Abstract
Purpose
The main purpose of this study was to evaluate the usefulness of the bell-hammer sign in the diagnosis of partial tears of the anterior cruciate ligament (ACL) of the knee on MRI.
Methods
A retrospective study was performed including all patients who underwent ACL reconstruction for partial or complete tears from 2008 to 2009. The diagnosis of partial or complete ACL tears was based on the appearance of the ligament bundles and the signal quality on MRI. On arthroscopy, which is considered the gold standard, each bundle was classified as normal, partially or completely torn depending on the extent of the rupture and the quality of the remaining fibres. The study included 312 patients, 83 women and 229 men (mean age 33.3 ± 19.6 years). A diagnosis of a tear was made in all patients on preoperative MRI. Arthroscopy did not show any normal ACL, 247/312 (79.2 %) complete tears and 65/312 (20.8 %) partial tears, 50/65 (76.9 %) on the anteromedial bundle (AM) and 15/65 (23.1 %) the posterolateral bundle.
Results
The bell-hammer sign was found on MRI in 13/312 patients (4.5 %). It involved 9/65 (13.8 %) partial tears, all in the AM bundle, and 4/247 (1.6 %) complete tears, significantly more frequent in cases of partial rupture (p < 0.0001). MRI diagnosed a partial tear in 15/65 cases without the bell-hammer sign (sensitivity CI95 % = 23.1 ± 10 %, specificity CI95 % = 95.9 ± 2.5 %) and with the bell-hammer sign in 23/65 cases (sensitivity CI95 % = 35.4 ± 11 %, specificity CI95 % = 93.9 ± 3 %). The association of the bell-hammer sign with conventional radiological diagnostic criteria has improved diagnosis performance of MRI for partial tears but not significantly (ns).
Conclusion
The most important interest of the bell-hammer sign in the day-to-day clinical work is to suggest partial tears on MRI. It aids making a diagnosis, but its absence does not exclude partial ACL rupture.
Level of evidence
Diagnostic study, Level II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An anterior cruciate ligament (ACL) bell-hammer tear, also known as the preoperative cyclops syndrome, has rarely been described in the literature [12, 20]. It is a ligament injury of the distal stump of the ACL in which a retracted bell hammer may be interposed between the femur and tibia. Histological evaluation of the resected nodules has showed distorted ACL fibres intermixed with variable fibrosis, inflammation and dark brown haemorrhagic areas [16, 20]. It involves an estimated 3 % of ACL tears [20] and often results in a loss of knee extension that may be mistakenly attributed to pain, post-traumatic joint effusion or the presence of meniscal fragments. According to some authors, this lesion is usually found in partial tears [1, 12].
The diagnosis of partial tears is difficult and is based on a series of tests [4]: an asymmetric Lachman test compared to the healthy knee, a negative pivot-shift test, laxity >3 mm with KT-1000 and ACL injury on arthroscopy. While MRI has a sensitivity of 92–96 % and a specificity of 92–98 % in the diagnosis of complete tears [19], its accuracy in diagnosing partial tears remains low [10, 21]. Normally, MRI can suggest a diagnosis of partial tear, but a definitive diagnosis is not possible [4, 22]. The main diagnostic criteria for a partial ACL tear on MRI are a hyperintense intraligamentary signal, sinuous path and/or localized thinning but continuous and well-oriented fibres [6, 24] on sagittal views, confirmed on coronal, axial and oblique views. Palle et al. [14] reported that the vertically oriented lateral collateral ligament is a useful indirect MRI sign of ACL tear in equivocal cases.
The aim of this study was to evaluate the diagnostic value of the bell-hammer sign on MRI in partial tears of the ACL compared to arthroscopy which was the gold standard. The study hypothesis was that the addition of this sign to other commonly used signs in MRI would improve the accuracy of this examination in the diagnosis of partial tears.
Materials and methods
A retrospective study was performed including all patients who underwent ACL reconstruction for partial or complete tears from 2008 to 2009. The clinical and arthroscopic data were collected prospectively.
Description of the bell-hammer tear
On MRI
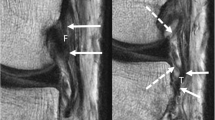
Previously described by Huang et al. [7] and Runyan et al. [16], the bell hammer is bundle of tissue 1 and 2 cm in diameter that is usually pedunculated but may be sessile. It is found in the anterior part of the intercondylar notch in front of the ACL and extends into the anterior femorotibial space (Fig. 1). The proximal end, which is often swollen and club shaped, may tilt anteriorly and laterally when it is pedicled and then hang over the insertion of the anterior horn of the lateral meniscus. The MRI signal varies, but it is often a heterogeneous intermediate signal on T2-weighted images and relatively hyperintense on T1.
Bell hammer on T2-weighted MRI of the knee after partial tear of ACL; 3D volume acquisition and reconstruction. a Sagittal T2: discontinuity of the anteromedial bundle. At the distal portion (blue arrow), the ligament stump is inclined forward and has an intermediate signal; b Axial oblique T2 in the axis of the distal portion of retracted ligament: the cyclops formation has a heterogeneous and intermediate signal in the anterior femorotibial space; c Coronal T2: the cyclops formation has an intermediate signal on the median line, separate of adjacent Hoffa’s fat; d Coronal oblique T2 in the axis of the posterior fibres of ACL: presence of ligament fibres (green arrow) with signal slightly increased, but an overall continuity of the posterolateral bundle
On CT arthrography
This is not an examination of routine, but it is sometimes realized in case of a sprained knee with irreducible flexion. The bell hammer is in the form of an oblong image in sagittal section or ovoid in coronal section (Fig. 2).
CT arthrography of the knee with ACL partial tear and bell hammer; CT 3D volume acquisition in the axial plane with reconstructions. a Sagittal reconstruction: the anteromedial bundle tilted anteriorly in the intercondylar notch; b Sagittal reconstruction: the posterolateral bundle remains continuous and tense while the anteromedial bundle is retracted forward; c Coronal reconstruction: ovoid mass of intermediate density, in the midline, surrounded by the contrast product corresponding to the stump of the anteromedial bundle; d Sagittal reconstruction: continuity of ligament fibres of the posterolateral bundle
On arthroscopy
As previously described [11, 20], the bell hammer is a mobile stump in the intercondylar notch of the ACL. It is pedunculated and inserts in the fibres of the ligament on the footprint of the native ACL. If surgery is performed early, the stump is bleeding, irregular and fibrous, suggesting a recent ligament tear. If surgery is delayed, the tendon stump is rounder and smoother (like a sea pebble) (Fig. 3). In both cases, the stump is often vascularized and veins are often visible on the periphery. Its orientation is mostly in front and external, but it is sometimes more central to the intracondylar notch. It may be difficult to see when the knee is flexed as it is hidden under the Hoffa fat pad, but when the knee is extended, it can always be identified. If the stump is very large, it takes the form of the intracondylar notch creating anterior impingement. Finally, it can usually be moved with a hook and looks like “a bell hammer turned upwards” (Fig. 4).
Arthroscopic view of the bell hammer in case of complete ACL tear. a Central stump with complete disappearance of the posterolateral bundle; b Bulky stump corresponding to the two torn bundles; c Old ACL tear with a bell hammer remodelled and flattened; d Bell-hammer tear of anteromedial and posterolateral bundles lying in the notch
Evaluation criteria
All preoperative MRIs were analysed retrospectively by a senior radiologist who is specialized in musculoskeletal imaging to identify the bell-hammer sign and also partial tears. The radiologist was blinded to arthroscopic findings. On MRI, a tear was considered to be partial in the presence of hyperintense intraligamentary images on one or more successive views associated with a concave ligament bundle and/or local thinning with continuous and well-oriented fibres [6, 24].
At arthroscopy, three senior surgeons noted the presence of the bell-hammer sign and whether the tears were complete or partial. The diagnosis was partial if fibres were found to be discontinuous but the ligament remained taut.
Patients
During the study period, 312 patients underwent ACL reconstruction in our department for partial or total tears. All patients underwent a preoperative MRI. The series included 312 patients, 83 women and 229 men (mean age 33.3 ± 19.6 years). Arthroscopy did not show any normal ACL, 247/312 (79.2 %) complete tears and 65/312 (20.8 %) partial tears, 50/65 (76.9 %) in the AM bundle and 15/65 (23.1 %) in the PL bundle. The bell hammer was excised arthroscopically, and partial tears all underwent unifascicular reconstruction during the same surgical procedure.
Statistical analysis
The performance parameters of MRI with and without the bell-hammer sign in the diagnosis of partial tears were calculated in relation to the gold standard test, arthroscopy: sensitivity (Se), specificity (Sp), accuracy, positive and negative likelihood ratio (LR+, LR−), positive predictive value (PPV) and negative predictive value (NPV). Differences were determined by the nonparametric Fisher’s exact test for categorical variables. A p value <0.05 was considered to be significant.
Results
The bell-hammer sign was found in 13/312 patients (4.2 %) on MRI and in 14/312 patients (4.5 %) on arthroscopy; thus, 1/14 case of this sign was not identified on MRI. This subgroup included 9 men and 5 women (mean age 28.1 ± 9.1 years). All injuries were sports related, mostly skiing and handball. Patients all had an extension deficit during the initial clinical examination with an average loss of extension of 7.1 ± 3.4 ° which could not be reduced under anaesthesia. MRI was performed in this group 2 days to 3 months after the accident and arthroscopy within a mean of 3.2 ± 1.9 months (15 days–7 months) after trauma. At arthroscopy, 9/14 (64.3 %) had partial tears and 2/9 (22.2 %) of these were diagnosed on MRI by conventional MRI criteria.
The bell-hammer sign was found on MRI in 9/65 (13.8 %) partial tears, all of the AM bundle, and in 4/247 (1.6 %) complete tears, significantly more frequent in cases of partial rupture (p < 0.0001). MRI diagnosed a partial tear without the bell-hammer sign in 15/65 cases (sensitivity CI95 % = 23.1 ± 10 %, specificity CI95 % = 95.9 ± 2.5 %) and with the bell-hammer sign in 23/65 cases (sensitivity CI95 % = 35.4 ± 11 %, specificity CI95 % = 93.9 ± 3 %), not significantly (Table 1). The likelihood of having a bell hammer was 6.9 times higher in a patient with partial tears. The negative likelihood ratio was high (0.96), indicating that the absence of this sign did not exclude a partial tear.
Discussion
The most important finding of the present study was that adding the bell-hammer sign to the existing criteria for the diagnosis of ACL partial tears improves the diagnostic sensitivity of MRI. On the other hand, the absence of this sign did not exclude this diagnosis. The bell-hammer sign was significantly more frequent in case of ACL partial tears.
While the cyclops syndrome described by Jackson and Schaefer [9] in 1990 after ACL reconstruction is well known and involves 2.2–21 % of patients [3, 5], the preoperative cyclops has not been clearly described in the literature. Most authors describe case reports [8, 11, 13, 20, 23], and a few series have been published [1, 7, 12, 16, 17]. The bell-hammer sign must be identified on MRI in patients with loss of extension to detect nodules in the intercondylar notch that could prevent functional recovery if excision is not performed [16]. In our patients, the block in extension was confirmed by failure to reduce the flexion contracture under anaesthesia.
In the population of this study, 4.5 % of patients had a preoperative cyclops syndrome, which is comparable to the estimation by Tonin et al. [20].
All of the patients in the series by Monaco et al. [12] and Chun et al. [1] with the preoperative cyclops had a partial tear. Only the series by Servien [17] found more complete than partial tears. Moreover, in our study as in that by Nakawaga et al. [13], the bell-hammer sign in case of partial tear was associated with a tear in the AM bundle. In the series by Chun et al. [1] with 19 patients, tears were all associated with the PL bundle. In the study by Sonnery-Cottet et al. [18] with 37 partial tears of the ACL, only 15 patients with isolated tears of the PL bundle had a preoperative cyclops. This difference may be because it is difficult for the surgeon to definitely confirm the broken bundle [15] especially since peri-arthroscopic evaluation was performed by a single surgeon in all these cases. The other hypothesis is that this is not a single bundle or partial tear but an injury to groups of fibres in the ACL in varying proportions. The term incomplete tears may be more appropriate than partial, with a continuous gradient of the proportion of broken ACL fibres.
The preoperative diagnosis on MRI of partial tears of the ACL is controversial [2] and considered to be imprecise. It is a concept that is also found in the series with preoperative cyclops. In the first series published in 1982 [12], arthrography was performed in 7/19 patients who were usually referred for meniscal tears. In the series by Runyan et al. [20], 5/10 cases of preoperative cyclops were diagnosed as partial tears on MRI. In a series of 30 preoperative cyclopes by Servien et al. [17], 11 partial tears were not diagnosed on MRI. However, none of these series explored the role of the bell-hammer sign in the diagnosis of ACL partial tears.
Although patients had a flexion contracture during the initial clinical examination due to a mechanical block, the case report by Veselko et al. [23] described a progressive loss of extension and knee locking several weeks after the patient, who did not undergo surgery initially, had returned to sports. A pedunculated nodule attached to the anterolateral part of the ACL was identified on arthroscopy. Histological results of the excised nodule showed the presence of bone fragments. For the authors, the symptoms were secondary to chronic reactive inflammation to a foreign body from the bone fragments and not broken fibre residue.
The most important interest of the bell-hammer sign in the day-to-day clinical work is to suggest partial tears on MRI. For patients with loss of extension, the excision of this nodule must be planned in order to obtain full functional recovery.
This study had several limitations. Although the study population was large, allowing us to determine prevalence, it only included patients who underwent surgical reconstruction. The study was retrospective, and histological analysis of excised nodules was not performed.
Conclusion
The most important interest of the bell-hammer sign in the day-to-day clinical work is to suggest partial tears on MRI. It aids making a diagnosis, but its absence does not exclude partial ACL rupture.
References
Chun CH, Lee BC, Yang JH (2002) Extension block secondary to partial anterior cruciate ligament tear on the femoral attachment of the posterolateral bundle. Arthroscopy 18:227–231
Cohen SB, Van Beek C, Starman JS et al (2009) MRI measurement of the 2 bundles of the normal anterior cruciate ligament. Orthopedics 32:687
Dandy DJ, Edwards DJ (1994) Problems in regaining full extension of the knee after anterior cruciate ligament reconstruction: does arthrofibrosis exist? Knee Surg Sports Traumatol Arthrosc 2:76–79
DeFranco MJ, Bach BR (2009) A comprehensive review of partial anterior cruciate ligament tears. J Bone Joint Surg Am 91:198–208
Delcogliano A, Franzese S, Branca A et al (1996) Light and scan electron microscopic analysis of cyclops syndrome: etiopathogenic hypothesis and technical solutions. Knee Surg Sports Traumatol Arthrosc 4:194–199
Duc SR, Zanetti M, Kramer J et al (2005) Magnetic resonance imaging of anterior cruciate ligament tears: evaluation of standard orthogonal and tailored paracoronal images. Acta Radiol 46:729–733
Huang GS, Lee CH, Chan WP et al (2002) Acute anterior cruciate ligament stump entrapment in anterior cruciate ligament tears: MR imaging appearance. Radiology 225:537–540
Irisawa H, Takahashi M, Hosokawa T, Nagano A (2007) Cyclops syndrome occurring after chronic partial rupture of the anterior cruciate ligament without surgical reconstruction. Knee Surg Sports Traumatol Arthrosc 15:144–146
Jackson DW, Schaefer RK (1990) Cyclops syndrome: loss of extension following intra-articular anterior cruciate ligament reconstruction. Arthroscopy 6:171–178
Lawrance JA, Ostlere SJ, Dodd CA (1996) MRI diagnosis of partial tears of the anterior cruciate ligament. Injury 27:153–155
McMahon PJ, Dettling JR, Yocum LA, Glousman RE (1999) The cyclops lesion: a cause of diminished knee extension after rupture of the anterior cruciate ligament. Arthroscopy 15:757–761
Monaco BR, Noble HB, Bachman DC (1982) Incomplete tears of the anterior cruciate ligament and knee locking. JAMA 19(247):1582–1584
Nakagawa T, Hiraoka H, Fukuda A et al (2006) Symptomatic cyclops lesion after rupture of the anteromedial bundle of the anterior cruciate ligament. J Orthop Sci 11:537–540
Palle L, Reddy B, Reddy J (2010) Sensitivity and specificity of vertically oriented lateral collateral ligament as an indirect sign of anterior cruciate ligament tear on magnetic resonance imaging. Skeletal Radiol 39:1123–1127
Petersen W, Zantop T (2006) Partial rupture of the anterior cruciate ligament. Arthroscopy 22:1143–1145
Runyan BR, Bancroft LW, Peterson JJ et al (2007) Cyclops lesions that occur in the absence of prior anterior ligament reconstruction. Radiographics 27:e26
Servien E, Ait Si Salmi T, Neyret P (2003) Bell-hammer tear of anterior cruciate ligament. J Traumatol Sport 20:72–75
Sonnery-Cottet B, Barth J, Graveleau N et al (2009) Arthroscopic identification of isolated tear of the posterolateral bundle of the anterior cruciate ligament. Arthroscopy 25:728–732
Steckel H, Vadala G, Davis D et al (2006) 2D and 3D 3-tesla magnetic resonance imaging of the double bundle structure in anterior cruciate ligament anatomy. Knee Surg Sports Traumatol Arthrosc 14:1151–1158
Tonin M, Saciri V, Veselko M, Rotter A (2001) Progressive loss of knee extension after injury. Cyclops syndrome due to a lesion of the anterior cruciate ligament. Am J Sports Med 29:545–549
Van Dyck P, Vanhoenacker FM, Gielen JL et al (2011) Three tesla magnetic resonance imaging of the anterior cruciate ligament of the knee: can we differentiate complete from partial tears? Skeletal Radiol 40:701–707
Van Dyck P, De Smet E, Veryser J et al (2012) Partial tear of the anterior cruciate ligament of the knee: injury patterns on MR imaging. Knee Surg Sports Traumatol Arthrosc 20:256–261
Veselko M, Rotter A, Tonin M (2000) Cyclops syndrome occurring after partial rupture of the anterior cruciate ligament not treated by surgical reconstruction. Arthroscopy 16:328–331
Walker CW, Moore TE (1997) Imaging of skeletal and soft tissue injuries in and around the knee. Radiol Clin North Am 35:631–653
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lefevre, N., Naouri, J.F., Bohu, Y. et al. Sensitivity and specificity of bell-hammer tear as an indirect sign of partial anterior cruciate ligament rupture on magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc 22, 1112–1118 (2014). https://doi.org/10.1007/s00167-013-2511-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2511-2