Abstract
Purpose
Previous research has demonstrated that women have a higher risk of anterior cruciate ligament (ACL) injury than men. Tibiofemoral articular geometry may play a role in the occurrence of ACL tears. The purpose of this study was to analyze the gender-specific geometric characteristics differences in tibiofemoral morphology in ACL-deficient patients.
Methods
Medial tibial slope (MTS), lateral tibial slope (LTS), medial tibial plateau concavity, medial and lateral femoral condyle convexity, and lateral plateau convexity were analyzed in 276 patients with complete ACL injuries (138 females and 138 males). Two blinded observers measured the anatomical parameters of tibiofemoral geometry with use of multiplanar CT scans. Intra- and inter-rater reliabilities were assessed and comparisons between anatomic measures were made between male and female patients.
Results
The average ICC for all measurements was 0.90 (range 0.83–0.97) indicating good reliability. Male ACL injured patients demonstrated significantly greater LTS (10.5° ± 2.8) than female patients (9.6° ± 3.5°; p < 0.05). No gender difference in MTS was found (n.s.). Medial and lateral femoral condyle convexity and medial tibial plateau concavity were greater in males than females (all p < 0.05). Lateral tibial plateau convexity in females was higher than in males (p < 0.001). The medial and lateral compartments were found to be more incongruent in females than males (p < 0.01 and p < 0.001, respectively).
Conclusions
Female patients were noted to have more incongruent medial and lateral compartments than male patients. These gender-specific differences in joint morphology may contribute to graft tear risk and outcomes of ACL reconstruction; however, comparative clinical studies are needed to confirm this possibility.
Level of evidence
3.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although the pathophysiology of anterior cruciate ligament (ACL) rupture is still incompletely elucidated, this risk appears to be multifactorial, including a combination of anatomical, hormonal, genetic, positional, neuromuscular and environmental factors [2, 10, 16]. Patient weight and height [40], the size and depth of the intercondylar notch [22], the diameter of the ACL [6], the magnitude of tibial slope [4, 37, 46], the volume of the tibial spines, the convexity of the lateral tibiofemoral articular surfaces, and the concavity of the medial tibial plateau [14] have been associated with ACL rupture. Moreover, there appears to be a specific influence of female gender on these risk factors [14, 17, 26], but relationship between sex and anatomic parameters as a risk factor for ACL injury has not been evaluated. A higher risk of non-contact ACL tear has been shown in women with an incidence two to five times noted in men [1, 10, 45] and a previous study has shown a 33.7% greater risk of subsequent contralateral ACL reconstruction in female patients [35].
Widespread use of MRI [11, 25] and CT scans [28, 30, 31, 47] in the evaluation of ACL injuries has allowed a more detailed analysis of three-dimensional tibiofemoral joint morphology. Increased posterior tibial slope appears to be an important risk factor for ACL tears [4, 39], although controversy remains [17, 27, 37]. A greater medial or lateral tibial slope, a low concavity of the medial tibial plateau [14], more convex lateral articular surfaces, as well as a narrow lateral tibial plateau [43] have been identified as risk factors for ACL rupture. However, these risk factors differ significantly between males and females [14, 38] and may be confounded in analyses that do not stratify by sex. Sturnick et al. [38] insisted on the need for independent analysis in individuals of both sexes and pointed out that female representation in these studies is rarely equivalent to male representation. Similarly, variables that have a large effect on risk in only one sex may erroneously appear to have an effect on both sexes in aggregate analyses.
Few studies have attempted to identify risk factors for ACL rupture specifically for individuals of both sexes. Wahl et al. [43] reported a higher risk of ACL tear in men with greater lateral convexity of the femoral condyle or lateral tibial plateau, or a greater narrowness of the lateral plateau. These findings were not found in women. Hohmann et al. [17] were able to show in a large series of 544 patients the influence of the posterior–inferior tibial slope on ACL rupture only in women.
To our knowledge, no study has included a three-dimensional combined analysis of femoral and tibial bone geometry of both tibiofemoral compartments based on sex. The goal of this study was to evaluate the sagittal tibiofemoral articular geometry in a cohort of male and female patients with a first ACL rupture using CT scans to assess gender-specific differences. It was hypothesized that female patients would demonstrate more incongruent medial and lateral tibiofemoral compartments than male patients. These differences in joint geometry may contribute to ACL injury risk.
Materials and methods
This retrospective study included a series of patients who underwent primary ACL reconstruction at our center between 2012 and 2016 who then underwent a postoperative knee CT scan. Subjects were included if they had no additional ligament injuries, no cartilage injuries or fractures. Patients were excluded if they had moderate or severe knee osteoarthritis (IKDC grade C or D). All subjects were skeletally mature with a complete ACL tear. None of the subjects had undergone previous knee surgery.
Evaluation methods
CT scans were performed postoperatively, as a routine examination when possible (initially for the evaluation of the positioning of femoral and tibial tunnels after ACL reconstruction), and analyzed in our Institutional Picture Archiving and Communications System (PACS, Centricity, GE Healthcare, Waukesha, WI). All examinations were carried out in the same institutional radiology department. The images were acquired in axial sections from which reconstructions in the coronal and sagittal planes were carried out by an experienced orthopaedic surgeon. No postoperative artifacts degraded the quality of CT scans. The distal femoral and proximal tibial epiphyseal regions were analyzed in three dimensions. The tests were carried out on CR-Brillance equipment CT 64 using a volume acquisition technique without injection (thickness 0.67 mm; increment 0.33 mm; 140 kVp; MAs 300 ; high resolution; no automatic dose modulation; collimation 16 × 0.625 mm; pitch 0.435; rotation 0.75 s/rev; FOV 250 mm).
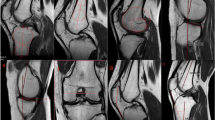
All images were analyzed using the image processing software (Philips® Intellispace Portal 7.0, Haifa, Israel) after import in DICOM format. Image processing was done in the CT Viewer in MPR mode, with double-obliquity image processing techniques. Treatment of the acquisitions was done after positioning of the tibia in three dimensions (Fig. 1): an axial plane passing through the center of the medial (point A) and lateral (point B) tibial plateaus (plane 1) controlling rotation of the tibia, a coronal plane including the longitudinal anatomical axis (plane 2), and a sagittal plane through the proximal tibial anatomic axis (PTAA, plane 3). Measurements of the distal femoral epiphysis were made with respect to the tibia-defined cutting planes.
CT measurements were performed using the tools in PACS. The measuring instrument in the software was used to define angles to within 0.1° and lengths to within 0.1 mm for measured distances.
Sagittal geometry evaluation
All measures used subchondral bone as a reference. A wide scanning method which applied several consecutive cuts made it possible to consider on the same image the simultaneous reconstruction of at least 25 images (a minimum of 15 mm) of bone.
The tibial slope evaluation was based on the radiological work of Bonnin et al. [7] and the CT scan evaluation of Kessler et al. [20], using the proximal tibial anatomic axis (PTAA), which has been shown to be strongly correlated to the mechanical tibial axis [5, 41, 44] and has been used by the American Knee Society [8]. The first step was to determine the PTAA by connecting two equidistant points of the anterior and posterior tibial cortices, one just under the anterior tibial tuberosity and a second 10 cm more distal. The wide scan allowed visualization of the entire anterior and posterior cortices on the same image, creating a real three-dimensional reconstruction. The previously defined PTAA was then applied to both the medial and lateral tibial plateaus on a mid-sagittal section (Fig. 2). The wide scanning method provided visualization of the entire bone relief on the same image by superimposing multiple adjacent cuts on both sides of the sagittal plane passing through the center of each plateau.
Medial tibial slope (MTS) was defined by the angle formed between the PTAA and the line joining the most proximal points of the anterior and posterior margins of the upper medial tibial plateau (Fig. 3). The value of the posterior slope corresponded to the difference between the angle obtained and the perpendicular to the PTAA. A posterior inclination was assigned a positive value, while an anterior inclination was assigned a negative value, according to convention [7, 9].
The same methodology was reproduced for the lateral compartment. The angle formed by the line joining the most anterior and posterior point of the subchondral surface and the perpendicular to the PTAA determined the lateral tibial slope (Fig. 4).
For the following measures, the methods of Wahl et al. [43] was used with simplification of the technique in order to describe the convexities or concavities of the articular surfaces.
-
Anterior–posterior medial tibial plateau length (MPL) and lateral tibial plateau length (LPL).
The maximum anterior–posterior articular length of the medial and lateral tibial plateaus were defined by the anatomy of each plateau (top of the concavity for the medial tibial plateau, base of the convexity for the lateral one) and were measured as the distance between the most anterior and posterior margins of the tibial plateau subchondral bone.
-
Anterior–posterior medial (MCL) and Lateral (LCL) femoral condyle lengths.
For each medial or lateral compartment, the maximum anterior–posterior length of the femoral condyle was measured on a sagittal reconstruction. It was defined as the greatest distance between the anterior and posterior articular surfaces of each condyle. The measurement technique used in a previous study by Musahl et al. [29] was used in which the distance between the junction point between femoral condyle and front trochlea and the point in the middle of the posterior articular condylar surface was measured.
Men have larger absolute anatomical measurements than women. Therefore, in addition to calculating absolute values for femoral condyle and tibial plateau lengths, ratios of the femur size relative to the tibia in the medial and lateral compartments were also calculated. These measurements were reported as the medial compartment ratio (MCR = MCL/MPL) and lateral compartment ratio (LCR = LCL/LPL).
For each of the maximal anterior–posterior lengths previously described, a perpendicular line was created between the line used to measure the length of the surface and the most distant subchondral bone. The length of this line was defined at the height of each osseous element: medial femoral condyle height (MCH), lateral femoral condyle height (LCH), medial tibial plateau height (MPH), and lateral tibial plateau height (LPH). The concavity or convexity of each element was described by the ratio of this vertical line to its anterior–posterior length, with higher values signifying increased convexity or concavity.
Femoral condyle convexities (medial condyle convexity, MCC = MCH/MCL and lateral condyle convexity, LCC = LCH/LCL), and tibial plateau concavity (medial plateau concavity, MPC = MPH/MPL) or convexity (lateral plateau convexity, LPC = LPH/LPL) were considered.
The global articular congruence of the medial compartment (medial congruency, MC) was calculated as the sum of the medial femoral condyle convexity (MCC) and the medial tibial plateau concavity (MPC) (Fig. 5). Because these two variables moved in the same direction, a lower overall value defined lower medial articular congruency, and a higher overall value defined higher medial articular congruency.
The global articular convexity of lateral compartment (lateral congruency LC) was similarly calculated by adding the lateral femoral condyle convexity (LCC) and the lateral tibial plateau convexity (LPC) (Fig. 6). A higher value corresponded to lower lateral congruency with more convex joint surfaces.
This study was approved by the institutional review board of the Hospices Civils de Lyon and the protocol number for this approval was 2016-037.
Statistical analysis
Statistical analyses were performed by the Laboratory of Biostatistics at our institution using R software (version 3.1.1, Copyright © 2014 The R Foundation for Statistical Computing Platform). A value of p < 0.05 was considered statistically significant. The normality of the different variables variances was checked by Kolmogorov–Smirnov tests. Continuous variables were expressed as mean ± standard deviation. Student’s t tests for independent samples were used to compare parametric variables and Mann–Whitney–Wilcoxon tests were used for comparison of non-parametric variables. Linear correlations used Pearson correlations.
CT scan measurement reliability
To assess the reproducibility of the different measurements, intra-class correlations (ICC) were calculated. An ICC value greater than 0.9 was considered excellent and a value between 0.9 and 0.8 was considered good [15, 21]. Intra-observative variability was assessed by the same surgeon re-measuring an arbitrarily set random sample of 50 patients 2 weeks after the initial analysis of all 276 CT scans. An independent radiologist measured CT scans from another arbitrarily set random sample of 50 patients to determine inter-observer variability.
Results
Seven hundred and eighty-six patients underwent ACL reconstruction at our institution during the inclusion period, including 456 men (58%). 355 post operative CT scans were available, including 138 female CT scans, which were matched at random to 138 scans of male patients who met the inclusion and exclusion criteria. Mean age at surgery was 32 ± 12 years. Mean time from injury to operation was 19 ± 37 months. The injury was sports related in 88% of the cases. Skiing was the largest cause of ACL tears (29%), followed by soccer (22%). Mean body mass index was 24 ± 3.6 kg/m2. Pre-reconstruction IKDC grade was C or D in 81% of patients in the cohort. Median pre-injury Tegner score was 7.
The reproducibility of the measurements after reconstruction of the tibial and femoral bone segments in dedicated image processing software was good to excellent, with ICCs between 0.83 and 0.97 (Table 1). The average ICC for all measurements was 0.90.
Concerning sagittal geometry, mean medial tibial slope was 9.8° ± 2.8° and mean lateral tibial slope 10.1° ± 3.2° (n.s.). Medial tibial slope was similar in males and females (n.s.), while lateral tibial slope was significantly greater in males (p = 0.02). Women had smaller absolute anatomical measurements than men in sagittal analysis. These measurements were strongly correlated with patient size (p < 0.001). However, the correlation coefficients found were lower for women, ranging from 0.5 to 0.6, while the coefficients were between 0.8 and 0.9 for men. The tibiofemoral ratios were not correlated with patient size, either in the overall population or in a stratified gender analysis. Anterior–posterior length ratios for medial and lateral compartment were greater in females than in males (p = 0.01 and p = < 0.001, respectively). Tibiofemoral geometric characteristics are summarized in Tables 2 and 3.
Women exhibited lower medial (p = 0.03) and lateral (p < 0.01) femoral convexities and lower medial tibial concavity (p < 0.01) than men. Overall, women had a lower medial tibiofemoral congruency than men (p < 0.01) and lateral tibial convexity was about 1.5 times greater than males (p < 0.001).
Discussion
The most important findings of this study were that in an ACL-injured population, females did not have higher posterior tibial slope than males, but showed more incongruency in their lateral tibiofemoral compartments. These differences, in association with decreased congruency of the medial compartment, likely contribute to increased risk of pathologic anterior translation of the lateral tibial plateau and subsequent higher risk of ACL rupture in females.
The findings of this study with regard to posterior tibial slope further contribute to a contradictory group of prior studies. Brandon et al. [4], in a radiological analysis of 100 ACL-deficient patients (66 men and 34 women), found no significant difference between men and women concerning the posterior–inferior tibial slope and showed similar findings in a group of 100 patients with patellofemoral pain syndrome (49 men and 51 women). In contrast, Hashemi et al. [13] in 2008 performed an MRI analysis of 55 patients without ACL injury and reported greater medial and lateral posterior tibial slopes in women than in men. In 2010 this same author [14] evaluated 49 ACL-injured patients and found no differences in medial or lateral slope or concavity of the medial tibial plateau based on sex.
The results of the current study regarding the size of the femoral condyles and tibial plateau were consistent with the recent literature. Wahl et al. [43] found mean values of anterior–posterior lateral condylar length of 71.1 and 65.5 mm, lateral tibial plateau length of 33 and 29.5 mm, and sagittal femoral-tibial ratio of 2.20 and 2.22, in 101 men and 72 women, respectively. We similarly observed this significantly greater femoral–tibial disproportion in the sagittal plane in women compared to men. A “bulky” femur facing a “narrow” tibial plateau in the sagittal plane could promote greater tibiofemoral instability.
In addition to the effects of slope and tibiofemoral ratio, the relative congruence of the medial and lateral compartments may also contribute to increased risk of ACL rupture in. In our study, women had a less congruent medial tibiofemoral compartment than men, with a lower medial femoral convexity and a lower medial tibial concavity. Concerning the lateral tibiofemoral compartment, women had a larger relative tibial convexity than men (about 1.5 times greater), whereas their femoral condyle appeared flatter. The overall congruence of this compartment was smaller in women, with a higher cumulative convexity than that noted in men.
These convexities were relative, taking into account anteroposterior tibial and femoral lengths, in contrast to Hashemi et al. [13] who found no significant difference based on sex between absolute convexity values. Wahl et al. [43] observed a shorter lateral condylar and tibial plateau radii of curvature in women, in favor of greater convexity of these anatomical structures in female patients with ACL rupture. This difference in convexity was found only at the level of the lateral tibial plateau. The technique of measuring the radius of femoral curvature according to a Fibonacci turn used by Wahl et al. was different and could increase the convexity of the external femoral condyle by considering the height of the condyle at the point of contact between the femur and the tibia, including the chondral thickness (MRI acquisitions). Our CT-based method allowed us to analyze only the subchondral surface.
The results of this study show that female articular anatomy is more prone to include specific factors that may lead to higher risk of anteroposterior and rotational instability and thus potential rupture of the ACL. While the influence of an excessive tibial slope on anterior and rotational laxity has been widely evaluated and confirmed [7, 32, 36], low joint congruence may also be a contributor to “at risk” anatomy for ACL injury. Very few studies to date have analyzed the influence of tibiofemoral congruency on the anterior tibial translation and rotational laxity. Further studies on the correlation between articular geometry and anterior laxity are needed.
Major strengths of this work are the size of the cohort and the equal number of males and females in the study. This is the first study with an equal proportion of individuals of both sexes, making the statistical analysis stronger. Further, the reproducibility of CT-based measurements was good to excellent. The majority of previous studies used images acquired via MRI to describe knee joint geometry, subjectively determining for each compartment a sagittal cut passing through the center of the compartment [3, 13, 14, 23, 43] because 3D reconstruction is not generally available for MRI. To avoid this measurement bias, we chose to perform a wide scan in a multiplanar mode, accounting for the global geometry by superimposing many adjacent cuts. A representation of the epiphysis was obtained, analyzed and controlled in three dimensions, greatly improving the inter- and intra-observer reliability of the methodology.
There are several limitations of the current study. First, the femoral and tibial epiphyses were not independently analyzed on separate reconstructions. The femoral measurements were made with respect to the tibial acquisitions, and we could not completely rule out possible rotation between the two bone segments. However, the evaluation of intra- and inter-observer correlations was found to be high. Moreover, blinding according sex was not ensured because first names were visible during measurements. Further, the decision to explore articular geometry by means of a CT-based method did not allow us to account for the influence of the soft tissues on joint congruence and slope. Both articular cartilage and meniscus may alter joint congruity and slope and differences in these structures may exist between men and women. It has been recently demonstrated that the meniscal tibial slope was significantly lower than the bony tibial slope for both the medial and lateral compartments. Lustig et al. [24] reported a reduction of the tibial slope of 1.8° in the medial compartment and 5.5° in the lateral compartment when considering the meniscus. However, this finding was not influenced significantly by sex. Finally, the tibia was not visualized in its entirety on the CT images and there could therefore be some measurement bias in the determination of the proximal anatomical tibial axis.
The findings of this study contribute to the understanding of anatomical risk factors for higher ACL injury risk in female patients. While the clinical application of these data to an individual patient cannot be confirmed by the current study, anatomic analysis such as those performed in the current study could provide insight why an ACL graft failed in a given patient when considered in association with other anatomical (laxity, tibial slope), demographic, surgical, and neuromuscular factors.
Conclusion
Female patients were noted to have more incongruent medial and lateral compartments than male patients. These differences in tibiofemoral joint geometry may contribute to ACL injury risk, graft tear risk and should be further investigated.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- MTS:
-
Medial tibial slope
- LTS:
-
Lateral tibial slope
- CT:
-
Computerized tomography
- ICC:
-
Intra-class correlation
- MRI:
-
Magnetic resonance imaging
- IKDC:
-
International knee documentation committee
- PACS:
-
Picture archiving and communications system
- FOV:
-
Field of view
- DICOM:
-
Digital imaging and communications in medicine
- MPR:
-
Multi-planar reconstruction
- PTAA:
-
Proximal tibial anatomic axis
- MPL:
-
Medial tibial plateau length
- LPL:
-
Lateral tibial plateau length
- MCL:
-
Medial femoral condyle length
- LCL:
-
Lateral femoral condyle length
- MCR:
-
Medial compartment ratio
- LCR:
-
Lateral compartment ratio
- MCH:
-
Medial femoral condyle height
- LCH:
-
Lateral femoral condyle height
- MPH:
-
Medial tibial plateau height
- LPH:
-
Lateral tibial plateau height
- MCC:
-
Medial condyle convexity
- LCC:
-
Lateral condyle convexity
- MPC:
-
Medial plateau concavity
- LPC:
-
Lateral plateau convexity
- MC:
-
Medial femorotibial congruency
- LC:
-
Lateral femorotibial congruency
- SD:
-
Standard deviation
- mm:
-
Millimeters
- CI:
-
Confidence interval
References
Arendt EA, Agel J, Dick R (1999) Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train 34(2):86–92
Bowers AL, Spindler KP, McCarty EC, Arrigain S (2005) Height, weight, and BMI predict intra-articular injuries observed during ACL reconstruction: evaluation of 456 cases from a prospective ACL database. Clin J Sport Med 15(1):9–13
Bozkurt M, Unlu S, Cay N, Apaydin N, Dogan M (2014) The potential effect of anatomic relationship between the femur and the tibia on medial meniscus tears. Surg Radiol Anat 36:741–746
Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF (2006) The association between posterior–inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 22(8):894–899
Brazier J, Migaud H, Gougeon F, Cotten A, Fontaine C, Duquennoy A (1996) Evaluation of methods for radiographic measurement of the tibial slope. A study of 83 healthy knees. Rev Chir Orthop Reparatrice Appar Mot 82(3):195–200
Chaudhari AM, Zelman EA, Flanigan DC, Kaeding CC, Nagaraja HN (2009) Anterior cruciate ligament-injured subjects have smaller anterior cruciate ligaments than matched controls: a magnetic resonance imaging study. Am J Sports Med 37(7):1282–1287
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76(5):745–749
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res (248):9–12
Genin P, Weill G, Julliard R (1993) The tibial slope. Proposal for a measurement method. J Radiol 74(1):27–33
Griffin LY, Agel J, Albohm MJ et al (2000) Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 8(3):141–150
Haddad B, Konan S, Mannan K, Scott G (2012) Evaluation of the posterior tibial slope on MR images in different population groups using the tibial proximal anatomical axis. Acta Orthop Belg 78(6):757–763
Harner CD, Paulos LE, Greenwald AE, Rosenberg TD, Cooley VC (1994) Detailed analysis of patients with bilateral anterior cruciate ligament injuries. Am J Sports Med 22(1):37–43
Hashemi J, Chandrashekar N, Gill B et al (2008) The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am 90(12):2724–2734
Hashemi J, Chandrashekar N, Mansouri H et al (2010) Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38(1):54–62
Helito CP, Helito PV, Costa HP et al (2014) MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skelet Radiol 43(10):1421–1427
Hewett TE, Myer GD, Ford KR et al (2005) Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med 33(4):492–501
Hohmann E, Bryant A, Reaburn P, Tetsworth K (2011) Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surg Sports Traumatol Arthrosc 19(Suppl 1):S109-114
Hooper GJ (1986) Radiological assessment of anterior cruciate ligament deficiency. A new technique. J Bone Joint Surg Br 68(2):292–296
Jacobsen K (1976) Stress radiographical measurement of the anteroposterior, medial and lateral stability of the knee joint. Acta Orthop Scand 47(3):335 – 334
Kessler MA, Burkart A, Martinek V, Beer A, Imhoff AB (2003) Development of a 3-dimensional method to determine the tibial slope with multislice-CT. Z Orthop Ihre Grenzgeb 141(2):143–147
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
LaPrade RF, Burnett QM 2nd (1994) Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. A prospective study. Am J Sports Med 22(2):198–202 (discussion 203)
Lustig S, Scholes CJ, Costa AJ, Coolican MJ, Parker DA (2013) Different changes in slope between the medial and lateral tibial plateau after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):32–38
Lustig S, Scholes CJ, Leo SP, Coolican M, Parker DA (2013) Influence of soft tissues on the proximal bony tibial slope measured with two-dimensional MRI. Knee Surg Sports Traumatol Arthrosc 21(2):372–379
Matsuda S, Miura H, Nagamine R et al (1999) Posterior tibial slope in the normal and varus knee. Am J Knee Surg 12(3):165–168
McNair PJ, Wood GA, Marshall RN (1992) Stiffness of the hamstring muscles and its relationship to function in anterior cruciate ligament deficient individuals. Clin Biomech (Bristol Avon) 7(3):131–137
Meister K, Talley MC, Horodyski MB, Indelicato PA, Hartzel JS, Batts J (1998) Caudal slope of the tibia and its relationship to noncontact injuries to the ACL. Am J Knee Surg 11(4):217–219
Meric G, Gracitelli GC, Aram L, Swank M, Bugbee WD (2015) Tibial slope is highly variable in patients undergoing primary total knee arthroplasty: analysis of 13,546 computed tomography scans. J Arthroplasty 30(7):1228–1232
Musahl V, Ayeni OR, Citak M, Irrgang JJ, Pearle AD, Wickiewicz TL (2010) The influence of bony morphology on the magnitude of the pivot shift. Knee Surg Sports Traumatol Arthrosc 18(9):1232–1238
Nunley RM, Nam D, Johnson SR, Barnes CL (2014) Extreme variability in posterior slope of the proximal tibia: measurements on 2395 CT scans of patients undergoing UKA? J Arthroplasty 29(8):1677–1680
Puthumanapully PK, Harris SJ, Leong A, Cobb JP, Amis AA, Jeffers J (2014) A morphometric study of normal and varus knees. Knee Surg Sports Traumatol Arthrosc 22(12):2891–2899
Rahnemai-Azar AA, Abebe ES, Johnson P, Labrum J, Fu FH, Irrgang JJ, Samuelsson K, Musahl V (2017) Increased lateral tibial slope predicts high-grade rotatory knee laxity pre-operatively in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 25:1170–1176
Renstrom P, Ljungqvist A, Arendt E et al (2008) Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med 42(6):394–412
Siebold R, Axe J, Irrgang JJ, Li K, Tashman S, Fu FH (2010) A computerized analysis of femoral condyle radii in ACL intact and contralateral ACL reconstructed knees using 3D CT. Knee Surg Sports Traumatol Arthrosc 18(1):26–31
Snaebjörnsson T, Hamrin Senorski E, Sundemo D, Svantesson E, Westin O, Musahl V, Alentorn-Geli E, Samuelsson K (2017) Adolescents and female patients are at increased risk for contralateral anterior cruciate ligament reconstruction: a cohort study from the Swedish National Knee Ligament Register based on 17,682 patients. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-017-4517-7
Song G, Zhang H, Wang Q, Zhang J, Li Y, Feng H (2016) Risk factors associated with grade 3 pivot shift after acute anterior cruciate ligament injuries. Am J Sports Med 44:362–369
Stijak L, Herzog RF, Schai P (2008) Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case–control study. Knee Surg Sports Traumatol Arthrosc 16(2):112–117
Sturnick DR, Vacek PM, DeSarno MJ et al (2015) Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med 43(4):839–847
Todd MS, Lalliss S, Garcia E, DeBerardino TM, Cameron KL (2010) The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med 38(1):63–67
Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC (2003) Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med 31(6):831–842
Utzschneider S, Goettinger M, Weber P et al (2011) Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc 19(10):1643–1648
Vacek PM, Slauterbeck JR, Tourville TW et al (2016) Multivariate analysis of the risk factors for first-time noncontact ACL injury in high school and college athletes: a prospective cohort study with a nested, matched case–control analysis. Am J Sports Med 44(6):1492–1501
Wahl CJ, Westermann RW, Blaisdell GY, Cizik AM (2012) An association of lateral knee sagittal anatomic factors with non-contact ACL injury: sex or geometry? J Bone Joint Surg Am 94(3):217–226
Yoo JH, Chang CB, Shin KS, Seong SC, Kim TK (2008) Anatomical references to assess the posterior tibial slope in total knee arthroplasty: a comparison of 5 anatomical axes. J Arthroplasty 23(4):586–592
Zelisko JA, Noble HB, Porter M (1982) A comparison of men’s and women’s professional basketball injuries. Am J Sports Med 10(5):297–299
Zeng C, Cheng L, Wei J, Gao S, Yang T, Luo W, Li Y, Xu M, Lei G (2014) The influence of the tibial plateau slopes on injury of the anterior cruciate ligament: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 22:53–65
Zhang Y, Wang J, Xiao J et al (2014) Measurement and comparison of tibial posterior slope angle in different methods based on three-dimensional reconstruction. Knee 21(3):694–698
Author information
Authors and Affiliations
Contributions
AS participated in the design of the study, acquisition and interpretation of the data. SS helped to evaluate the inter-observer reliability. RM helped to translate the manuscript in English and revising it critically for important intellectual content. SL have given final approval of the version to be published. PN have given final approval of the version to be published. ES have made substantial contribution to conception, design of the study and have given final approval of the version to be published.
Corresponding author
Ethics declarations
Funding
No external source of funding was used.
Conflict of interest
AS, SS, RM, SL, PN and ES: no competing interests.
Ethical approval
This study was approved by our institutional review board.
Informed consent
Patients gave informed consent that data would be published.
Rights and permissions
About this article
Cite this article
Schneider, A., Si-Mohamed, S., Magnussen, R.A. et al. Tibiofemoral joint congruence is lower in females with ACL injuries than males with ACL injuries. Knee Surg Sports Traumatol Arthrosc 26, 1375–1383 (2018). https://doi.org/10.1007/s00167-017-4756-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4756-7