Abstract
Purpose
Magnetic resonance imaging (MRI) has relatively low accuracy in diagnosing chronic anterior talofibular ligament (ATFL) injury. This study’s purpose was to evaluate the angle between the ATFL and posterior talofibular ligament (PTFL) as a new indirect MRI sign of chronic ATFL injury in patients with mechanical ankle instability (MAI).
Methods
This study included 200 participants: 105 patients with MAI and 95 patients seen at our institution for reasons unrelated to ankle instability. MR images of all 200 participants were reviewed. The ATFL–PTFL angle in the axial plane was measured and compared between groups. Receiver operating characteristic curves (ROC) were used to analyze ATFL–PTFL angles in participants with and without ATFL injury. The sensitivity and specificity of this method for diagnosing ATFL injury were calculated.
Results
The mean ATFL–PTFL angle was significantly larger among MAI patients than among control patients (81.5° ± 9.8° vs 75.2° ± 8.9°, respectively; P < 0.01). The area under the ROC was 0.789 (P < 0.01). The optimal cut-off point for diagnosing ATFL injury on the basis of the ATFL–PTFL angle was 79.0° (sensitivity 0.89, specificity 0.67).
Conclusion
The ATFL–PTFL angle was significantly larger among MAI patients than among those without MAI. Increased ATFL–PTFL angle offers a new indirect MRI sign for diagnosing chronic ATFL injury. The ATFL–PTFL angle can be used not only to improve the accuracy of diagnosis of chronic ATFL injury, but also to evaluate the restoration of normal ankle joint geometry after lateral ligament reconstruction.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ankle sprain is one of the most common sports injuries. More than 20% of patients experience chronic symptoms after ankle sprain, including pain, swelling, and giving way or instability [20]. Chronic ankle instability (CAI) can be subdivided into mechanical ankle instability (MAI) and functional ankle instability (FAI) [6]. MAI patients have laxity and excessive motion of the ankle joint caused by structural damage to the supporting ligamentous tissues [6], especially the lateral ligaments. In contrast, the lateral ankle ligaments in FAI patients are normal. The feeling of giving way and instability in FAI patients may be caused by specific insufficiencies in proprioception, neuromuscular control, postural control, and/or muscle strength [6]. In clinical practice, different treatment strategies are used according to type of ankle instability. Therefore, it is very important for clinicians to accurately evaluate the status of the lateral ligaments of the ankle to provide appropriate treatment recommendations.
Magnetic resonance imaging (MRI) is an important tool in assessing the status of the lateral ankle ligaments. Some authors suggested that preoperative MRI of the ATFL is a reliable and valid decisional tool to choose the surgical technique for stabilization of chronic lateral ankle laxity [18]. However, the reported sensitivity and specificity of MRI in diagnosing chronic anterior talofibular ligament (ATFL) and calcaneofibular ligament injures are only 44–75% and 53–86%, respectively. The sensitivity and specificity of MRI in diagnosing partial ligament tears are much lower [4, 8, 12, 22, 26]. Therefore, it is necessary to use indirect MRI signs to improve the diagnostic accuracy. It has been reported that indirect MRI signs can be used in clinical practice to improve the accuracy of diagnosing anterior cruciate ligament (ACL) injury [5, 13, 21, 27]. However, to date, no study has reported the use of indirect MRI signs to assess ATFL injury.
The main purpose of this study was to measure and compare the ATFL–posterior talofibular ligament (PTFL) angles in patients with MAI versus those in control participants without a history of ankle sprain, and to introduce a new indirect MRI sign to assess ATFL injury. We hypothesized that the ATFL–PTFL angle would be greater in MAI patients than in control subjects. Because the accuracy of MRI in the diagnosis of chronic ATFL injury is relatively low, confirmation of the hypothesis would provide a new indirect MRI sign to improve diagnostic accuracy. Moreover, this indirect MRI sign could be used to evaluate the restoration of normal geometry of the ankle joint after lateral ligament reconstruction.
Materials and methods
MRI scans taken from 2012 to 2016 of 105 patients (35 women and 70 men) with MAI (Group A) were retrospectively reviewed. Clinical evaluations were made by the authors on the basis of history, physical examination, and radiographic findings (anteroposterior, lateral, and MRI). Arthroscopic ankle evaluation and debridement were performed in all MAI patients. ATFL tears were identified during ankle arthroscopy. All operations were performed by a senior surgeon specializing in ankle arthroscopy and sports medicine.
The control group consisted of 95 patients (28 women and 67 men) who had undergone MRI at the author’s institution for reasons unrelated to ankle instability (Group B). Chart reviews were undertaken to exclude patients with ligamentous laxity and history of ankle sprain.
The exclusion criteria were as follows: (1) a history of ankle or ipsilateral lower extremity surgery; (2) deformity around the ankle joint such as flat foot, high arch, varus heel, or inverting tibial plateau; (3) previous history of ankle fracture; (4) age less than 16 or older than 60 years; (5) patients with PTFL tear; (6) patients with ATFL tear and the ligament absorbed completely.
MRI scan and image analysis
All MRI scans were performed with a 3.0-T MRI scanner (MAGNETOM Verio, A Tim system, Siemens, Germany) in a standardized fashion. Axial images were taken at PD FSE TR/TE 2600–2800/24–30 ms, matrix 512 × 320, slick thickness 3 mm, at increments from the distal tibial diaphysis to the most inferior aspect of the calcaneus.
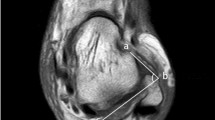
The ATFL–PTFL angle was measured in all participants in the following manner (Fig. 1). The plane in which the ATFL and PTFL appeared simultaneously on the axial image was determined. Two straight lines were drawn, one parallel to the ATFL and one parallel to the PTFL. The angle between these two lines was measured. Because the ATFL and PTFL are oriented in a nearly horizontal plane [24], it was easy to identify these two ligaments in the same axial image [25].
Angle measurements were made with a picture archiving and communication system (PACS version 11.0, Carestream Healthcare, Rochester, NY, USA). The values were accurate to one decimal place. An independent observer who was blinded to the group assignment measured all index values on MRI scans. Each measurement was repeated three times for intraobserver analysis as well as for calculation of mean values. The interval between measurements was at least 1 week to eliminate memory effects. To test interobserver reliability, 30 MRIs from the MAI group were measured independently by two of the authors (the first and the second authors).
This study was approved by the Research Ethics Committee of Huashan Hospital, Fudan University (KY2016-002).
Statistical analysis
All values were reported as means and standard deviations (SD). Intra- and interobserver reliabilities of measurements were analyzed with the intraclass correlation coefficient (ICC). An ICC < 0.4 was considered poor; between 0.4 and 0.7, moderate; and > 0.7, excellent. A reliability analysis of scale was used to calculate the ICC values. Control and laxity patients were compared with an independent t test. Receiver operating characteristic curves (ROC) were used to analyze the ATFL–PTFL angles of participants with versus without ATFL injury. The sensitivity and specificity of this method for diagnosing ATFL injury were calculated. All statistical analyses were performed with SPSS 19.0 (IBM Corporation, Armonk, New York, USA). Differences were considered statistically significant at values of P < 0.05. Post hoc analysis was performed to calculate the statistical power. Because the calculated effect size was 0.9, the sample size was 105 in Group A and 95 in Group B, and the α level was 0.05, the calculated power was 1.0.
Results
Participants’ demographic data are shown in Table 1. No significant differences were found in age, sex, height, weight, or body mass index between the groups.
The intra- and interobserver reliabilities were 0.953 and 0.863, respectively.
The mean angle between the ATFL and PTFL in laxity patients was 81.5° ± 9.8°. The angles varied from 59.4° to 110.1°, a range of 50.7°. The mean ATFL–PTFL angle in the control group was 75.2° ± 8.9°. The angles varied from 54.7° to 103.8°, a range of 49.1°. There was a statistically significant difference in ATFL–PTFL angle between the patient and control groups (P < 0.01).
The area under the ROC was 0.789 (P < 0.01). The optimal cut-off point of the ROC curve in the diagnosis of ATFL injury was an ATFL–PTFL angle 79.0°, which had a sensitivity of 0.89 and a specificity of 0.67.
Discussion
The most important finding of the present study was that the angle between the ATFL and PTFL was significantly larger among MAI patients than among control patients. The ATFL–PTFL angle offers a new indirect MRI sign in the diagnosis of chronic ATFL injury.
CAI can be divided into MAI and FAI, according to different pathological changes. Moreover, different treatment strategies should be chosen for these two types of CAI. Patients with MAI often require ligament reconstruction to restore the laxity of the ankle joint. In contrast, patients with FAI often rely on proprioception, balance, and strength training to restore neuromuscular function [7, 16] and to reduce the risk of ankle re-injury [29]. Accurate assessment of the status of the lateral ankle ligaments is very important when determining treatment strategies. The importance of MRI in evaluating injury of the lateral ankle ligaments has been demonstrated in many studies [9, 10, 17, 19, 23,]. However, recent studies have raised doubts about the accuracy of MRI in these patients [8, 10, 14, 22]. In a meta-analysis, the pooled sensitivity and specificity of MRI in diagnosing chronic ATFL are 0.83 and 0.79, respectively [1]. Moreover, the sensitivity and specificity of MRI are lower in patients with partial versus full ligament tears [12, 22]. One reason for the low accuracy of MRI in the diagnosis of chronic lateral ligament tears is that patients with chronic instability lack joint-space hemorrhage and soft-tissue swelling over the lateral malleolus, making diagnosis more difficult [22]. A second reason is that the sensitivity of MRI for the detection of ATFL tears varies according the location of the ATFL injury [11]. A third reason is that dynamic assessment of joint laxity is not possible with MR scans, which limits the diagnostic accuracy. Previous study indicated that stress ultrasound could increase the diagnostic accuracy of chronic ankle laxity [3]. Moreover, the accuracy of assessing ligament injuries is affected by the experience of the radiologists. Therefore, it is necessary to propose new and easy methods to increase the accuracy of diagnosing chronic lateral ankle ligament injury.
It has been reported that indirect MRI signs can be used to improve the accuracy of ACL injury diagnosis [5, 13, 21, 27]. For example, the angle between the lateral tibial plateau and the ACL is smaller after ACL injury whereas the angle between the Blumenstaat line and the ACL is larger. The presence of indirect signs corroborates the diagnosis of ACL tear [5]. Among the lateral ligamentous structures of the ankle, the ATFL is most often disrupted in ankle sprains and is thus highly important clinically [28]. Therefore, in the current study we proposed a new indirect MRI sign to improve the accuracy of diagnosing ATFL injury. The angle between the ATFL and PTFL was significantly larger among patients with ATFL injury compared with that of the control group, suggesting that this angle may be an indirect MRI sign for diagnosing ATFL injury. Detection and measurement of the angle between the ATFL and PTFL is very simple and reproducible on axial images; therefore, the angle can also be used to evaluate the restoration of the original geometry of the intact joint after lateral ankle ligament reconstruction. Because the ATFL is the most commonly injured ligament in ankle sprain, we believe that evaluation of the ATFL–PTFL angle could be very helpful in clinical practice.
The reasons for the increased size of the ATFL–PTFL angle in patients with MAI are not clear. One potential reason is that the ATFL becomes loose and distorted after injury, resulting in a larger angle between the ATFL and PTFL. Recent studies found that patients with ankle laxity were more likely to have an internally rotated talus [2, 15]; a change in the relative positions of the ATFL and PTFL insertions on the talus, resulting in an increase in the angle between ATFL and PTFL, could also help explain our findings.
Although this study revealed a significant difference in the ATFL–PTFL angle between ankle laxity and control participants, an increased ATFL–PTFL angle was not found in all patients with MAI. The angle between the ATFL and PTFL was less than 79° in one-third of patients with unilateral ankle laxity and was more than 79° in one-third of participants in the control group. Therefore, an increased ATFL–PTFL angle may be present in some, but not in all patients with MAI. Additionally, there was wide variability in the ATFL–PTFL angle (ranges of 50.7° and 49.1° in ankle laxity and control groups, respectively). Therefore, the ATFL–PTFL angle cannot be used as the gold standard to diagnose ATFL injury. The diagnosis of ATFL injury in MAI patients should be based on patient history, clinical examination, and imaging. Further studies are needed to address the relationship between these abnormal changes and MAI.
The advantage of the current study was its large sample size.
One limitation of this study was that participants in the control group might not be representative of the normal healthy population. However, patients with ankle instability were excluded from the control group. A prospective study will be required to compare the differences between CAI patients and the normal healthy population in the future. A second limitation was that the MRI scans were obtained in a supine, non-weight-bearing position. Because the angle between the ATFL and PTFL may be different in weight-bearing versus non-weight-bearing positions, the values of the ATFL–PTFL angle could be altered. However, all participants in the current study were scanned in the same supine position; therefore, we believe that the results of the measurements were comparable between the two groups. An MRI study in weight-bearing ankles may be needed in the future.
In previous studies, the accuracy of MRI for diagnosing chronic ATFL injury was relatively low, especially for the diagnosis of partial injury. Therefore, new indirect MRI signs are needed to improve diagnostic accuracy. In the current study, a new, simple, and reproducible indirect MRI sign was introduced to evaluate the angle between the ATFL and PTFL. The ATFL–PTFL angle could be used to evaluate ATFL injury in a clinical setting. An increased ATFL–PTFL angle may be an indirect MRI sign of ATFL injury. Moreover, the ATFL–PTFL angle could be used to evaluate the restoration of normal ankle joint geometry after lateral ligament reconstruction.
Conclusion
Patients with ankle laxity were more likely to have a larger ATFL–PTFL angle than patients without ankle laxity. The angle between the ATFL and PTFL offers a new indirect MRI sign for diagnosing ATFL injury. A larger angle between the ATFL and PTFL was associated with a diagnosis of ATFL tear.
References
Cao S, Wang C, Ma X, Wang X, Huang J, Zhang C (2018) Imaging diagnosis for chronic lateral ankle ligament injury: a systemic review with meta-analysis. J Orthop Surg Res 2018; 13:122
Caputo AM, Lee JY, Spritzer CE, Easley ME, DeOrio JK, Nunley JA IInd, DeFrate LE (2009) In vivo kinematics of the tibiotalar joint after lateral ankle instability. Am J Sports Med 37:2241–2248
Cho JH, Lee DH, Song HK, Bang JY, Lee KT, Park YU (2016) Value of stress ultrasound for the diagnosis of chronic ankle instability compared to manual anterior drawer test, stress radiography, magnetic resonance imaging, and arthroscopy. Knee Surg Sports Traumatol Arthrosc 24:1022–1028
Elkaïm M, Thès A, Lopes R, Andrieu M, Cordier G, Molinier F, Benoist J, Colin F, Boniface O, Guillo S, Bauer T; French Arthroscopy Society (2018) Agreement between arthroscopic and imaging study findings in chronic anterior talo-fibular ligament injuries. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2018.09.008
Gentili A, Seeger LL, Yao L, Do HM (1994) Anterior cruciate ligament tear: indirect signs at MR imaging. Radiology 193:835–840
Hertel J (2002) Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train 37:364–375
Holmes A, Delahunt E (2009) Treatment of common deficits associated with chronic ankle instability. Sports Med 39:207–224
Jolman S, Robbins J, Lewis L, Wilkes M, Ryan P (2017) Comparison of magnetic resonance imaging and stress radiographs in the evaluation of chronic lateral ankle instability. Foot Ankle Int 38:397–404
Jung HG, Kim NR, Kim TH, Eom JS, Lee DO (2017) Magnetic resonance imaging and stress radiography in chronic lateral ankle instability. Foot Ankle Int 38:621–626
Kanamoto T, Shiozaki Y, Tanaka Y, Yonetani Y, Horibe S (2014) The use of MRI in pre-operative evaluation of anterior talofibular ligament in chronic ankle instability. Bone Jt Res 3:241–245
Kim YS, Kim YB, Kim TG, Lee SW, Park SH, Lee HJ, Choi YJ, Koh YG (2015) Reliability and validity of magnetic resonance imaging for the evaluation of the anterior talofibular ligament in patients undergoing ankle arthroscopy. Arthroscopy 31:1540–1547
Kumar V, Triantafyllopoulos I, Panagopoulos A, Fitzgerald S, van Niekerk L (2007) Deficiencies of MRI in the diagnosis of chronic symptomatic lateral ankle ligament injuries. Foot Ankle Surg 13:171–176
Lefevre N, Naouri JF, Bohu Y, Klouche S, Herman S (2014) Sensitivity and specificity of bell-hammer tear as an indirect sign of partial anterior cruciate ligament rupture on magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc 22:1112–1118
Lee MH, Cha JG, Lee YK, Choi GC, Paik SH, Lee HK, Park SJ, Kim HJ (2012) The bright rim sign on MRI for anterior talofibular ligament injury with arthroscopic correlation. AJR Am J Roentgenol 198:885–890
Li HY, Zhou RS, Hua YH, Chen SY (2017) MRI identification of the fibular and talus position in patients with mechanical ankle instability. Int J Sports Med 38:546–550
McKeon PO, Hertel J (2008) Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athl Train 43:305–315
Miller JR, Dunn KW, Ciliberti LJ Jr, Eldridge SW, Reed LD (2017) Diagnostic value of early magnetic resonance imaging after acute lateral ankle injury. J Foot Ankle Surg 56:1143–1146
Morvan A, Klouche S, Thes A, Hardy P, Bauer T (2018) Reliability and validity of preoperative MRI for surgical decision making in chronic lateral ankle instability. Eur J Orthop Surg Traumatol 28:713–719
Oae K, Takao M, Uchio Y, Ochi M (2010) Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skelet Radiol 39:41–47
O’Loughlin PF, Murawski CD, Egan C, Kennedy JG (2009) Ankle instability in sports. Phys Sportsmed 37:93–103
Palle L, Reddy B, Reddy J (2010) Sensitivity and specificity of vertically oriented lateral collateral ligament as an indirect sign of anterior cruciate ligament tear on magnetic resonance imaging. Skelet Radiol 39:1123–1127
Park HJ, Cha SD, Kim SS, Rho MH, Kwag HJ, Park NH, Lee SY (2012) Accuracy of MRI findings in chronic lateral ankle ligament injury: comparison with surgical findings. Clin Radiol 67:313–318
Perrich KD, Goodwin DW, Hecht PJ, Cheung Y (2009) Ankle ligaments on MRI: appearance of normal and injured ligaments. AJR Am J Roentgenol 193:687–695
Raheem OA, O’Brien M (2011) Anatomical review of the lateral collateral ligaments of the ankle: a cadaveric study. Anat Sci Int 86:189–193
Schneck CD, Mesgarzadeh M, Bonakdarpour A, Ross GJ (1992) MR imaging of the most commonly injured ankle ligaments. Part I. Normal anatomy. Radiology 184:499–506
Tan DW, Teh DJW, Chee YH (2016) Accuracy of magnetic resonance imaging in diagnosing lateral ankle ligament injuries: a comparative study with surgical findings and timings of scans. Asia Pac J Sports Med Arthrosc Rehabil Technol 7:15–20
Vassalou EE, Klontzas ME, Kouvidis GK, Matalliotaki PI, Karantanas AH (2016) Rotational knee laxity in anterior cruciate ligament deficiency: an additional secondary sign on MRI. AJR Am J Roentgenol 206:151–154
Verhagen RA, de Keizer G, van Dijk CN (1995) Long-term follow-up of inversion trauma of the ankle. Arch Orthop Trauma Surg 114:92–96
Witchalls J, Blanch P, Waddington G, Adams R (2012) Intrinsic functional deficits associated with increased risk of ankle injuries: a systematic review with meta-analysis. Br J Sports Med 46:515–523
Acknowledgements
This work was supported by a grant awarded to Ying-Hui Hua from the National Natural Science Foundation of China (NSFC81572209).
Funding
This study was funded by National Natural Science Foundation of China (NSFC81572209).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflict of interest.
Ethical approval
This study was approved by the Research Ethics Committee of Huashan Hospital, Fudan University (KY2016-002).
Rights and permissions
About this article
Cite this article
Li, HY., Li, WL., Chen, SY. et al. Increased ATFL–PTFL angle could be an indirect MRI sign in diagnosis of chronic ATFL injury. Knee Surg Sports Traumatol Arthrosc 28, 208–212 (2020). https://doi.org/10.1007/s00167-018-5252-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5252-4