Abstract
We evaluated the outcome in 10 young patients, ages ranging from 15 to 26, with types III and IV osteochondritis dissecans of the knee, treated with Herbert screws fixation and reverse guided drillings. The disease involved the medial femoral condyle in eight patients and the lateral in two. Diagnosis and preoperative planning based on plain radiographs (AP, lateral and tunnel view) and MRI (in seven patients). Fixation of the fragment with Herbert screws using a mini-arthrotomy technique and additional reverse drillings behind the crater of the lesion using the ACL aiming devise were performed in all patients. Post-operatively, no weight bearing was recommended for at least three months. The follow-up ranged from 15 months to 38 months (mean 27 months). According to the subjective questionnaire of the International Cartilage Repair Society (ICRS) scale, seven patients had normal knees, two had nearly normal knees and one abnormal. The Lysholm Knee score ranged 65–96 points (mean 88 points). All patients except one returned to their previous activities and they were satisfied with the result. Radiological union of the fragment was found in 9/10 patients (six grade III, three grade IV). Progressive flattening of the injured femoral condyle was noticed in two patients (grade III). Securing the lesion using Herbert screws in combination with reverse guided drillings seems to be an effective treatment choice for detached or displaced osteochondral fragments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteochondritis dissecans (OCD) is characterized by separation of a fragment of bone with overlying articular cartilage from the surrounding normal bone. The disease evolves in four stages [6]: depressed osteochondral fracture (stage I), osteochondral fragment attached by an osseous bridge (stage II), detached non-displaced fragment (stage III), displaced fragment (stage IV).
Arthroscopic surgical management of OCD and osteochondral fragments has increased in popularity in recent years. Various arthroscopic techniques such as drilling [16], grafting [8] or fixation have been proposed over the past few years, for treatment of this condition. Bone pegs [14, 19] Kirshner wires [3, 9, 15], compression screws [11] or pins [10], biodegradable rods [7] and metal staples [13] have been used. However, these methods have weaknesses and no generally accepted arthroscopic fixation method exists.
The methods of treatment, for stages III and IV lesions, are debated and several options are available: drilling in situ, removal of the fragment with debridement and drilling of the crater, fragment re-fixation, or osteochondral grafting.
The purpose of this study was to evaluate the clinical results and the radiographic findings after treatment using Herbert’s compression screw fixation technique in detached fragments (type 3 and 4), in addition to reverse guided drillings.
Patients and methods
Between 1998 and 2002, 10 young patients (one female and nine males), ages ranging from 15 years to 26 years (mean 21 years) underwent surgical fixation of a detached osteochondral fragment (seven grade III and three grade IV) of one of the femoral condyles (Table 1). Three of the patients were juveniles and seven adults. The disease involved the medial femoral condyle in eight patients and the lateral in two. Two patients had open physes at the time of surgery. The average duration of symptoms before operation was 13 months (range from 1 months to 30 months). Seven of the patients had a history of trauma to the involved knee (70%). In four of them, this occurred during daily activities and in three, during sports. Preoperative diagnosis made by plain radiographs (AP, lateral and tunnel view) and MRI (in seven patients).
Preoperative functional status of the patients was recorded at the time of hospital admittance, to the ICRS form. Six of them reported symptoms during sports activities while the remaining four complained of mild pain during activities of daily living. None of them was a professional athlete. Concerning sports participation, two patients were involved in class I activities (competitive sports), three in class II (frequent sports), and one in class III (occasional sports).
The location of the lesion was defined from preoperative radiography according to the method of Cahill and Berg [5] while the size definition depended mostly on MRI T1 and T2 weighted images [12]. The three dimensions of the lesion (width, length and area) were measured better on the MRI films (Fig. 1). The average width of the lesion was 1.8 cm, the average length 2.4 cm and average area 4.22 cm2.
All patients were assessed clinically and radiographically once a month for the first 6 months after operation and then every 2 months for the first year. They were also interviewed at follow up for any residual symptoms and underwent a routine clinical and radiological examination. Healing was evaluated radiologically according to Dervin et al.[7].
Final clinical and radiological evaluation was performed for the needs of this study. Clinical assessment based on ICRS evaluating form, which separately evaluates subjective assessment, symptoms of pain, swelling and giving way, range of motion and objective stability. They also answered a modification of Lysholm Knee Score.
Fixation of the fragment with Herbert screws using a mini arthrotomy technique and additional reverse drillings behind the crater of the lesion using the aiming devise of the ACL instruments were performed in all patients.
Surgical technique
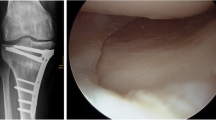
All patients were treated at first arthroscopically, with curettage and debridement of the interposing fibrous tissue. The anterolateral approach was used for the arthroscope, the anteromedial for the instruments, and the superolateral for the inflow. The crater of the lesion was always inspected with a prone hook and the size of the lesion was accurately demarcated. Any effort to remove the attached fragments for reshaping or crater drilling was avoided. For this reason, reverse drillings of the crater were performed using the angular guide instrument for the tibial tunnel of the ACL reconstruction, through a parapatellar incision of 2 cm, in order to achieve the best targeting of the subchondral bone inside the crater (Fig. 2). In the cases of displaced fragments, refreshing of the crater and autologous bone grafting was also performed. After a temporary stabilization of the fragment with a Kirshner wire, the Herbert screw guide was inserted with the knee flexed to 90°(Fig. 3). The screw head was always buried below the articular surface to contact the bone, to gain compression and to avoid protrusion that could erode the opposite tibial surface. Second or even third or fourth screws were used when size permitted according to lesion’s measurements (size and depth) on MRI films in order to have rotational stability and secure fixation of the fragment. More than one screw was used in six cases. Small loose bodies were removed in three knees.
Postoperatively, a Robert–Jones bounding was set with an elastic bandage. Full range of motion was encouraged from the first postoperative day. Quadriceps muscle isometric exercises and patella mobilization were also begun during the same time. Weight bearing was restricted for 8–12 weeks in relation to the size and location of the injured area.
Results
The mean follow-up of the patients was 27 months (15–38 months). According to the subjective questionnaire of the ICRS scale, seven patients had normal knees, two had nearly normal knees and one abnormal (Table 2). The Lysholm Knee score was 65–96 points (mean 88 points). An extension loss of 5° compared with the other knee was found in one patient. All knees were stable at the follow-up examination.
Postoperatively, function improved in all patients except one who described restriction during activities of daily living. All other nine patients returned to their previous daily and sport activities including one patient with radiographic degenerative changes of the knee.
Radiological union of the fragment was found in nine patients (6 grade III, 3 grade IV) during the tenth postoperative month (Fig. 4). Union of the fragment was considered according to (a) the common radiological criteria for fragments union (occious bridging, disappearing of the fracture line), (b) the lack of pain after weight bearing, and (c) the evidence that fragment collapse has been avoided. In one patient (grade III) the fragment collapsed inside the joint during the 11th postoperative month because of wrong technique. The AP radiographic projection showed progressive flattening of the injured femoral condyle in two patients (grade III). No case of screw migration or breakage was noticed.
There was no significant correlation between the location of the chondral fragment and clinical results, while no significant differences were found between clinical and radiographic results.
Until now, only one patient had to be reoperated in order to remove the non- healed loose fragment and to replace the gap with an osteochondral autograft (mosaic plasty).
Discussion
The age of the patient, the mechanical stability of the fragment, the fragment dimensions and the degree of deterioration are the most important factors for the treatment of OCD. Stable lesions are usually treated conservatively by decreasing limp activity and weight bearing at least for 2 months, while unstable fragments, especially those in the weight bearing surface, require some kind of surgical treatment.
The poor results following detached fragment removal, specially over 2 cm in size, in a weight-bearing area of the condyles are well-known and are reported by several authors [2, 4]. Internal fixation seems to be an indispensable and optimal method for loose bodies and unstable partial detached lesions and some different methods of fixation are reported in the literature. Smillie [20] was one of the first to describe fixation of a separated osteochondritis dissecans lesion with use of pins. Lipscomb et al. [15] used Kirschner wires to reattach a large fragment and emphasized the importance of removal of the fibrous tissue at the base of the crater, drilling of the bed of the defect to increase vascularity, and use of bone graft to restore the congruity of the joint surfaces if necessary. Slough et al. [19] reported good results with use of bone-peg fixation in eight of ten knees (nine patients), on an average of 2.9 years. Anderson et al. [3] treated 17 knees with curettage, bone grafting and pinning. Of these knees 12% were graded as excellent and 53% as good after a follow-up of 5–7 years. Aglietti et al. [1] reported excellent results (100% healing) after arthroscopically drilling in 16 OCD lesions in children.
The previous methods had different kinds of problems. Arthroscopic pinning using Kirschner wire fixation has shown several complications [9]. Technical advancements using drill guides for alignment have improved on this technique but mobility is restricted by the wires impinging on soft tissue.
Fixation with metal staples has also been recently reported, but despite their theoretical superiority, they have some harmful disadvantages, such as the breakdown of the staple, which leads to a repeat operation [13].
The use of the Herbert compression screw is an alternative method of fixation, which provides both additional stability and compression of the separated fragment. Thomson [21] reported radiographic union in three patients with separated and 8/10 with unseparated osteochondral fragments who had been managed with Herbert compression-screw fixation. Wombwell and Nunley [22] reported healing in one patient with large and unstable medial condylar fragment with the use of this technique. Mackie et al. [17] inserted Herbert screws under arthroscopic guidance in three patients who had early-stage osteochondritis dissecans. The patients were allowed to bear weight immediately and had a decrease in symptoms at the one-year follow-up evaluation. Rey Zuniga et al. [18] treated 11 patients with symptomatic OCD of the medial condyle with Herbert screws, in conjunction or not with absorbable pins, and reported 81.8% excellent or good results at 16.3 months follow-up.
As for the treatment, in our series we emphasize on the two main principles that characterize the disease. The first one concerns the role of subchondral bone in the pathogenesis of OCD and the second one the fact that we have to deal with a fracture.
It is generally recognized that the target tissue in OCD is the subchondral bone of the distal femoral condyle, rather than the articular cartilage. Stress fractures may develop in subchondral tissue, subjected to cyclic and cumulative stresses. This subchondral injury may then provoke vascular compromise, resulting in the typical OCD lesion of a variably viable bone nucleus covered with intact articular cartilage. The exact definition of the size and the depth of the lesion crater and the percentage of the subchondral bone involved, is crucial in order to achieve rigid fixation and revascularization of the fragment.
In our study, we found that MRI is a very helpful and reliable method for the right preoperative planning because of the accurate estimation of the extent of subchondral participation. In seven of the cases there has been a preoperative estimation not only of the crater dimensions but also of the number and the location of the screws on the fragment surface that we had to use, according to the MRI findings. We also believe that the intraoperative targeting of the lesion with the ACL targeting device is a quite sufficient method that permits safe and accurate drilling of the lesion crater without damaging the surrounding cartilage and the contact area between the fragment and the crater. Reverse guided drillings promotes the revascularization of the subchondral bone leading to early bone healing.
The second basic principle that defined the method we treated these lesions was that we regarded them as typical subchondral fractures so that the principles of fracture treatment can be applied. We tried not only to fix the fragment in its place but to achieve compression osteosynthesis in order to create the right biological and biomechanical environment for bone union. We prefer Herbert’s compression screws because of their two main characteristics, strong compression and burring of their head under the articular surface in order to prevent protrusion of the opposite articular cartilage. Intraoperatively, fixation of the lesion with Herbert compression screws provided rigid fixation, which allowed early joint motion because of the anatomical restoration of the joint surface.
In conclusion, the objective of the surgical treatment of the OCD must be to restore the joint surface to a normal configuration and to establish early postoperative motion. The concept of our method is not new but the reverse guided drilling method using the ACL aiming device and the preoperative planning based on MRI evaluation may play an important role in the healing of the lesion.
References
Aglietti P, Buzzi R, Bass PB, Frioriti M (1994) Arthroscopic drilling in juvenile osteochondritis dissecans of the medial femoral condyle. Arthroscopy 10:286–291
Aglietti P, Ciardullo A, Giron F, Ponteggia F (2001) Results of arthroscopic excision of the fragment in the treatment of osteochondritis dissecans of the knee. J Arthrosc Rel Surg 7:741–746
Anderson AF, Lipscomb AB, Coulam C (1990) Antegrade curettement, bone grafting and pinning of osteochondritis dissecans in the skeletally mature knee. Am J Sports Med 18:254–261
Cahill BR (1995) Osteochondritis dissecans of the knee: treatment of juvenile and adult forms. J Am Acad Orthop Surg 3:237–247
Cahill BR, Berg BC (1983) 99m-Technetium phosphate compound joint scintigraphy in the management of juvenile osteochondritis dissecans of the femoral condyles. Am J Sports Med 11:329–335
Clanton TO, DeLee JC (1982) Osteochondritis dissecans: history, pathophysiology and current treatment concepts. Clin Orthop 167:50–64
Dervin G, Keene G, Chissell H (1998) Biodegradable rods in adult osteochondritis dissecans of the knee. Clin Orthop 356:213–221
Greville NR (1964) Osteochondritis dissecans: treatment by bone grafting. Southern Med J 57:886–893
Jaberi FM (2002) Osteochondritis dissecans of the weight-bearing surface of the medial femoral condyle in adults. Knee 9(3):201–207
Jakob R, Miniaci A (1989) A compression pinning system for osteochondritis dissecans of the knee. Acta Orthop Scand 60(3):319–321
Jonson LL, Uitvlugt G, Austin MD, Detrisac DA, Johnson (1990) Osteochondritis dissecans of the knee: arthroscopic compression screw fixation. Arthroscopy 6:179–189
Jurgensen I, Bachmann G, Schleicher I, Haas H (2002) Arthroscopic versus conservative treatment of osteochondritis dissecans of the knee: value of magnetic resonance imaging in therapy planning and follow-up. Arthroscopy 18(4):378–386
Kivisto R, Pasanen L, Leppilahti, Jalovaara P (2002) Arthroscopic repair of osteochondritis dissecans of the femoral condyles with metal staple fixation: a report of 28 cases. Knee Surg Sports Traumatol Arthrosc 10:305–309
Lindholm TS, Osterman K (1980) Long term results after transfixation of an osteochondritis dissecans fragment to the femoral condyle using autologous bone transplants in adolescent and adult patients. Arch Orthop Trauma Surg 97:225–230
Lipscomb PR Jr, Lipscomb PR Sr, Bryan RS (1978) Osteochondritis dissecans of the knee with loose fragments. Treatment by replacement and fixation with readily removed pins. J Bone Joint Surg 60:235–240
Louisia S, Beaufils P, Katabi M, Robert H (2003) Transchondral drilling for osteochondritis dissecans of the medial condyle of the knee. Knee Surg Sports Traumatol Arthrosc 11(1):33–39
Mackie IG, Pemberton DJ, Maheson M (1990) Arthroscopic use of the Herbert screw in osteochondritis dissecans. J Bone Joint Surg 72(6):1076
Rey Zuniga JJ, Sagastibelza J, Lopez Blasco JJ, Martinez Grande M (1993) Arthroscopic use of the Herbert screw in osteochondritis dissecans of the knee. Arthroscopy 9(6):668–670
Slough J, Noto A, Schmidt T (1989) Tibial cortical bone peg fixation in osteochondritis dissecans of the knee. Clin Orthop 267:122–127
Smillie IS (1957) Treatment of osteochondritis dissecans. J Bone Joint Surg 39(2):248–260
Thomson NL (1987) Osteochondritis dissecans and osteochondral fragments managed by Herbert compression screw fixation. Clin Orthop 224:71–78
Wombwell JH, Nunley JA (1987) Compressive fixation of osteochondritis dissecans fragments with Herbert screws. J Orthop Trauma 1:74–77
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kouzelis, A., Plessas, S., Papadopoulos, A.X. et al. Herbert screw fixation and reverse guided drillings, for treatment of types III and IV osteochondritis dissecans. Knee Surg Sports Traumatol Arthrosc 14, 70–75 (2006). https://doi.org/10.1007/s00167-005-0634-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-005-0634-9