Abstract
Purpose
To diagnose chronic anterior talofibular ligament (ATFL) injury, three different physical examinations were compared: the anterior drawer test (ADT), the anterolateral drawer test (ALDT), and the reverse anterolateral drawer test (RALDT).
Methods
A total of 72 ankles from potential ATFL-injured patients and the normal population were included and examined using the ADT, ALDT, and RALDT by two examiners without knowing the injury histories of any of the participants. Ultrasound examination was then applied as the gold standard to divide the ankles into the ATFL-injured group and the control group. The sensitivity (Se), specificity (Sp), false negative rate (FNR), false positive rate (FPR), accuracy, κ value, and p value of the two examiners’ diagnoses were calculated to assess the diagnostic ability of each examination.
Results
There were 38 ankles in the injured group and 34 ankles in the control group. No significant difference was found between the two groups in terms of gender, age, body mass index (BMI), and included ankles. In the ADT and ALDT groups, the specificity reached one, while the sensitivity was relatively low (0.053 and 0.477 for the junior examiner and 0.395 and 0.500 for the senior examiner). In the RALDT, both the sensitivity and specificity were greater than 85% (0.868 and 0.912 for the senior examiner and 0.921 and 0.882 for the junior examiner). The κ value of the RALDT (0.639) was higher than that of the ALDT (0.528) and the ADT (0.196), whereas all the p values were less than 0.05.
Conclusion
The ADT and ALDT are valuable physical tests to assess ATFL injuries. Compared with the traditional ADT and ALDT, however, the RALDT is more sensitive and accurate in diagnosing chronic ATFL injuries.
Level of evidence
II (diagnostic).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral ankle sprain (LAS) is one of the most common musculoskeletal injuries, with a high prevalence among the general population and particularly among individuals who participate in sports and recreational physical activities [14, 15]. It has been reported that as many as 70% of the general population indicate having incurred an ankle injury during their lifetime [16]. The long-term prognosis of acute ankle sprain is still not optimistic, since a high proportion of patients (up to 70%) report having persistent residual symptoms, including pain, persistent swelling, feelings of ankle joint instability or ‘giving-way’ [1, 15]. ‘Chronic ankle instability (CAI)’ is the term used to describe these chronic symptoms, which have been shown to persist for more than 12 months and, in turn, may cause an inability to participate in work and sports and incur a high economic burden [30].
The anterior talofibular ligament (ATFL) is most likely involved in ankle sprains with an 80% prevalence [3]. Therefore, it is important to accurately and efficiently diagnose ATFL injuries. The traditional physical examination test is the anterior drawer test (ADT), which provides an anterior–posterior vector that exerts stress to both the lateral and medial ligaments [31]. In the ADT, when the ATFL is injured, the medial deltoid ligament can remain intact, which can lead to false negative results. Lahde et al. reported that 28% of ATFL tears and 38% of combined ATFL and calcaneofibular ligament (CFL) tears were not detected by the ADT [18]. Since 2006, the anterolateral drawer test (ALDT), a new physical examination with higher accuracy, has been modified and applied to diagnose ATFL injuries with or without CFL injuries [23]. However, the differences between the traditional ADT and ALDT were only 10°–15° of plantar flexion (which puts the ATFL in a tightened state) and palpation at the surface of the lateral ligament (which makes it easy to feel the displacement of the talus). Some techniques, such as unconstrained internal rotation of the forefoot (which puts the ATFL in a tightened state and relaxes the medial ligaments at the same time), could be applied for diagnosing ATFL injuries to maximize the accuracy of the ALDT [22].
Nevertheless, during the examination, the two hands manipulating the ankle, whether stabilizing the distal tibia or measuring the displacement of the talus, are unfixed. This means that the sensation of relative hand movements on the ankle generated during the examination is inevitable. Both the ADT and ALDT are based on the perception of the talus displacement, which is likely to be disturbed when the sensation of relative hand movements and the displacement of the talus (the positive result of the examination) occur simultaneously. Given the psychological fact that the perception of a stimulus is strongly influenced by the context in which the stimulus appears, i.e., the contextual effect [21], a new method that significantly decreases the sensation of relative hand movements is expected to be designed for diagnosing ATFL injuries. Thus, supplemented with more technical requirements, the ALDT was modified and named the ‘Reverse Anterolateral Drawer Test (RALDT)’ to optimize the examination, avoid the contextual effects introduced by the clinician’s hands, and provide a more sensitive and accurate measurement for diagnosing chronic ATFL injuries.
Hence, the goal of the current study was to prospectively determine the diagnostic abilities of the ADT, ALDT, and RALDT and compare them with each other.
The hypothesis of this study is that the RALDT has better diagnostic ability than the ADT and ALDT in indicating chronic ATFL injuries.
Materials and methods
This was a prospective and double-blind diagnostic trial. Patients who sought care at the Sports Medicine outpatient clinic of our hospital during the period of January 2018–June 2018 were assessed in terms of the inclusion and exclusion criteria for this study. After the assessment, 36 participants who were suspected of having ATFL injury were included in this study. The inclusion criteria were: (1) participants who were younger than 60 years; (2) participants who were conscious and willing to cooperate with the physical examination; (3) participants who had a history of inversion ankle sprains in one or both feet; (4) participants whose ATFL injuries had occurred at least 1 week prior to the study—pain and swelling in the acute phase could decrease the accuracy of the physical examinations, and a delayed physical examination could help to improve the sensitivity and specificity of the test [29]; and (5) participants were conscious and willing to take part in the trail. Patients were excluded if they had a history of distal tibiofibular syndesmosis injuries, deltoid ligament injuries, lower limb fractures, previous ATFL surgeries, Achilles tendon injuries or had broken skin around the ankle region that could limit the accuracy of the ultrasound examination.
After signing the consent form to accept both the physical and ultrasound examinations at the outpatient clinic of the corresponding author, the participants were randomly brought to the physical examination room by the first author. Then, a junior and a senior examiner came into the room to examine the two ankles of the included participants and recorded the outcomes of the ADT, ALDT, and RALDT one after another. The two examiners were blinded to any information about the participants. Next, the participants were brought to the ultrasound examination room to receive ultrasonography. The sonographer had no knowledge of the participants’ clinical history or the results of the physical examinations. The procedure is shown in Fig. 1.
Anterior drawer test
The test was performed in a seated position with the calf hanging over the edge of the examination bed. The examiner stabilized the distal tibia of the participant with one hand and applied an anteriorly orientated force to the calcaneus with the other hand (Fig. 2a), which is consistent with the technique as described by van Dijk et al. [28]. The examiner graded the amount of talus anterior–posterior displacement according to a 0-to-4 ordinal scale, with a grade of 0 as hypomobile, 1 as normal, 2 as mildly increased laxity, 3 as moderately increased laxity, and 4 as severely increased laxity. Grades 3 and above were considered ‘positive’ for excessive laxity, whereas grades 0, 1, and 2 were considered ‘negative’ or normal [7].
Three physical examinations were shown in the figure. The ADT was demonstrated in (a) and the ALDT and RALDT were demonstrated in (b) and (c), respectively. The red arrows showed the directions of the forces exerted by hands. ADT anterior drawer test, ALDT anterolateral drawer test, RALDT reverse anterolateral drawer test
Anterolateral drawer test
The test was performed in a seated position with the calf hanging over the edge of the examination bed. The examiner stabilized the distal tibia with one hand and provided a combination of an anteriorly orientated force, measurement of talus displacement, and control of ankle plantarflexion simultaneously with the other hand, as described by Phisitkul et al. [23]. More specifically, the index and middle fingers pressed firmly against the posterior aspect of the heel to provide the anteriorly directed force. The palm supported the sole of the foot to maintain a 10°–15° plantar flexion and tighten the lateral ligaments. The thumb was placed along the relatively smooth plane of the lateral aspect of the anterior talar dome and the anterior aspect of the lateral malleolus 1 cm proximal to its tip. The grading standard was the same as that of the ADT (Fig. 2b).
Reverse anterolateral drawer test
The examination was performed, while the patient was lying in the bed with the knee flexed and the angle of the knee adjusted to facilitate plantar flexion. The heel was completely pressed on the bed by the examiner with one hand after adjusting the ankle to a 10°–15° degree plantar flexion and unconstrained internal rotation. The index and middle fingers were placed along the relatively smooth plane of the lateral aspect of the anterior talar dome and the anterior aspect of the lateral malleolus 1 cm proximal to its tip. The other hand held the distal tibia, and the base of the palm pushed against the tibia to induce a posteriorly oriented displacement of the tibia with a force parallel with that of the articular surface arch of the talus. The grading standard was similar to that of the ADT (Fig. 1c).
Ultrasound examination
The outcomes of the ultrasound examination were regarded as the reference standards due to its high sensitivity and specificity (0.99 [0.96, 1.00] and 0.91 [0.82, 0.97], respectively) [5]. All ultrasound examinations were performed by a senior sonographer who had 33 years of experience in musculoskeletal ultrasound. An ALT HDI 5000 US unit (Philips Medical Systems, Bothell, WA, USA) was used to perform these examinations. Patients were in a supine position with the ankle passively placed in a maximal inversion and plantar flexion position. A wide frequency linear array transducer with centre frequencies from 5 to 17 MHz was applied. The transducer was placed over the lateral side of the ankle with coupling gel and moved carefully around the tip of the lateral malleolus to locate the ATFL. The transducer was placed along the long axis of the ATFL to examine the whole ligament and then rotated 90° to show the short axis of the ATFL. The criteria for ATFL injury were as follows: (1) ligament tear: a partial or total interruption of the ligament fibres at the fibular side, talus side or in the middle; (2) lax ligament: the ligament remained curved when the ankle was in the maximum inversion and plantar flexion position; (3) thickened ligament: the width of the ligament was larger than 2.4 mm or exceeded 20% of the normal ligament width; (4) ligament absorbed: no ligament fibres were observed; and (5) non-union of the avulsion fracture of the lateral malleolus [17] (Fig. 3).
Examples of the normal and injured ATFL. a Sonogram showed a normal longitudinal ATFL of the left foot. b Sonogram showed a normal longitudinal ATFL of the right foot. c Sonogram showed a normal transversal ATFL of the left foot and the cross indicated the edge of the ATFL. d Sonogram showed a total tear of the ATFL at the fibula side and the white arrow indicated the fluid. e Sonogram showed a hyperechoic shadow (surrounded by the white cross) in the remanent ligament at the fibular side. F fibula, T talus, ATFL anterior talofibular ligament, AB avulsion bone
This study was approved by the institutional review board of Huashan Hospital (Reference Number: KY2106-314).
Statistical analysis
The sample size was calculated with a desired type I error of 0.05 and a power of 0.9: and the minimal sample size was 28 [6]. Data analysis was performed using SPSS 24.0 software (IBM Corp, Armonk, New York, USA). Age and body mass index (BMI) were expressed as the mean ± SD, because they were found to be normally distributed via the Lilliefors test and were assessed with a t test. The gender and number of included ankles were assessed with Fisher’s exact test. The sensitivity (Se), specificity (Sp), false negative rate (FNR), false positive rate (FPR), accuracy, positive likelihood ratio (LR+), and negative likelihood ratio (LR−) of each examination collected by the two examiners were calculated. The κ values and their p values, indicating the consistency of the two examiners, were also calculated to reflect the diagnostic ability of each examination.
Results
Patient demographics
The groups were divided according to the results of the ultrasound examination. There were 38 ankles (20 left and 18 right) from 31 participants (18 male and 13 female) with a median age of 30.4 ± 8.9 years and a BMI of 22.6 ± 3.7 kg/m2 in the injured group and 34 ankles (15 left and 19 right) from 29 participants (15 male and 14 female) with a median age of 29.1 ± 8.9 years and BMI of 22.5 ± 3.7 kg/m2 in the control group (Table 1). Thus, the sample size in the current study was larger than 28 and verifiable for the subsequent statistical test. There was no significant difference between the two groups in terms of gender, age, BMI, and included ankles.
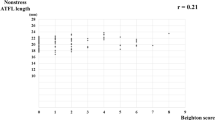
Comparisons of the diagnostic ability for the three examinations
The results of the three examinations collected from all participants are shown in Table 2. The specificities of the ADT and ALDT were high, while the sensitivities were relatively low (respectively, 0.053 and 0.447 for the junior examiner and 0.395 and 0.500 for the senior examiner). Both the sensitivity and specificity of the RALDT were higher than 85% (respectively, 0.868 and 0.912 for the junior examiner and 0.921 and 0.882 for the senior examiner). The κ value of the RALDT (0.639) was higher than that of the ALDT (0.528) and ADT (0.196); meanwhile, the p values reflecting the consistencies of the two examiners were all less than 0.05.
Discussion
The most important finding of this study is that the sensitivity and accuracy of the RALDT calculated based on the two examiners’ physical examination results were higher than those of the ALDT and ADT. Although the specificity in the ADT and ALDT were higher than those in the RALDT, rationally, the specificity is supposed to be chosen to balance a relatively high sensitivity. Thus, the RALDT, with both a relatively high specificity and sensitivity, showed a greater ability to diagnose chronic ATFL injuries. Meanwhile, the RALDT had the highest κ value of the three examinations, revealing that the RALDT was most consistent with the results of the ultrasound or, in other words, the real outcomes. As a traditional physical examination, the ADT has been applied to diagnose CAI for decades [12, 24, 26]; however, its reliability and validity have often been doubted. During the traditional ADT process, the foot is placed in a neutral position, which is likely to cause a false negative result if the deltoid ligament is intact [23]. Phisitkul et al. found that after adding 10°–15°of plantar flexion and palpation at the surface of the lateral ligament to the ADT, the resulting examination, the ALDT, showed higher accuracy. Gomes et al. also verified that palpation of the anterolateral talus increases sensitivity [9], which allows the detection of more subtle degrees of ankle instability. The findings in this study also showed that the ALDT was more sensitive and accurate than the traditional ADT.
Nevertheless, as mentioned above, the additional techniques described for the ADT and the ALDT focus on how to control subjective elements that may interfere with the accuracy of the examination. However, the drawer test is ultimately a relatively objective examination. Therefore, psychological factors should also be taken into consideration. When context effects occur, the perception of a stimulus is compared with that of a reference stimulus when they occur simultaneously [4]. This means that the examiners use environmental cues (the sensation of relative hand movements generated during the examination) perceived while feeling the stimuli (the displacement of the talus) to help with analysing the outcomes [13, 19]. If the stimulus is perceived to have a high intensity, the actual strength of the stimulus is underestimated and vice versa [11]. That is, in both the ADT and ALDT, the sensation of relative hand movements would inevitably decrease the perception of positive signs and cause false negative results, which may explain the low sensitivities of the ADT and ALDT. In addition, kinesthesis had a close relationship with visual sensations [8, 27], which means that the sensation of relative hand movements caused by unfixed hands would influence judgement of the tactile sensations. Even if the ankle is stabilized and both the medial and lateral ligaments are intact, the relative hand movements could still make the eyes ‘see’ a positive sign. This might be an underlying cause of the low accuracy of the ADT and ALDT. Fortunately, these biases were avoided in the RALDT, with the heel of the foot being fixed on the bed with one hand. In this situation, the examiner’s hand is fixed to the foot and to the bed, largely decreasing sensations of relative hand movements as well as biases caused by incorrect perception due to visualizing the relative hand movements. The existence of psychological factors in the drawer tests might be proven in this study. The main difference between the RALDT and the ADT ALDT was the movement range of hand. When the RALDT was applied, the examiner was less likely to perceive and see inaccurate information.
The unconstrained internal rotation state of the foot puts the ATFL in a tightened state, and the deltoid ligament relaxes at the same time [2, 20, 25]. Moreover, Miller et al. stated that unconstrained internal rotation of the foot could provoke almost twice as much lateral talus displacement using a measuring instrument [22]. This step was also added to the RALDT, which might also explain why the RALDT was the most sensitive and accurate test of the three physical examinations.
Keeping the ankle in a plantar flexion of 10°–15°and putting the thumb on the ATFL could have improved the sensitivity and accuracy of the ALDT and RALDT over those of the ADT. Furthermore, adding another essential technique (the internal rotation of the forefoot) and reducing the psychological bias could have also improved the sensitivity of the RALDT over those of the ADT and ALDT. Both the accuracies and the κ values of the three examinations from the two examiners also indicated this tendency.
Another important finding of this study was that the sensitivity of the first examiner, the junior doctor, was lower than that of the second examiner, the senior doctor. Meanwhile, the accuracy of the junior examiner was higher than that of the senior examiner. The results were consistent with those of Fujii, who found that the determination of ankle instability from physical examinations lacked sensitivity and would be difficult in less experienced hands [10]. It is possible that the junior doctor tended to diagnose more conservatively, especially as he was oblivious of any information about the history of the participants. With the accumulation of working experience, the examiner will eventually become more decisive and accurate.
There were several limitations to this study. First, the results of only two examiners were analysed. Given that the judgements for physical examinations vary from person to person, more examiners should be employed in further studies. Second, the ultrasonography was used as the ‘gold standard’ instead of operative findings, because ultrasound examination is inexpensive, requiring only operator time and no radiation, while performing arthroscopic surgery on every included participant would have been unethical, since nearly half of the ankles were clinically intact. Finally, although the sample size in this study met statistical standards, it was still not large enough for stable outcomes in the whole population.
The study compared three similar manual examinations in diagnosing chronic ATFL injury and provided a more objective reference for clinical workers when choosing ankle examinations. The results suggest applying RALDT as a first option or as an important supplement in the clinicians’ daily duties. More high-quality studies are required to verify these results.
Conclusion
The ADT and ALDT are valuable means to assess ATFL injuries and have been in use for decades. The accuracy of these two tests can be improved by amending the main parts of the technique, resulting in the RALDT. Compared with the traditional ADT and the modified ALDT, the RALDT showed greater ability to diagnose chronic ATFL injuries.
References
Anandacoomarasamy A, Barnsley L (2005) Long term outcomes of inversion ankle injuries. Br J Sports Med 39:e14 (discussion e14)
Boruta PM, Bishop JO, Braly WG, Tullos HS (1990) Acute lateral ankle ligament injuries: a literature review. Foot Ankle 11:107–113
Brostrom L (1966) Sprained ankles. V. Treatment and prognosis in recent ligament ruptures. Acta Chir Scand 132:537–550
Brozek J (1966) Fechner G-elements of Psychophtsics. Am Sci 54:A359
Cao S, Wang C, Ma X, Wang X, Huang J, Zhang C (2018) Imaging diagnosis for chronic lateral ankle ligament injury: a systemic review with meta-analysis. J Orthop Surg Res 13:122
Chow S-C, Wang H, Shao J (2007) Sample size calculations in clinical research. CRC Press, Boca Raton
Croy T, Koppenhaver S, Saliba S, Hertel J (2013) Anterior talocrural joint laxity: diagnostic accuracy of the anterior drawer test of the ankle. J Orthop Sports Phys Ther 43:911–919
Dieter KC, Hu B, Knill DC, Blake R, Tadin D (2014) Kinesthesis can make an invisible hand visible. Psychol Sci 25:66–75
Fujii T, Luo ZP, Kitaoka HB, An KN (2000) The manual stress test may not be sufficient to differentiate ankle ligament injuries. Clin Biomech (Bristol, Avon) 15:619–623
Gescheider GA, Thorpe JM, Goodarz J, Bolanowski SJ (1997) The effects of skin temperature on the detection and discrimination of tactile stimulation. Somatosens Mot Res 14:181–188
Glasgow M, Jackson A, Jamieson AM (1980) Instability of the ankle after injury to the lateral ligament. J Bone Joint Surg Br 62-b:196–200
Goldreich D, Peterson MA (2012) A Bayesian observer replicates convexity context effects in figure-ground perception. Seeing Perceiving 25:365–395
Gomes JLE, Soares AF, Bastiani CE, de Castro JV (2018) Anterolateral talar palpation: a complementary test for ankle instability. Foot Ankle Surg 24:486–489
Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT et al (2016) 2016 consensus statement of the International Ankle Consortium: prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med 50:1493–1495
Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT et al (2016) Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med 50:1496–1505
Hiller CE, Nightingale EJ, Raymond J, Kilbreath SL, Burns J, Black DA et al (2012) Prevalence and impact of chronic musculoskeletal ankle disorders in the community. Arch Phys Med Rehabil 93:1801–1807
Hua Y, Yang Y, Chen S, Cai Y (2012) Ultrasound examination for the diagnosis of chronic anterior talofibular ligament injury. Acta Radiol 53:1142–1145
Lahde S, Putkonen M, Puranen J, Raatikainen T (1988) Examination of the sprained ankle: anterior drawer test or arthrography? Eur J Radiol 8:255–257
Lloyd K, Leslie DS (2013) Context-dependent decision-making: a simple Bayesian model. J R Soc Interface 10:20130069
Marder RA (1995) Current methods for the evaluation of ankle ligament injuries. Instr Course Lect 44:349–357
Meyers-Levy J, Zhu R, Jiang L (2010) Context effects from bodily sensations: examining bodily sensations induced by flooring and the moderating role of product viewing distance. J Consum Res 37:1–14
Miller AG, Myers SH, Parks BG, Guyton GP (2016) Anterolateral drawer versus anterior drawer test for ankle instability: a biomechanical model. Foot Ankle Int 37:407–410
Phisitkul P, Chaichankul C, Sripongsai R, Prasitdamrong I, Tengtrakulcharoen P, Suarchawaratana S (2009) Accuracy of anterolateral drawer test in lateral ankle instability: a cadaveric study. Foot Ankle Int 30:690–695
Rasmussen O (1985) Stability of the ankle joint. Analysis of the function and traumatology of the ankle ligaments. Acta Orthop Scand Suppl 211:1–75
Santilli V, Frascarelli MA, Paoloni M, Frascarelli F, Camerota F, De Natale L et al (2005) Peroneus longus muscle activation pattern during gait cycle in athletes affected by functional ankle instability: a surface electromyographic study. Am J Sports Med 33:1183–1187
Seligson D, Gassman J, Pope M (1980) Ankle instability: evaluation of the lateral ligaments. Am J Sports Med 8:39–42
Treisman M, Lages M (2010) Sensory integration across modalities: how kinaesthesia integrates with vision in visual orientation discrimination. Seeing and Perceiving 23:435–462
van Dijk CN, Mol BW, Lim LS, Marti RK, Bossuyt PM (1996) Diagnosis of ligament rupture of the ankle joint. Physical examination, arthrography, stress radiography and sonography compared in 160 patients after inversion trauma. Acta Orthop Scand 67:566–570
van Dijk CN, Lim LSL, Bossuyt PMM, Marti RK (1996) Physical examination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg 78B:958–962
Vuurberg G, Hoorntje A, Wink LM, van der Doelen BFW, van den Bekerom MP, Dekker R et al (2018) Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med 52:956
Watanabe K, Kitaoka HB, Berglund LJ, Zhao KD, Kaufman KR, An KN (2012) The role of ankle ligaments and articular geometry in stabilizing the ankle. Clin Biomech (Bristol, Avon) 27:189–195
Funding
This work was funded by the National Science Foundation of China (Nos. 81572209).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the review board of Fudan University (Reference Number: KY2106-314).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, Q., Tu, Y., Chen, J. et al. Reverse anterolateral drawer test is more sensitive and accurate for diagnosing chronic anterior talofibular ligament injury. Knee Surg Sports Traumatol Arthrosc 28, 55–62 (2020). https://doi.org/10.1007/s00167-019-05705-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05705-x