Strong [78] suggested using OAT technique for fixing unstable knee OCD lesions. Osteochondral 4.5 mm grafts were harvested from the edges of the trochlea and inserted through the osteochondral lesion in a mixed population of 20 patients affected by juvenile and adult OCD. 6 months after surgery, all knees were fully healed at MRI, and 18 months after surgery all knees were “normal” both clinically and radiologically. Beside fragment fixation, OAT has been applied to restore the entire area of a lesion, with data showing good survival rate of the autologous hyaline cartilage transplanted. Yoshizumi et al. [108] treated successfully three skeletally mature 18-year-old patients, showing both clinical and radiological healing of the OCD lesions. Smolders et al. [94] described satisfactory results in a group of seven adult patients with eight lesions ranging from 0.5 cm2 to 3.2 cm2. At 12-month follow-up, the subjective IKDC score significantly improved, as well as KOOS for pain, symptoms, ADL and QoL. However, larger lesions could not be fully covered even with the multiple cylinders transplanted, and MRI evaluation showed a non-complete osseous integration. Wang et al. [104] reported poor results when OAT was used to treat lesions larger than 6 cm2. As complete coverage of the defect, especially in case of large lesions, is critical, the OAT technique has limitations for addressing the entire defect, even when multiple grafts plugs are used. This as donor tissue is limited and fibrocartilage forms around the periphery of each individual grafts creating a mixed healing response. Inherent to this technically demanding procedure is limited graft availability with the risks of morbidity at the donor site. This severely reduces the possibility of using these procedures for the treatment of large defects or patients with limited healthy adjacent tissue.
Allografts
The use of fresh osteochondral allograft (FOCA) tissue for the treatment of OCD is an established surgical therapy for symptomatic lesions which have not healed prior to impending skeletal maturity and have left a substantive articular defect, are not amenable to direct repair or have failed prior surgery [31, 35, 46]. The rational for transplantation of allogenic tissue stems from the unique nature of this approach, providing immediate congruent restoration of the articular surface with structurally competent subchondral bone and associated viable chondral surface, with no size limitations. The fundamental indication for transplantation of allogenic osteochondral grafts includes substantive (> 2 cm2) joint surface compromise with bone loss and/or failed prior cartilage repair. Technically, pathologic OCD tissue can be removed by cylindrical drills and replaced by press fit dowels, or resected to create a flush surface for application of “shell grafts” [21, 33]. The later requires fixation to maintain compression, although an amalgam of these two methods, the “bio-uni” instrumentation set, provides a press fit mechanism to replace avoid lesions of the femoral condyle [87]. Selection of a specific surgical technique aims to craft a transplant–host articular contour that restores native anatomy after removal of the OCD pathology.
Results for FOCA are among the most favorable seen for surgical treatment of advanced OCD, although direct comparison is confounded by patient age, lesion size, lesion location and associated diagnosis (mal-alignment, knee instability, meniscal pathology) [65]. The most experience with this technique for treating OCD involves distal femur injury. Cotter et al. [29] analyzed the results of FOCA in 37 skeletally mature patients in whom prior surgical intervention failed, and they reported clinically meaningful improvements in patient-reported outcomes and high patient satisfaction and return to sport rates at an average of 7 years’ follow-up, with a low failure rate (5.1%). Lyon et al. [69] reported short-term success with FOCA in a mixed population of 11 juvenile and adult OCDs, where all patients presented at 2 years with full radiographic graft incorporation and return to full sport activities. The largest series were documented by Sadr et al. and Emmerson et al. (135 and 64 patients) [39, 90]. Although these reports included patients as young as 12 and 15 years old, mean age in the cohorts was 21 and 28 years, respectively. A 93% survivorship was documented, with 95% patient satisfaction at 10 years, results confirmed by Murphy et al. [80], who showed 90% survival of the grafts at 10 years and an identical percentage of satisfied or extremely satisfied patients, reflecting IKDC and Knee Society Function score improvements of 33 and 20 points, respectively. A representative series of pre and post-operative images of a large osteochondral lesion treated with FOCA are presented in Fig. 1.
Images of a young male adult with osteochondritis dissecans. Pre (a, b) and Post (c, d) operatively. a Flexed knee AP radiograph showing the classic lateral aspect of the medial femoral condyle lesion and associated displaced large loose fragment, b Sagittal STIR MRI of the medial femoral condyle shows a large displaced OCD lesion with minimal fragmentation. Post-op CT scans 3 months after surgery, indicating bone incorporation of the FOCA (“Bio-uni technique”) into the prior site of bone deficit in the area of the prior OCD lesion, c Coronal and d sagittal plane
The successful use of FOCA transplant is also reported in a series of OCD cases in the elbow in young baseball players, where all nine treated patients were capable of return to throwing [79]. Good results were reported in similar case series and reports describing FOCA for osteochondral conditions analogous to OCD [11, 47], with successful treatments in the patellae and the proximal humerus. Furthermore, FOCA has also been used to address large osteochondral lesions of the talus with up to 87% good and stable results over time [102].
The principal limitation for this technology surrounds the availability of tissue. This stems from access to healthy donors and temporal limitations across the procurement and distribution process necessary to maintain chondrocyte viability and meet government regulations pertaining to aseptic collection and distribution of human tissue. Clinical factors potentially limiting applicability include size matching and graft congruence with native joint surface, incorporation to adjacent tissue, preservation of in vitro viability and potentially graft–host immunologic considerations [18, 28, 56, 93, 106]. Although there is no specific concern for systemic immunologic “rejection” phenomenon per se, and blood type matching is not required for this process, limiting the potential for antigenic exposure is strongly recommended as an essential element of both graft processing and implant procedures [22, 77, 93]. Practically, time from identification of adequate disease free tissue to transplant and common post-operative rehabilitation restrictions place burden on surgical scheduling and patient acceptance [53]. Finally, regulatory restrictions, organization and distribution issues concur to limit the possible application and benefits of this successful procedure to a few countries [30].
Cell-based treatments
Autologous chondrocytes implantation (ACI) is a regenerative cell-based procedure aiming at recreating a hyaline-like tissue to restore the chondral elements of the articular surface as similar as possible to the physiological one. It involves two surgical procedures: the first one to harvest articular cartilage from a non–weight-bearing area and the second, after cell expansion, for the implantation of cultured chondrocytes [72]. ACI has been employed with high rate of success in treating full thickness defects of articular cartilage of the knee since its very first description [15]. In case of deep osteochondral lesions, such as those observable in OCD, this original purely chondral approach was limited by challenge of restoring articular congruity, potential instability of the ACI graft and delayed maturation of the cells of the implant into “tissue”, especially in defects deeper than 8–10 mm [86]. The poor histologic quality of regenerated tissue was highlighted by LaPrade et al. [64] who found mainly fibro-cartilaginous tissue and type I collagen in a series of OCDs treated with ACI. The first-generation technique was thus subsequently modified to directly address the pathologic subchondral bone, with the introduction of the so-called “sandwich” technique: cancellous bone was used to fill the bony defect and chondrocytes were then injected between two periosteal flaps over the grafted bone [86]. Afterwards, the procedure has been further modified using a porcine collagen membrane as an alternative to periosteum to cover the lesion and the chondrocyte suspension [103]. Peterson et al. [85] treated 58 patients and reported 93% improvement at 5.6 years’ follow-up, and similar results were confirmed by Cole et al. [27], who obtained an 85% success rate at 4 years. More recently, Bhattacharjee et al. reported histology of 17 OCDs treated with bone graft + ACI showing good integration of repaired cartilage with the bone graft. However, subchondral bone was found atypical in 90% of the MRI analyses, with the most common abnormalities being subchondral bone cysts and disorganized non-homogeneous bone graft [10].
First-generation ACI has been associated with several limitations related to the complexity and morbidity of the surgical procedure that requires a large joint exposure with a high risk of arthrofibrosis [82]. Moreover, there is a frequent occurrence of periosteal hypertrophy and delamination, which often requires revision surgery. Technical problems were also identified, such as maintenance of chondrocyte phenotype, non-homogeneous cell distribution and cell loss using liquid suspension. To address these problems, matrix-assisted autologous chondrocyte transplantation (MACT) techniques have been developed. Scaffolds provide a support for cell adhesion, proliferation while maintaining the chondrocyte phenotype, and production of matrix. The ease of scaffolds handling even permitted the development of arthroscopic implantation techniques. Several scaffold designs have been developed recently and combined with autologous bone grafting to treat deep ostechondral lesions with good medium-term results [42]. Bartlett et al. [8] reported preliminary results at 1-year follow-up: four of the five patients had good or excellent results. Steinhagen et al. [96] showed good or excellent results in 18 out of 21 patients at 3 years of follow-up, and Filardo et al. confirmed the potential of this procedure reporting a significant improvement of function and symptoms maintained at 6 years in 34 knees [42]. More recently, Zellner et al. [109] reported about a large series of 51 patients affected by of osteochondral lesions, with both good clinical and imaging findings at 3 years. Despite the generally good clinical results shown with MACT combined with bone graft, also this scaffold-based technique has limitations. Graft hypertrophy, well described as one of the most common complications after first-generation ACI, was documented also by Niethammer et al. [83], who observed a significant incidence of graft hypertrophy using MACT for OCD lesions as well. Moreover, it remains a two-step technique with regulatory restrictions for cell manipulation in many countries and considerably high costs if compared to other surgical alternatives.
One-step cell-based techniques are therefore of increasing interest, taking advantage of the use of bone marrow concentrates obtained from the iliac crest. The rationale for this approach is based on the theoretical capability of the multipotent cells and microenvironment influences to differentiate and regenerate both the cartilaginous and subchondral bone layer [101]. Bone marrow concentrates have been delivered with assorted scaffolds and blood derivatives, and either implanted with overlapping layers or with bone grafting, so to fill the osteochondral defects. A few reports, using a minimally invasive arthroscopic approach suggest early promising results [89, 101].
Overall, these cell-based approaches show good clinical results for cartilage lesions. However, adaptation of techniques, originally developed for cartilage lesions, to address the more advanced lesions with underlying subchondral pathology, also presented some limitations. Evidence of a less successful outcome for larger lesions has been reported, with abnormal MRI findings increasing over time, indicating that the optimization of these cell-based approaches, for regenerating both bone and cartilage joint surface to treat OCD lesions, has remaining challenges [44, 101].
Cell-free scaffolds
Cell-free scaffolds have been introduced recently to treat OCD lesions with the advantages of avoiding the risks related to cell manipulation (such as bacterial contamination and disease transmission, and phenotypic regression), reducing costs and simplifying the surgical procedure. To this aim, biomaterials have been developed not just as carrier systems for cell delivery but also for enhancing intrinsic ability to provide chondral or osteochondral healing or regeneration. Results at short- and medium-term follow-up have established the potential of this approach [60]. Although the possibility shown by isolated reports suggests that acellular matrices can repair isolated chondral injury, the development of osteochondral-specific scaffolds, capable to guide regeneration of both bone and cartilage remains a significant scientific and clinical hurdle.
Biphasic scaffolds have been developed with the aim to restore the osteochondral unit, but only few have been investigated in clinical trials. Only one has been specifically evaluated for the treatment of OCD: a nanostructured biomimetic scaffold with a composite structure mimicking the architecture of the native subchondral bone–cartilage unit [59]. The construct is composed of a superficial layer consisting of type I equine-derived collagen designed to provide a surface mimicking native hyaline cartilage; the deep layer is made of type I collagen (30%) and hydroxyapatite (70%), meant to substitute subchondral bone; and between there is an intermediate transition layer of 60% type 1 collagen and 40% of hydroxyapatite [59]. The scaffold structure is designed to allow migration and colonization by subchondral bone stem cells to obtain osteochondral tissue regeneration [59]. This scaffold is implanted through either a lateral or medial parapatellar mini-arthrotomy. Once the lesion parameters are identified, the sclerotic subchondral bone is eliminated, creating an area of optimally 6–8 mm in depth, with stable shoulders to house the scaffold. After shaping the scaffold to the proper dimensions, it can be implanted by press fit technique or with addition of fibrin glue for further stabilization [41]. This implant has been applied for the treatment of late stage (ICRS 3–4) large irreparable cartilage lesions in adults or sequelae of juvenile OCD disease, as well as other complex osteochondral defects such as multifocal [57] or patello-femoral lesions [58], in revision surgery of previously failed reparative surgery (i.e., fixation of a non-viable unstable fragment) or even late stage osteonecrosis [9].
A representative series of pre-, intra- and post-operative images of a large osteochondral lesion treated with the osteochondral scaffold are presented in Fig. 2.
Images of a young male adult with osteochondritis dissecans. Pre (a), Intra (b, c) and Post (d) operatively. a Coronal plane MRI of the medial femoral condyle documenting a large OCD lesion, b Intra-articular view of defect site preparation with vertical shoulders to host the scaffold. c The defect is filled with the osteochondral scaffold, properly sized and implanted press fit, with further fixation by applying fibrin glue. d Coronal plane MRI documenting the imaging results of the implant at 2 years of follow-up
Kon et al. [58] reported good clinical results after 5 years in a population of patients treated with this scaffold for osteochondral lesions of different aetiologies, including OCD. These results were similar to those of Berruto et al. who reported a multicenter study involving 49 patients treated for symptomatic osteochondral lesions. Subgroup analysis found the best improvement when treating OCD etiology [9]. Afterwards, Filardo et al. [43] specifically focused on a cohort of 27 consecutive adult patients with symptomatic late stage OCD of the femoral condyles. He reported a significant improvement of clinical scores at 1 year with further improved at 2 years. These results for treatment of OCD lesions were also confirmed by Delcogliano et al. [34], with good functional outcomes in 23 patients at 2 years’ follow-up. Given these findings, the use of biphasic scaffolds in treating OCD can be considered another option, which provides advantages in comparison to other methods. It requires only one surgery avoiding the need for a cell harvesting procedure, necessary when using ACI or MACT type techniques. Moreover, this technique specifically addresses the subchondral bone, a principal challenge of regenerative and reparative procedures designed to treat OCD. Limitations of this particular device include limited long-term follow-up results confirming reports of early effectiveness, comparison to other techniques and concern regarding abnormal MRI morphology reported to date [26, 43, 58]. Even though regenerated tissue was histologically analyzed in the study by Berruto et al. and was described as hyaline-like tissue with normal mineralization of the subchondral bone [9], MRI was of relatively low quality in comparison to standards. Brix et al. [17] found significantly lower tissue quality compared to healthy surrounding cartilage using T2 mapping and T2 zonal index MRI, with subchondral bone abnormality remaining a concerning finding although improving with time. Nonetheless, MRI signal after scaffold implantation has not been correlated with the clinical results, an observation consistent with some other type of cartilage surgery [44]. In this light, a recent cohort study on 27 patients showed MRI abnormalities at 5 years’ follow-up, in particular at the subchondral bone level, with an overall improvement of these features over time and a significant improvement and stable clinical results [84]. Longer term follow-up high quality studies are needed to further assess the impact of these MRI findings on the clinical results and to confirm cell-free scaffolds as a valid option in treating large non-reparable OCD lesions.
Discussion
The overall evidence documents positive results for each of the assorted surgical procedures applied to treat unstable OCD, thus indicating support for their selected use to treat osteochondral defects paying particular attention to their specific indications for the lesion characteristics. The restoration of the articular surface integrity is of major importance especially in young adults. In fact, in lesions left untreated or following simple fragment excision, early osteoarthritis can be anticipated [92]. Joint surface incongruence from symptomatic OCD alters the articular physiologic congruence, thus increasing the contact stress on adjacent joint surfaces, further accelerating wear and the cascade of joint degeneration [20].
Different solutions have been applied and variably studied to address OCD lesions. They include refixation of the detached fragment, bone marrow stimulation of the lesions, osteochondral autograft implantation or fresh osteochondral allograft transplantation and cell-based or cell-free regenerative techniques. Refixation of the fragment may represent the most anatomical procedure, but its limits lay on the quality of the detached fragment, which is often compromised at presentation. The best results with this approach are limited to immature patients with fragments remaining in situ. Bone marrow stimulation techniques are primarily chondral procedures, unable to properly treat large osteochondral lesions such as OCD, which is reflected by the lack of evidence for application of this technique in the setting of subchondral bone loss. ACI and MACT techniques, originally described as chondral procedures, have evolved with technical modifications including addition of autologous bone grafting and have shown excellent results for OCD in particular settings. However, these regenerative procedures do not restore an optimal osteochondral unit and present with significant limitations. As a two-step technique, with demanding technical surgical issues, significant regulatory restrictions varying among countries and significantly higher costs compared to other surgical alternatives, this approach has unique hurdles to becoming a routine rather than salvage approach around the world. Combining cell-based techniques with autologous bone graft harvesting further adds operative time and thus costs. For these reasons, some investigators have focused on single step techniques such as cell-free osteochondral scaffolds, other than osteochondral autografts or allografts, as first choice treatment for the large deep osteochondral lesions typical of late stage OCD.
In this light, it appears that procedures capable of restoring the entire osteochondral unit represent the best strategy for OCD. Osteochondral cell-free scaffolds have the advantage of an off-the-shelf product, while OAT allows to transplant a mosaic of living autologous osteochondral tissue. FOCA has the further benefit of avoiding the donor site morbidity, with more consistent long-term results and the capacity of addressing larger lesions, or even lesions at multiple sites. All these techniques provide good to excellent clinical results, but the lack of randomized trials or comparative studies across the spectrum of these approaches does not allow a clearly defined best option. However, the quality of the regenerated tissue obtained with these treatments and the ability of one technique to meet the majority of demands in patients with OCD, should be taken into account when considering the potential of these techniques. Except from sporadic studies analyzing histologic tissue repair, most of the present knowledge about tissue quality is provided by the segregate of indirect imaging studies. Unfortunately, such imaging has generally been shown to poorly correlate with clinical outcome, thus confusing correlation and interpretation. Imaging findings showed that the osteochondral scaffolds, which are growing in interest and application, still need to be improved to regenerate the autologous osteochondral unit, with good clinical results but abnormal findings both at the cartilage and bone level.
Thus, currently the best options to treat unstable OCD lesions in young adults, aiming to restore the osteochondral unit, remain either osteochondral autograft for small lesions or allograft transplantation for the more typical large lesion. Importantly, larger defects cannot be filled with OAT due to donor site morbidity and limited tissue availability, particularly important in young adults affected by large defects. As well, articular cartilage incongruence is technically challenging and problematic with the mosaic required. These limits are overcome by FOCA, which on the other hand suffers from other challenges in terms of universal applicability. The principal limitation for this technology surrounds the availability of tissue, rather than some limit to indications or outcome longevity. This stems from access to healthy donors and temporal limitations across the procurement and distribution process necessary to maintain chondrocyte viability. Most notably, meeting government regulations pertaining to aseptic collection and distribution of human tissue remain the principal reason patients cannot benefit from this well-established surgical therapy. Clinical factors potentially limiting applicability include size matching and graft congruence with native joint surface, incorporation to adjacent tissue, preservation of in vitro viability and potentially graft–host immunologic considerations [18, 28, 56, 93, 106]. Although there is no specific concern for systemic immunologic “rejection” phenomenon per se, and blood type matching is not required for this process, limiting the potential for antigenic exposure is strongly recommended as an essential element of both graft processing and implant procedures [22, 77, 93]. Practically, time from identification of adequate disease-free tissue to transplant and common post-operative rehabilitation restrictions place burden on surgical scheduling and patient acceptance [53]. However, advancements in FOCA technology and surgery and translational improvements are expected to elevate the access to, indications for and success of this burgeoning biologic joint reconstruction treatment.
Technological advances in handling, testing and storage have improved the accessibility of and potential for FOCA use [22, 28], especially in the USA, where standardization of tissue bank practices in concert with the AATB (American Association of Tissue Banks) has improved procurement and distribution of aseptic viable human tissue for transplant. This has been facilitated by governmental and regulatory agency policy guidelines that promote accountability within health systems by establishing uniform process, to best assure the safety and compliance chain for managing this valuable biologic therapeutic [74]. Further to this, the translation of these scientific and logistical advances has expanded the potential for clinical application of FOCA which is uniquely able to restore articular structure biologically [106], while maintaining cell viability and chondrogenic activity in situ, at levels analogous to adjacent host cartilage [19, 73]. These efforts have allowed for remarkable patient satisfaction, associated with predictable improved functional outcomes for both primary and salvage cartilage reconstruction procedures for OCD [6, 25, 39, 48, 100]. Thus, until technological improvements optimize the regenerative potential of cell-based or cell-free osteochondral treatments, FOCA currently represent the best option to restore the articular surface with viable physiologic osteochondral tissue. This, together with the long-term outcomes documented, prompts the need to invest efforts aimed at overcoming the regulatory restrictions and organization issues that limit the access to this procedure, currently available in a few countries, to extend the possibility to successfully treat unstable OCD lesion in young adults.
Conclusion
Different surgical strategies have been proposed to address unstable OCD lesions. The fixation of a good quality fragment(s) should be pursued as a first option, while unfixable small lesions may benefit from OAT. For large lesions, available cell-based or cell-free osteochondral scaffold are a feasible solution but with limitation in term of regenerated tissue quality. In this light, fresh allografts are well known to allow to obtain articular surface restoration with viable physiologic osteochondral tissue providing a predictably successful outcome, and therefore they may currently represent the most suitable option to treat unstable irreparable OCD lesion in young adults.
References
https://www.fda.gov/BiologicsBloodVaccines/TissueTissueProducts/default.htm. Accessed 9 Oct 2018
Aglietti P, Ciardullo A, Giron F, Ponteggia F (2001) Results of arthroscopic excision of the fragment in the treatment of osteochondritis dissecans of the knee. Arthroscopy 17:741–746
Anderson AF, Pagnani MJ (1997) Osteochondritis dissecans of the femoral condyles. Long-term results of excision of the fragment. Am J Sports Med 25:830–834
Andriolo L, Candrian C, Papio T, Cavicchioli A, Perdisa F, Filardo G (2018) Osteochondritis dissecans of the knee-conservative treatment strategies: a systematic review. Cartilage. https://doi.org/10.1177/1947603518758435
Andriolo L, Crawford DC, Reale D, Zaffagnini S, Candrian C, Cavicchioli A et al (2018) Osteochondritis Dissecans of the Knee: Etiology and Pathogenetic Mechanisms. A Systematic Review. Cartilage. https://doi.org/10.1177/1947603518786557
Assenmacher AT, Pareek A, Reardon PJ, Macalena JA, Stuart MJ, Krych AJ (2016) Long-term outcomes after osteochondral allograft: a systematic review at long-term follow-up of 12.3 years. Arthroscopy 32:2160–2168
Barrett I, King AH, Riester S, van Wijnen A, Levy BA, Stuart MJ et al (2016) Internal fixation of unstable osteochondritis dissecans in the skeletally mature knee with metal screws. Cartilage 7:157–162
Bartlett W, Gooding CR, Carrington RW, Skinner JA, Briggs TW, Bentley G (2005) Autologous chondrocyte implantation at the knee using a bilayer collagen membrane with bone graft. A preliminary report. J Bone Joint Surg Br 87:330–332
Berruto M, Ferrua P, Uboldi F, Pasqualotto S, Ferrara F, Carimati G et al (2016) Can a biomimetic osteochondral scaffold be a reliable alternative to prosthetic surgery in treating late-stage SPONK? Knee 23:936–941
Bhattacharjee A, McCarthy HS, Tins B, Roberts S, Kuiper JH, Harrison PE et al (2016) Autologous bone plug supplemented with autologous chondrocyte implantation in osteochondral defects of the knee. Am J Sports Med 44:1249–1259
Black LO, Ko JK, Quilici SM, Crawford DC (2016) Fresh osteochondral allograft to the humeral head for treatment of an engaging reverse hill-sachs lesion: technical case report and literature review. Orthop J Sports Med 4:2325967116670376
Bohndorf K (1998) Osteochondritis (osteochondrosis) dissecans: a review and new MRI classification. Eur Radiol 8:103–112
Bradley J, Dandy DJ (1989) Results of drilling osteochondritis dissecans before skeletal maturity. J Bone Joint Surg Br 71:642–644
Brittberg M (2012) How to treat patients with osteochondritis dissecans (juvenile and adult). In: Brittberg M, Gobbi A, Imhoff A, Kon E, Madry H (eds) Cartilage repair. Clinical guidelines. DJO Publications, Guildford, pp 171–184
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331:889–895
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85 A Suppl 2:58–69
Brix M, Kaipel M, Kellner R, Schreiner M, Apprich S, Boszotta H et al (2016) Successful osteoconduction but limited cartilage tissue quality following osteochondral repair by a cell-free multilayered nano-composite scaffold at the knee. Int Orthop 40:625–632
Brown D, Shirzad K, Lavigne SA, Crawford DC (2011) Osseous integration after fresh osteochondral allograft transplantation to the distal femur: a prospective evaluation using computed tomography. Cartilage 2:337–345
Brown DS, Durkan MG, Foss EW, Szumowski J, Crawford DC (2014) Temporal in vivo assessment of fresh osteochondral allograft transplants to the distal aspect of the femur by dGEMRIC (delayed gadolinium-enhanced MRI of cartilage) and zonal T2 mapping MRI. J Bone Joint Surg Am 96:564–572
Buckwalter JA, Anderson DD, Brown TD, Tochigi Y, Martin JA (2013) The Roles of mechanical stresses in the pathogenesis of osteoarthritis: implications for treatment of joint injuries. Cartilage 4:286–294
Bugbee WD, Convery FR (1999) Osteochondral allograft transplantation. Clin Sports Med 18:67–75
Bugbee WD, Pallante-Kichura AL, Gortz S, Amiel D, Sah R (2016) Osteochondral allograft transplantation in cartilage repair: Graft storage paradigm, translational models, and clinical applications. J Orthop Res 34:31–38
Camathias C, Gogus U, Hirschmann MT, Rutz E, Brunner R, Haeni D et al (2015) Implant failure after biodegradable screw fixation in osteochondritis dissecans of the knee in skeletally immature patients. Arthroscopy 31:410–415
Carey JL, Wall EJ, Grimm NL, Ganley TJ, Edmonds EW, Anderson AF et al (2016) Novel arthroscopic classification of osteochondritis dissecans of the knee: a multicenter reliability study. Am J Sports Med 44:1694–1698
Chahal J, Gross AE, Gross C, Mall N, Dwyer T, Chahal A et al (2013) Outcomes of osteochondral allograft transplantation in the knee. Arthroscopy 29:575–588
Christensen BB, Foldager CB, Jensen J, Jensen NC, Lind M (2016) Poor osteochondral repair by a biomimetic collagen scaffold: 1- to 3-year clinical and radiological follow-up. Knee Surg Sports Traumatol Arthrosc 24:2380–2387
Cole BJ, DeBerardino T, Brewster R, Farr J, Levine DW, Nissen C et al (2012) Outcomes of autologous chondrocyte implantation in study of the treatment of articular repair (STAR) patients with osteochondritis dissecans. Am J Sports Med 40:2015–2022
Cook JL, Stoker AM, Stannard JP, Kuroki K, Cook CR, Pfeiffer FM et al (2014) A novel system improves preservation of osteochondral allografts. Clin Orthop Relat Res 472:3404–3414
Cotter EJ, Frank RM, Wang KC, Totlis T, Poland S, Meyer MA et al (2018) Clinical outcomes of osteochondral allograft transplantation for secondary treatment of osteochondritis dissecans of the knee in skeletally mature patients. Arthroscopy 34:1105–1112
Crawford DC (2017) Personal communication. Metrics of Osteochondral Allograft Study Group Meeting, Chicago
Crawford DC, Safran MR (2006) Osteochondritis dissecans of the knee. J Am Acad Orthop Surg 14:90–100
Cugat R, Garcia M, Cusco X, Monllau JC, Vilaro J, Juan X et al (1993) Osteochondritis dissecans: a historical review and its treatment with cannulated screws. Arthroscopy 9:675–684
Dean CS, Chahla J, Serra Cruz R, LaPrade RF (2016) Fresh osteochondral allograft transplantation for treatment of articular cartilage defects of the knee. Arthrosc Tech 5:e157–e161
Delcogliano M, Menghi A, Placella G, Speziali A, Cerulli G, Carimati G et al (2014) Treatment of osteochondritis dissecans of the knee with a biomimetic scaffold. A prospective multicenter study. Joints 2:102–108
Detterline AJ, Goldstein JL, Rue JP, Bach BR Jr (2008) Evaluation and treatment of osteochondritis dissecans lesions of the knee. J Knee Surg 21:106–115
Dines JS, Fealy S, Potter HG, Warren RF (2008) Outcomes of osteochondral lesions of the knee repaired with a bioabsorbable device. Arthroscopy 24:62–68
Drez D Jr (2012) Antegrade versus retrograde. Am J Sports Med 40:NP7; author reply NP7
Ellermann JM, Donald B, Rohr S, Takahashi T, Tompkins M, Nelson B et al (2016) Magnetic resonance imaging of osteochondritis dissecans: validation study for the ICRS classification system. Acad Radiol 23:724–729
Emmerson BC, Gortz S, Jamali AA, Chung C, Amiel D, Bugbee WD (2007) Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med 35:907–914
Federico DJ, Lynch JK, Jokl P (1990) Osteochondritis dissecans of the knee: a historical review of etiology and treatment. Arthroscopy 6:190–197
Filardo G, Drobnic M, Perdisa F, Kon E, Hribernik M, Marcacci M (2014) Fibrin glue improves osteochondral scaffold fixation: study on the human cadaveric knee exposed to continuous passive motion. Osteoarthritis Cartilage 22:557–565
Filardo G, Kon E, Berruto M, Di Martino A, Patella S, Marcheggiani Muccioli GM et al (2012) Arthroscopic second generation autologous chondrocytes implantation associated with bone grafting for the treatment of knee osteochondritis dissecans: Results at 6 years. Knee 19:658–663
Filardo G, Kon E, Di Martino A, Busacca M, Altadonna G, Marcacci M (2013) Treatment of knee osteochondritis dissecans with a cell-free biomimetic osteochondral scaffold: clinical and imaging evaluation at 2-year follow-up. Am J Sports Med 41:1786–1793
Filardo G, Kon E, Di Martino A, Perdisa F, Busacca M, Tentoni F et al (2014) Is the clinical outcome after cartilage treatment affected by subchondral bone edema? Knee Surg Sports Traumatol Arthrosc 22:1337–1344
Fokter SK, Strahovnik A, Kos D, Dovnik A, Fokter N (2012) Long term results of operative treatment of knee osteochondritis dissecans. Wien Klin Wochenschr 124:699–703
Garrett JC (1994) Fresh osteochondral allografts for treatment of articular defects in osteochondritis dissecans of the lateral femoral condyle in adults. Clin Orthop Relat Res 33–37
Gracitelli GC, Meric G, Pulido PA, Gortz S, De Young AJ, Bugbee WD (2015) Fresh osteochondral allograft transplantation for isolated patellar cartilage injury. Am J Sports Med 43:879–884
Gracitelli GC, Meric G, Pulido PA, McCauley JC, Bugbee WD (2015) Osteochondral allograft transplantation for knee lesions after failure of cartilage repair surgery. Cartilage 6:98–105
Grimm NL, Weiss JM, Kessler JI, Aoki SK (2014) Osteochondritis dissecans of the knee: pathoanatomy, epidemiology, and diagnosis. Clin Sports Med 33:181–188
Gudas R, Simonaityte R, Cekanauskas E, Tamosiunas R (2009) A prospective, randomized clinical study of osteochondral autologous transplantation versus microfracture for the treatment of osteochondritis dissecans in the knee joint in children. J Pediatr Orthop 29:741–748
Hefti F, Beguiristain J, Krauspe R, Moller-Madsen B, Riccio V, Tschauner C et al (1999) Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B 8:231–245
Hughston JC, Hergenroeder PT, Courtenay BG (1984) Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg Am 66:1340–1348
Kane MS, Lau K, Crawford DC (2017) Rehabilitation and postoperative management practices after osteochondral allograft transplants to the distal femur: a report from the metrics of osteochondral allografts (MOCA) study group 2016 survey. Sports Health. https://doi.org/10.1177/1941738117717011
Kivisto R, Pasanen L, Leppilahti J, Jalovaara P (2002) Arthroscopic repair of osteochondritis dissecans of the femoral condyles with metal staple fixation: a report of 28 cases. Knee Surg Sports Traumatol Arthrosc 10:305–309
Kocher MS, Tucker R, Ganley TJ, Flynn JM (2006) Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med 34:1181–1191
Koh JL, Kowalski A, Lautenschlager E (2006) The effect of angled osteochondral grafting on contact pressure: a biomechanical study. Am J Sports Med 34:116–119
Kon E, Delcogliano M, Filardo G, Altadonna G, Marcacci M (2009) Novel nano-composite multi-layered biomaterial for the treatment of multifocal degenerative cartilage lesions. Knee Surg Sports Traumatol Arthrosc 17:1312–1315
Kon E, Filardo G, Di Martino A, Busacca M, Moio A, Perdisa F et al (2014) Clinical results and MRI evolution of a nano-composite multilayered biomaterial for osteochondral regeneration at 5 years. Am J Sports Med 42:158–165
Kon E, Mutini A, Arcangeli E, Delcogliano M, Filardo G, Nicoli Aldini N et al (2010) Novel nanostructured scaffold for osteochondral regeneration: pilot study in horses. J Tissue Eng Regen Med 4:300–308
Kon E, Roffi A, Filardo G, Tesei G, Marcacci M (2015) Scaffold-based cartilage treatments: with or without cells? A systematic review of preclinical and clinical evidence. Arthroscopy 31:767–775
Konig F (2013) The classic: on loose bodies in the joint. 1887. Clin Orthop Relat Res 471:1107–1115
Kouzelis A, Plessas S, Papadopoulos AX, Gliatis I, Lambiris E (2006) Herbert screw fixation and reverse guided drillings, for treatment of types III and IV osteochondritis dissecans. Knee Surg Sports Traumatol Arthrosc 14:70–75
Kramer DE, Glotzbecker MP, Shore BJ, Zurakowski D, Yen YM, Kocher MS et al (2015) Results of surgical management of osteochondritis dissecans of the ankle in the pediatric and adolescent population. J Pediatr Orthop 35:725–733
LaPrade RF, Bursch LS, Olson EJ, Havlas V, Carlson CS (2008) Histologic and immunohistochemical characteristics of failed articular cartilage resurfacing procedures for osteochondritis of the knee: a case series. Am J Sports Med 36:360–368
Levy YD, Gortz S, Pulido PA, McCauley JC, Bugbee WD (2013) Do fresh osteochondral allografts successfully treat femoral condyle lesions? Clin Orthop Relat Res 471:231–237
Linden B (1976) The incidence of osteochondritis dissecans in the condyles of the femur. Acta Orthop Scand 47:664–667
Linden B (1977) Osteochondritis dissecans of the femoral condyles: a long-term follow-up study. J Bone Joint Surg Am 59:769–776
Louisia S, Beaufils P, Katabi M, Robert H (2003) Transchondral drilling for osteochondritis dissecans of the medial condyle of the knee. Knee Surg Sports Traumatol Arthrosc 11:33–39
Lyon R, Nissen C, Liu XC, Curtin B (2013) Can fresh osteochondral allografts restore function in juveniles with osteochondritis dissecans of the knee? Clin Orthop Relat Res 471:1166–1173
Magnussen RA, Carey JL, Spindler KP (2009) Does operative fixation of an osteochondritis dissecans loose body result in healing and long-term maintenance of knee function? Am J Sports Med 37:754–759
Makino A, Muscolo DL, Puigdevall M, Costa-Paz M, Ayerza M (2005) Arthroscopic fixation of osteochondritis dissecans of the knee: clinical, magnetic resonance imaging, and arthroscopic follow-up. Am J Sports Med 33:1499–1504
Marcacci M, Filardo G, Kon E (2013) Treatment of cartilage lesions: what works and why? Injury 44(Suppl 1):S11–S15
Maury AC, Safir O, Heras FL, Pritzker KP, Gross AE (2007) Twenty-five-year chondrocyte viability in fresh osteochondral allograft. A case report. J Bone Joint Surg Am 89:159–165
McAllister DR, Joyce MJ, Mann BJ, Vangsness CT Jr (2007) Allograft update: the current status of tissue regulation, procurement, processing, and sterilization. Am J Sports Med 35:2148–2158
Merchan EC, Galindo E (1991) Cannulated screw breaking in arthroscopic surgery of osteochondritis dissecans of the knee: a case report. Arthroscopy 7:108–110
Mesgarzadeh M, Sapega AA, Bonakdarpour A, Revesz G, Moyer RA, Maurer AH et al (1987) Osteochondritis dissecans: analysis of mechanical stability with radiography, scintigraphy, and MR imaging. Radiology 165:775–780
Meyer MA, McCarthy MA, Gitelis ME, Poland SG, Urita A, Chubinskaya S et al (2017) Effectiveness of lavage techniques in removing immunogenic elements from osteochondral allografts. Cartilage 8:369–373
Miniaci A, Tytherleigh-Strong G (2007) Fixation of unstable osteochondritis dissecans lesions of the knee using arthroscopic autogenous osteochondral grafting (mosaicplasty). Arthroscopy 23:845–851
Mirzayan R, Lim MJ (2016) Fresh osteochondral allograft transplantation for osteochondritis dissecans of the capitellum in baseball players. J Shoulder Elbow Surg 25:1839–1847
Murphy RT, Pennock AT, Bugbee WD (2014) Osteochondral allograft transplantation of the knee in the pediatric and adolescent population. Am J Sports Med 42:635–640
Nakagawa T, Kurosawa H, Ikeda H, Nozawa M, Kawakami A (2005) Internal fixation for osteochondritis dissecans of the knee. Knee Surg Sports Traumatol Arthrosc 13:317–322
Niemeyer P, Laute V, John T, Becher C, Diehl P, Kolombe T et al (2016) The effect of cell dose on the early magnetic resonance morphological outcomes of autologous cell implantation for articular cartilage defects in the knee: a randomized clinical trial. Am J Sports Med 44:2005–2014
Niethammer TR, Pietschmann MF, Horng A, Rossbach BP, Ficklscherer A, Jansson V et al (2014) Graft hypertrophy of matrix-based autologous chondrocyte implantation: a two-year follow-up study of NOVOCART 3D implantation in the knee. Knee Surg Sports Traumatol Arthrosc 22:1329–1336
Perdisa F, Kon E, Sessa A, Andriolo L, Busacca M, Marcacci M et al (2018) Treatment of knee osteochondritis dissecans with a cell-free biomimetic osteochondral scaffold: clinical and imaging findings at midterm follow-up. Am J Sports Med 46:314–321
Peterson L, Minas T, Brittberg M, Lindahl A (2003) Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: results at two to ten years. J Bone Joint Surg Am 85 A Suppl 2:17–24
Peterson L, Minas T, Brittberg M, Nilsson A, Sjögren-Jansson E, Lindahl A (2000) 2- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res 212–234
Provencher M (2016) Personal communication. Metrics of osteochondral allograft study group meeting, Centenial.
Robert H, Elise S, Dubois H (1998) Osteochondritis dissecans of the knee, results of 43 refixations. Arthroskopie 11:177–181
Sadlik B, Gobbi A, Puszkarz M, Klon W, Whyte GP (2017) Biologic inlay osteochondral reconstruction: arthroscopic one-step osteochondral lesion repair in the knee using morselized bone grafting and hyaluronic acid-based scaffold embedded with bone marrow aspirate concentrate. Arthrosc Tech 6:e383–e389
Sadr KN, Pulido PA, McCauley JC, Bugbee WD (2016) Osteochondral allograft transplantation in patients with osteochondritis dissecans of the knee. Am J Sports Med 44:2870–2875
Sales de Gauzy J, Mansat C, Darodes PH, Cahuzac JP (1999) Natural course of osteochondritis dissecans in children. J Pediatr Orthop B 8:26–28
Sanders TL, Pareek A, Obey MR, Johnson NR, Carey JL, Stuart MJ et al (2017) High rate of osteoarthritis after osteochondritis dissecans fragment excision compared with surgical restoration at a mean 16-year follow-up. Am J Sports Med 45:1799–1805
Sherman SL, Garrity J, Bauer K, Cook J, Stannard J, Bugbee W (2014) Fresh osteochondral allograft transplantation for the knee: current concepts. J Am Acad Orthop Surg 22:121–133
Smolders JM, Kock NB, Koeter S, Van Susante JL (2010) Osteochondral autograft transplantation for osteochondritis dissecans of the knee. Preliminary results of a prospective case series. Acta Orthop Belg 76:208–218
Steadman JR, Rodkey WG, Briggs KK, Rodrigo JJ (1999) [The microfracture technic in the management of complete cartilage defects in the knee joint]. Orthopade 28:26–32
Steinhagen J, Bruns J, Deuretzbacher G, Ruether W, Fuerst M, Niggemeyer O (2010) Treatment of osteochondritis dissecans of the femoral condyle with autologous bone grafts and matrix-supported autologous chondrocytes. Int Orthop 34:819–825
Tabaddor RR, Banffy MB, Andersen JS, McFeely E, Ogunwole O, Micheli LJ et al (2010) Fixation of juvenile osteochondritis dissecans lesions of the knee using poly 96L/4D-lactide copolymer bioabsorbable implants. J Pediatr Orthop 30:14–20
Tarabella V, Filardo G, Di Matteo B, Andriolo L, Tomba P, Vigano A et al (2016) From loose body to osteochondritis dissecans: a historical account of disease definition. Joints 4:165–170
Thomson NL (1987) Osteochondritis dissecans and osteochondral fragments managed by Herbert compression screw fixation. Clin Orthop Relat Res 71–78
Torrie AM, Kesler WW, Elkin J, Gallo RA (2015) Osteochondral allograft. Curr Rev Musculoskelet Med 8:413–422
Vannini F, Battaglia M, Buda R, Cavallo M, Giannini S (2012) “One step” treatment of juvenile osteochondritis dissecans in the knee: clinical results and T2 mapping characterization. Orthop Clin North Am 43:237–244, vi
VanTienderen RJ, Dunn JC, Kusnezov N, Orr JD (2017) Osteochondral allograft transfer for treatment of osteochondral lesions of the talus: a systematic review. Arthroscopy 33:217–222
Vijayan S, Bartlett W, Bentley G, Carrington RW, Skinner JA, Pollock RC et al (2012) Autologous chondrocyte implantation for osteochondral lesions in the knee using a bilayer collagen membrane and bone graft: a 2- to 8-year follow-up study. J Bone Joint Surg Br 94:488–492
Wang CJ (2002) Treatment of focal articular cartilage lesions of the knee with autogenous osteochondral graftsA 2- to 4-year follow-up study. Arch Orthop Trauma Surg 122:169–172
Weckstrom M, Parviainen M, Kiuru MJ, Mattila VM, Pihlajamaki HK (2007) Comparison of bioabsorbable pins and nails in the fixation of adult osteochondritis dissecans fragments of the knee: an outcome of 30 knees. Am J Sports Med 35:1467–1476
Williams III RJ, Ranawat AS, Potter HG, Carter T, Warren RF (2007) Fresh stored allografts for the treatment of osteochondral defects of the knee. J Bone Joint Surg Am 89:718–726
Yonetani Y, Matsuo T, Nakamura N, Natsuume T, Tanaka Y, Shiozaki Y et al (2010) Fixation of detached osteochondritis dissecans lesions with bioabsorbable pins: clinical and histologic evaluation. Arthroscopy 26:782–789
Yoshizumi Y, Sugita T, Kawamata T, Ohnuma M, Maeda S (2002) Cylindrical osteochondral graft for osteochondritis dissecans of the knee: a report of three cases. Am J Sports Med 30:441–445
Zellner J, Grechenig S, Pfeifer CG, Krutsch W, Koch M, Welsch G et al (2017) Clinical and radiological regeneration of large and deep osteochondral defects of the knee by bone augmentation combined with matrix-guided autologous chondrocyte transplantation. Am J Sports Med 45:3069–3080
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
GF is a consultant for Finceramica Faenza Spa, Fidia Farmaceutica, Cartiheal Ltd, EON medica; received institutional support from Finceramica Faenza Spa, Fidia Farmaceutica, IGEA Biomedical, Zimmer Biomet, Kensey Nash. PV is a consultant for DePuy Synthes, Smith and Nephew, Conmed, Active implants. LA, FS, MB, PF, FR and DCC have nothing to disclose.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Filardo, G., Andriolo, L., Soler, F. et al. Treatment of unstable knee osteochondritis dissecans in the young adult: results and limitations of surgical strategies—The advantages of allografts to address an osteochondral challenge. Knee Surg Sports Traumatol Arthrosc 27, 1726–1738 (2019). https://doi.org/10.1007/s00167-018-5316-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5316-5