Abstract
Purpose
The purpose of this study was to determine the most reliable radiographic measurement method to evaluate PTS as a risk factor for ACL reconstruction failure.
Methods
Patients who underwent ACL reconstruction or ACL revision reconstruction between January 2009 and December 2014 by a single surgeon were included. Fifty-two consecutive patients who underwent ACL revision reconstruction were compared to a random selection of 52 patients who underwent primary ACL reconstruction and a control group of 52 patients without ACL injury. ACL reconstruction was performed using either ipsilateral (primary) or contralateral (revision) quadrupled hamstring autograft. Lateral knee radiographs were evaluated using three methods: (1) longitudinal axis, (2) anterior tibial cortex axis, and (3) posterior tibial cortex.
Results
A significant difference was found between subjects who underwent ACL reconstruction and control knees (6.79° vs. 5.31°, p = 0.046) using the posterior tibial cortex method. No other statistical significance was found between groups. A multiple linear regression analysis found that the PTS as measured by any method was not affected by the patient’s age, sex, height, weight, and BMI. All methods of measurement for PTS demonstrated excellent (ICC > 0.90) intra-rater and inter-rater reliability, but only the posterior tibial cortex method maintained excellent intra-rater and inter-rater reliability (ICC > 0.90) when evaluating patients with ACL revision reconstruction.
Conclusions
The posterior tibial cortex measurement is the most reliable method for analyzing the PTS on lateral knee radiographs in patients undergoing ACL revision reconstruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite significant research and interventions, non-contact anterior cruciate ligament (ACL) tears remain common athletic injuries, leading investigators to identify risk factors that may predispose athletes to injury [1]. Only by understanding the factors leading to injury may successful injury prevention algorithms be developed. Risk factors are commonly classified into four categories: environmental, neuromuscular, hormonal, and anatomical [2]. While anatomy may be difficult to modify, identifying these factors may lead to more aggressive prevention regimens for athletes found to be at highest risk.
Studies have investigated various osseous morphologic characteristics as they relate to anterior cruciate ligament (ACL) injury, including notch width, Q angle, lateral femoral condyle ratio, and posterior tibial slope [3, 4]. Posterior tibial slope (PTS) is a non-modifiable anatomic risk factor that has received attention in recent years. The ACL functions to prevent anterior tibial translation of as well as rotational forces on the knee [5]. Therefore, increased anterior tibial translation of the knee joint places strain on the ACL. Dejour et al. [6] demonstrated that for every 10° increase in posterior inclination of the tibial plateau, there was a 6-mm increase in anterior tibial translation. In a 20-year follow-up of patients who underwent ACL reconstruction, Salmon et al. [7] reported that a PTS of 12° or more was the strongest predictor of ACL reconstruction failure.
The methods of analyzing posterior tibial slope vary throughout the literature, including the use of radiographs versus magnetic resonance imaging (MRI) [8]. The definition of an “at-risk” posterior tibial slope is, therefore, inconsistent and variable based upon the method of measurement. The purpose of this study is to determine the most reliable radiographic measurement method to evaluate posterior tibial slope (PTS) as a risk factor for ACL reconstruction failure.
Materials and methods
Patients who underwent ACL reconstruction or ACL revision reconstruction between January 2009 and December 2014 by a single senior orthopaedic surgeon at our institution were included in this retrospective study. Primary and revision reconstruction were performed using an anatomic intraarticular ACL reconstruction technique with ipsilateral (primary) or contralateral (revision) quadrupled hamstring autograft.
Primary inclusion criteria were noncontact, isolated, complete rupture of the ACL (verified by Arthroscopy, MRI, physical examination).
Fifty-six consecutive patients who underwent ACL revision reconstruction with a minimum four year follow up without the need of further knee were included in the analysis (group I); however, four were lost to follow-up, leaving 52 patients available for inclusion in this study. A second group (group II) consisted of 52 randomly selected patients who underwent primary ACL reconstruction during the study time frame and had a minimum four year follow-up without evidence of graft failure. The third group (group III) was a control group consisting of 52 randomly selected patients who had obtained knee radiographs during this time period for other medical reasons and had no clinical evidence of ACL incompetency.
Exclusion criteria were a history of osteoarthritis or rheumatoid arthritis, history of knee surgery like tibial osteotomy and previous fracture except for ACL reconstruction, BMI > 29, age over 50 years, severe associated ligamentous injuries, Outerbridge 3 or 4 cartilage damage, or lateral radiograph of the knee with less than 10 cm of tibia.
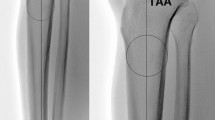
All patients underwent the knee series of radiographs taken to investigate tibial slope. It usually comprises an AP and lateral projection. The lateral knee view is an orthogonal view of the AP view of the knee. The patient is lying on side of interest with the knee of interest closest to the table and the other lower limb rolled anteriorly. Affect knee is flexed approximately 20–30° and tibial is in neutral rotation. The lateral knee radiograph for each subject was evaluated by two independent orthopaedic surgeons. Three techniques for posterior tibial slope measurement were performed on all subjects: (1) longitudinal axis, as described by Hashemi et al. [9]; (2) anterior tibial cortex axis, as described by Chung et al. [10]; and (3) posterior tibial cortex, as described by Hohmann et al. [11] (Fig. 1). Measurements were performed on dedicated digital radiology software (Centricity Imaging PACS/AW Suite, GE Healthcare IT, Chicago, IL, USA) and corrected for magnification.
Three techniques for posterior tibial slope measurement: a Longitudinal axis as described by Hashemi is defined by 2 points situated at a distance midway between anterior and posterior cortex with 1 point in the lower part of the anterior tibial tuberosity and the other 10 cm below it [9]; b anterior tibial cortex axis as described by Chung is defined as line drawn over the anterior border of tibial cortex axis [10]; and c posterior tibial cortex as described by Hohmann is defined as line drawn over the posterior border of tibial cortex axis [11]
A power analysis was performed using the following parameters: a posterior tibial slope difference of 1.34, power of 0.10, and alpha error 0.05. A sample size of 52 subjects was found to be sufficient to detect a difference between groups. Measurements were evaluated by applying the two-tailed paired Student’s t test. A multiple linear regression analysis was performed comparing posterior tibial slope to patient demographics (SPSS 17.0, SPSS, Chicago, IL, USA). Inter-rater and intra-rater reliability was assessed using intraclass correlation (ICC) for each test in each group. A score of greater than 0.70 was considered good, and a score of greater than 0.90 was considered excellent (Stata 14.2, College Station, TX). This study was approved by the institutional ethics committee. Informed consent was obtained from all individual participants included in the study.
Results
A total of 156 subjects were included in the study. Group I consisted of 52 ACL revision reconstructions, average age 28.8 years (17 females, 35 males). Group II included 52 primary ACL reconstructions, average age 27.9 years (20 females, 32 males). Group III was comprised of 52 healthy knees, average age 30.1 years (16 females, 36 males). No significant differences were found between the groups I and II compared to control group III in terms of age, weight, height, BMI, and injury site (Table 1). The most common activities leading to ACL injury in group I and group II were soccer, basketball, and skiing.
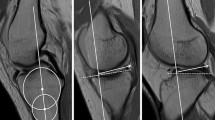
The mean posterior tibial slope for each group is shown in Fig. 2. Using the posterior tibial cortex method described by Hohmann et al. [11], a significant difference was found between subjects who underwent ACL reconstruction (group II) and control knees (group III) (6.79° vs. 5.31°, p = 0.046). No other statistical significance was found between those who underwent ACL revision reconstruction, ACL reconstruction, or control using any method. A multiple linear regression analysis found that the posterior tibial slope as measured by any method was not affected by the patient’s age, sex, height, weight, and BMI.
Posterior tibial slope measurements utilizing three methods. Results are reported as mean + standard deviation. A significant difference (p < 0.05) was found only between groups II and III using the posterior tibial cortex method. No significant differences were found when comparing groups I, II, and III the longitudinal axis or anterior tibial cortex methods
All methods of measurement for posterior tibial slope demonstrated excellent (> 0.90) intra-rater and inter-rater reliability (Table 2). However, when comparing each group separately, only the posterior tibial cortex method of Hohmann et al. [11] maintained excellent intra-rater and inter-rater reliability for both revision ACL and primary ACL patients (Table 3). The longitudinal axis method of Hashemi et al. [9] and the anterior tibial cortex method of Chung et al. [11] did not achieve excellent intra-rater and inter-rater reliability in patients who had undergone revision ACL reconstruction (group I) (Table 3).
Discussion
The posterior tibial cortex measurement is the most reliable method for analyzing the posterior tibial slope on lateral knee radiographs in patients undergoing ACL revision reconstruction. This could be because of the presence of the tibial tuberosity of the anterior tibial cortex regarding the method described by Chung. Regarding the longitudinal axis, as described by Hashemi, it is necessary to take into consideration a greater number of anatomical landmarks which can determine a greater error rate. But we have to admit that all the three methods were affected by the length of the proximal tibial bone.
However, in our cohort of patients, the posterior tibial slope of patients who underwent ACL reconstruction and revision reconstruction were not significantly different from patients with no previous ACL injuries. Only one measurement method found a significant difference of 1.48° between patients who underwent ACL reconstruction and controls, but the clinical significance of this measurement is unclear. No differences were found between patients who underwent ACL reconstruction and those who underwent ACL revision reconstruction. Posterior tibial slope therefore may not be a risk factor for ACL revision reconstruction in this patient cohort.
Currently, there is no consensus regarding the measurement method for posterior tibial slope, including the use of lateral radiograph versus magnetic resonance imaging [8]. In this study, we evaluated three methods that have been described in the literature to determine posterior tibial slope. All measurement techniques had good to excellent intraclass correlation coefficients, but only the posterior tibial cortex method of Hohmann et al. [11] was found to retain excellent intra- and inter-rater reliability for group I, patients who had undergone ACL revision reconstruction. In contrast, a study performed by Zeng et al. [12] previous reported that the longitudinal measurement technique for posterior tibial slope was the most reliable in patients who were undergoing primary ACL reconstruction (longitudinal axis, 0.928 intra-rater, and 0.898 inter-rater reliability versus posterior tibial cortex, 0.916 intra-rater and 0.871 inter-rater reliability). Our data similarly found higher intra-rater and inter-rater reliability for the longitudinal axis method versus the posterior tibial cortex method for patients undergoing primary ACL reconstruction (Table 3). However, in patients who underwent revision ACL reconstruction, the intra-rater and inter-rater reliability was higher for the posterior tibial cortex method versus the longitudinal axis method (intra-rater, 0.977 and inter-rater, 0.939 versus intra-rater 0.958 and inter-rater 0.773, respectively). Therefore, the posterior tibial cortex method of measuring posterior tibial slope should be considered when utilizing lateral knee radiographs to determine posterior tibial slope in patients with ACL deficiency and, specifically, in patients with ACL graft failure (Table 3).
A plethora of research has been performed both clinically and biomechanically to identify anatomic risk factors of noncontact ACL failure and subsequent graft failure or contralateral ACL failure [13, 14]. By identifying those athletes at higher risk, ACL tear prevention programs and patient-specific counseling regarding risk of injury may be individualized. However, the measurement techniques for similar structures vary within the published literature. Several methods of measuring PTS have been described using either standard lateral radiograph or MRI, with conflicting results. Previous reports state that posterior tibial slope may be considered excessive when the PTS is measured to be greater than 12° [5, 14,15,16]. This has led to the use of high tibial osteotomies to alter anatomic variations that may place excess stress on the ACL reconstruction graft [17]. A meta-analysis and systematic review performed by Wordeman et al. in 2012 [8] reviewed the literature for studies that compared posterior tibial slope in ACL-injured groups and control groups using MRI or radiographic measurement techniques. In their study, they found that almost all studies found a higher posterior tibial slope in patients with ACL rupture; however, the amount of posterior tibial slope that places a patient “at risk” was inconsistent between studies. As shown in this study and in previous reports, the measurement method can significantly alter this numerical value.
In an attempt to quantify the interaction of the medial and lateral tibial slope as well as the coronal plane alignment and contribution of soft tissues to these measurements, authors have utilized MRI measurement techniques [18,19,20,21]. While Elmansori et al. [18] and Hudek et al. [20] did not find a significant difference in these MRI parameters in patients with ACL injury and those without, Grassi et al. [19] determined that patients who had recurrent ACL tears had significantly steeper posterior tibial slope than patients with a single ACL reconstruction and a control group. Patients with recurrent ACL tears may need to be analyzed separately in order to determine potential anatomic risk factors.
Recently, biomechanical testing has attempted to further quantify the effect of posterior tibial slope on anterior tibial translation and its effect on graft strain. Bates et al. [22], who measured posterior tibial slope using MRI, found that sagittal and coronal tibial slope measurements did not account for peak ACL strain prior to graft failure in a cadaveric specimen. However, Bernhardson et al. [23] measured posterior tibial slope radiographically and found that tibial slope had independently significant effect on graft force in a cadaveric knee specimen. Furthermore, Imhoff et al. [24] utilized cadaveric knee specimens with the highest measured posterior tibial slope on computer tomography (CT) scan and measured the effect of a slope reducing osteotomy to anterior tibial translation in ACL deficient and ACL reconstructed knees. They found that slope reducing osteotomies of 10° significantly reduced anterior tibial translation in ACL deficient knees and significantly reduced graft forces on the ACL graft under axial loading.
Dejour et al. in two reports [25, 26] found that patients who had undergone ACL reconstruction and had an increased posterior tibial slope, as measured on a lateral radiograph, has increased anterior tibial translation on standing lateral knee radiograph. Furthermore, in those patients with ACL reconstruction and medial meniscectomy, posterior tibial slope additional increased anterior tibial translation on stress radiography. Strain on the ACL graft, as measured by the anterior tibial translation, may not only be affected by posterior tibial slope but a combination of anatomic factors and loss of secondary stabilizers may put patients at risk for further ACL graft failure.
A recent report by Salmon et al. [7] examined the 20-year follow-up clinical outcomes in patients who had undergone ACL reconstruction, with 90% follow-up. Patients who were < 18 years old at the time of surgery with a posterior tibial slope of > 12° were 11 times more likely to rupture the ACL graft and 7 times more likely to rupture the contralateral graft than those > 18 years old with tibial slopes < 12°. Furthermore, patients > 18 years old with a posterior tibial slope of > 12° were 7 times more likely to rupture the contralateral ACL. Identifying these individuals pre-operatively with a reliable measurement of the posterior tibial slope may allow surgeons to counsel them about their post-operative course and potentially consider procedures such as a high tibial osteotomy for those at risk and desiring to return to sport.
This study attempted to identify reliable radiographic measurements of the posterior tibial slope using three measurements reported in the literature. In comparison to previous studies, we attempted to identify differences in posterior tibial slope for patients who had multiple ACL injuries, primary ACL injury, and patients without ACL injury. Three common measurements for posterior tibial slope using the lateral radiograph were compared, and measurements demonstrated very good to excellent intra- and inter-rater reliability (> 0.9 overall). The main limitation of this study is the retrospective design. Secondly, this study does not correlate how posterior tibial slope change affects knee biomechanics and clinical evaluation. Confounding factors such as contact versus noncontact injuries, the prior method of reconstruction for patients who underwent ACL revision reconstruction was not included in the analysis. Furthermore, the patients included in the primary ACL reconstruction (group II) and control (group III) may have unknown clinical difference from the entire group as they were not selected in continuity as with those who underwent ACL revision reconstruction (group I). Due to the use of lateral radiographs, we were unable to distinguish the bony medial and lateral tibial slope or the meniscal lateral and medial tibial slope for comparison, as can be possible using MRI measurement techniques. We were able to identify a single measurement that allowed for a more reliable measurement of the posterior tibial slope. Furthermore, while clinically significant differences in posterior tibial slope between the cohorts in this study were not found, we propose that future studies identify patients with multiply injured ACL and contralateral ACL tears as a separate cohort when evaluating anatomic variables related to the risk of ACL tear.
Conclusions
Investigators should consider utilizing the posterior tibial cortex measurement method when analyzing the posterior tibial slope on lateral knee radiographs, but the use of posterior tibial slope as a risk factor for ACL rupture and reconstruction failure should be considered with caution. In our cohort, the posterior tibial slope measurement was not found to be associated with incidence of ACL revision reconstruction when compared to patients undergoing primary ACL reconstruction, and a control patient population without ACL injury even if a significant difference was found between primary ACL reconstruction and control group using the posterior tibial cortex method.
References
Yang XG, Wang F, He X et al (2020) Network meta-analysis of knee outcomes following anterior cruciate ligament reconstruction with various types of tendon grafts. Int Orthop 44(2):365–380. https://doi.org/10.1007/s00264-019-04417-8
Napier RJ, Garcia E, Devitt BM, Feller JA, Webster KE (2019) Increased radiographic posterior tibial slope is associated with subsequent injury following revision anterior cruciate ligament reconstruction. Orthop J Sports Med 7(11):2325967119879373. https://doi.org/10.1177/2325967119879373
Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF (2006) The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 22(8):894–899
Hashemi J, Chandrashekar N, Gill B et al (2008) The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am 90(12):2724–2734
Feucht MJ, Mauro CS, Brucker PU, Imhoff AB, Hinterwimmer S (2013) The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 21(1):134–145
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg (Br) 76(5):745–749
Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA (2018) 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med 46(3):531–543
Wordeman SC, Quatman CE, Kaeding CC, Hewett TE (2012) In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury. Am J Sports Med 40(7):1673–1681
Hashemi J, Chandrashekar N, Mansouri H et al (2010) Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38(1):54–62
Chung SC-Y, Chan W-L, Wong S-H (2011) Lower limb alignment in anterior cruciate ligament–deficient versus –intact knees. J Orthop Surg 19(3):303–308
Hohmann E, Bryant A, Reaburn P, Tetsworth K (2010) Does posterior tibial slope influence knee functionality in the anterior cruciate ligament–deficient and anterior cruciate ligament–reconstructed knee? Arthrosc J Arthrosc Relat Surg 26(11):1496–1502
Zeng C, Yang T, Wu S et al (2016) Is posterior tibial slope associated with noncontact anterior cruciate ligament injury? Knee Surg Sport Traumatol Arthrosc 24(3):830–837
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32(2):376–382
Cavaignac E, Pailhé R, Reina N, Murgier J, Laffosse JM, Chiron P, Swider P (2016) Can the gracilis replace the anterior cruciate liga- ment in the knee? A biomechanical study. Int Orthop 40(8):1647–1653
Dejour D, Saffarini M, Demey G, Baverel L (2015) Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc 23(10):2846–2852
Sonnery-Cottet B, Mogos S, Thaunat M et al (2014) Proximal tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med 42(8):1873–1880
Robin JG, Neyret P (2016) High tibial osteotomy in knee laxities: concepts review and results. EFORT Open Rev 1(1):3–11
Elmansori A, Lording T, Dumas R, Elmajri K, Neyret P, Lustig S (2017) Proximal tibial bony and meniscal slopes are higher in ACL injured subjects than controls: a comparative MRI study. Knee Surg Sport Traumatol Arthrosc 25(5):1598–1605
Grassi A, Macchiarola L, Urrizola Barrientos F et al (2019) Steep posterior tibial slope, anterior tibial subluxation, deep posterior lateral femoral condyle, and meniscal deficiency are common findings in multiple anterior cruciate ligament failures: an MRI case-control study. Am J Sports Med 47(2):285–295
Hudek R, Fuchs B, Regenfelder F, Koch PP (2011) Is noncontact ACL injury associated with the posterior tibial and meniscal slope? Clin Orthop Relat Res 469(8):2377–2384
Suprasanna K, Chamala T, Kumar A (2019) Comparison of anatomical risk factors for noncontact anterior cruciate ligament injury using magnetic resonance imaging. J Clin Orthop Trauma 10(1):143–148
Bates NA, Mejia Jaramillo MC, Vargas M, McPherson AL, Schilaty ND, Nagelli CV, Krych AJ, Hewett TE. (2019) External loads associated with anterior cruciate ligament injuries increase the correlation between tibial slope and ligament strain during in vitro simulations of in vivo landings. Clin Biomech, Bristol, Avon 61:84–94. https://doi.org/10.1016/j.clinbiomech.2018.11.010.
Bernhardson AS, Aman ZS, Dornan GJ et al (2019) Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med 47(2):296–302
Imhoff FB, Mehl J, Comer BJ et al (2019) Slope-reducing tibial osteotomy decreases ACL-graft forces and anterior tibial translation under axial load. Knee Surg Sports Traumatol Arthrosc 27(10):3381–3389. https://doi.org/10.1007/s00167-019-05360-2
Dejour D, Pungitore M, Valluy J, Nover L, Saffarini M, Demey G (2019) Preoperative laxity in ACL-deficient knees increases with posterior tibial slope and medial meniscal tears. Knee Surg Sport Traumatol Arthrosc 27(2):564–572. https://doi.org/10.1007/s00167-018-5180-3
Dejour D, Pungitore M, Valluy J, Nover L, Saffarini M, Demey G (2019) Tibial slope and medial meniscectomy significantly influence short-term knee laxity following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 27(11):3481–3489. https://doi.org/10.1007/s00167-019-05435-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Level III. Study Design: Retrospective case-control study
Rights and permissions
About this article
Cite this article
Gaj, E., Monaco, E., De Carli, A. et al. Measurement technique for posterior tibial slope on radiographs can affect its relationship to the risk of anterior cruciate ligament rupture. International Orthopaedics (SICOT) 45, 1469–1475 (2021). https://doi.org/10.1007/s00264-020-04865-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04865-7