Abstract
Purpose
The primary goal was to describe the injury patterns in a population of primary (first time) lateral patellar dislocators (LPD) to lend clarity to commonly held notions about injury patterns in this population.
Methods
A prospective study identifying patients presenting with LPD between 2008 and 2012. Inclusion criteria were a history and physical exam consistent with primary LPD, and an MRI consistent with the diagnosis without other significant ligamentous injury. On MRI, location of cartilage, medial patellofemoral ligament (MPFL) injury, and bone bruising were noted. Severity was categorized as partial or complete for MPFL and cartilage lesions. Anatomic patellar instability risk factors (patella alta, trochlear dysplasia, increased TT-TG, and lateral patella tilt) were recorded and compared to the injury patterns.
Results
This study involved 157 patients; 107 patients were skeletally mature. Of the 157 patients, 26 had surgery for this injury due to clinician-perceived need for cartilage debridement. MPFL injury severity was complete rupture (N = 69, 44%), partial (N = 67, 43%), and none (N = 19, 13%). MPFL injury location was isolated femoral (N = 16, 10%), isolated patella (N = 26, 17%), isolated mid-substance (0%), multiple locations (N = 95, 61%), and none (N = 20, 13%). Chondral injury location was patella (N = 67, 43%), lateral femoral condyle (N = 11, 7%), multiple locations (N = 53, 34%), and none (N = 26, 17%). A majority (61%) of patellar chondral lesions were at its inferomedial aspect; all medial patellar retinacular partial injuries involved the inferomedial aspect of the patella, consistent with the insertion of the medial patellotibial ligament (MPTL). Skeletally immature patients had a greater risk of isolated patellar MPFL and chondral injury. No clear relationship was found between/across the location and/or severity of bone bruising, MPFL, or chondral injury.
Clinical relevance
Underlying anatomic patellar instability risk factors defined by MRI, do not predict injury patterns. MPFL and chondral injury, as well as bone bruising, are common following LPD. The medial patellotibial ligament is torn in patellar-based medial retinacular injuries, based on MRI injury location. Skeletal immaturity plays a role in the location of the injury pattern with isolated patellar-based MPFL/chondral injury being more common in the skeletally immature patient. Sex does not appear to be a factor in injury patterns after primary LPD. Knowledge of these injury trends will help focus the clinician in injury evaluation when managing primary patellar dislocations.
Level of evidence
Case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral patellar dislocation (LPD) often causes injury to structures within the patellofemoral joint [20, 31]. Key areas of injury include the medial patellofemoral ligament (MPFL), as well as cartilage and bone on the patella and/or trochlea [19, 37, 42]. Dysfunction of the knee can result from injury to these structures [39]. If the MPFL remains insufficient, recurrent patellar dislocations are more likely [9, 14, 34]. With recurrent instability episodes, the risk of cartilage and bone injury increases [31, 33]. Damage to cartilage can lead to early-onset degenerative changes and, eventually, symptoms that coincide with arthritis [12, 24, 37, 39]. This can have significant impact on quality of life for young active patients, which is a major complaint of patellar instability patients. Managing primary (first-time) LPD to limit recurrence is important; part of managing these patients is understanding primary LPD injury patterns.
Previous studies evaluating injury patterns in patellar instability patients have demonstrated that MPFL and osteochondral injury is common [1, 6, 15, 16, 20, 36, 40]. More recently, studies have looked at the site of MPFL injury: patella, interstitial, femur, or a combination of those sites [3, 7, 17, 22, 23, 42, 43]. Knowing the location is important because the rate of redislocation is higher when there is an isolated femoral lesion [22, 35] and acute repair may fare better when the lesion is solely patella based [10, 11].
Injury patterns have been evaluated based on age. Most reports suggest the patella is the most common site of MPFL injury in children [3, 17, 23, 27, 32]. Studies have also evaluated the extent and location of osteochondral injury [32, 37, 41–43]. Few studies, however, have evaluated the full injury pattern based on sex or by age, as defined by bony maturity.
The primary goal of this study was to describe the injury patterns in a population of primary (first time) lateral patellar dislocators (PLPD) to evaluate the following hypotheses reflective of commonly held notions:
-
Patients with a greater number of underlying anatomic risk factors for patellofemoral instability will have less chondral damage.
-
Skeletally immature patients have more MPFL patellar-based lesions.
-
Bone bruising infers higher forces and is associated with greater cartilage damage.
-
Injury patterns in primary LPD are not different between the sexes.
Materials and methods
Approval was obtained from our institutional review board prior to initiation of this study. Consecutive patients with a history of LPD between 2008 and 2012 were prospectively identified from two musculoskeletal outpatient clinics.
Inclusion criteria for the study were:
-
A history and physical exam consistent with primary LPD [2, 5, 18].
-
An MRI consistent with this diagnosis obtained within 6 weeks of the initial injury.
Exclusion criteria included previous instability event, injury to other ligaments of the knee beside the MPFL, and previous surgery in the index knee.
The injury location and severity for MPFL and chondral injury, as well as the bone bruising, were described for the entire patient cohort. Stratification was performed based on sex and skeletal maturity, defined as open vs. closed physes. It was also documented as to whether the patients underwent surgery for chondral debridement following their PLPD event.
In an attempt to further define injury patterns, injury location and severity was compared with underlying anatomic risk factors as defined by patella alta, trochlear dysplasia, tibial tubercle-trochlear groove (TT-TG) distance, and patellar tilt. The measurement of these risk factors on MRI has been described in a previous study [2]. The thresholds for surgical intervention as defined by Dejour et al. were used to define “excessive” measurements (CD >1.2, TT–TG > 20 mm, tilt > 20°) [13]. Trochlear depth <3 mm was chosen to define trochlea dysplasia as reported by Pfirrmann et al. [28]. The number of excessive measurements within each of the four measurements was tabulated by individual patient to represent how many underlying anatomic risk factors for instability were present, a ‘four-factor’ analysis. These numbers were then compared to the injury pattern data.
In addition, specific attention was given to MPFL imaging injury patterns to assess:
-
1.
Associated injury to the medial collateral ligament (MCL), and
-
2.
The location of the medial retinacular injury on the patella
MRI interpretation
MRI was performed on either 1.5 or 3 T magnets. All MRIs were evaluated for injury to the MPFL, chondral injury, and bone bruising. Location of the MPFL injury was classified as either patella, femur, mid-substance, combination lesion, or no lesion. Severity of MPFL injury was defined as no injury, partial rupture, or complete rupture [3]. Partial rupture by MRI was defined as extending less than 50% of the total vertical length of the medial retinaculum attachment to the patella or <2 cm, as previously described [3, 4]. Location of chondral lesions were classified as patella, lateral femoral condyle, combined lesion, or no lesion. Severity of chondral lesion was defined as full thickness, partial thickness, or none. As a marker of chondral injury severity, the need for surgical debridement was noted. Bone bruising was defined by location and divided into patella, lateral femoral condyle, combined lesion, no lesion, or other which included bruising in other locations of the knee. MRIs were also used to determine skeletal maturity; patients with open physes were classified as skeletally immature while patients with closing or closed physes were classified as skeletally mature [2, 4, 25].
A fellowship-trained musculoskeletal radiologist interpreted the injury patterns on all MRI. Consensus was arrived at to ensure that radiology and orthopaedic terminology were aligned between the musculoskeletal fellow-trained radiologist and the senior sports medicine fellowship trained orthopaedic surgeon; in particular, partial ‘MPFL’ tears were reviewed by the radiologist and orthopaedic surgeon with consensus on location and length of the patellar-based injury. Intra- and inter-observer methodology for each of the anatomic measurements taken from the MRI scan can be referred to in a previous paper [2].
Institutional Review Board (IRB) approval was obtained from the IRB (study number 1005E82296) prior to initiation of this study.
Statistical analysis
Data were analysed using SPSS (version 21 IBM) for the descriptive statistics. Chi-square tests were used to compare the injury factors based on sex, skeletal maturity, and the ‘four-factor’ analysis. Statistical significance was set at p < 0.05.
Results
This study involved 157 patients: 79 males and 78 females. A total of 107 patients were skeletally mature (46 M/61 F; mean age 23 years, SD ± 9.5, range 11–50) and 50 were skeletally immature (33 M/17 F; mean age 14.3 years, SD ± 1.4, range 10–17). Of the 157 patients, 26 (17%) had surgery for their injury due to clinician-perceived need for cartilage debridement.
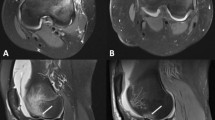
MPFL injury severity was complete rupture (N = 69, 43.9%), partial (N = 67, 42.7%), and no injury (N = 19, 12.8%). All ‘partial’ patellar-based ruptures were located on the inferior medial patella (Fig. 1a–c). MPFL injury location was isolated femoral (N = 16, 10.2%), isolated patella (N = 26, 16.6%), isolated mid-substance (0%), multiple locations (N = 95, 60.5%), (Fig. 2) and no injury (N = 20, 12.7%). In the sub-group of open growth plates (N = 50), MPFL location involved the patella 78% of the time (28% isolated patellar injury, 50% combined with other locations). MPFL injury based on sex and skeletal maturity is displayed in Table 1.
a An axial MRI (1.5 T) depicting a patellar-based medial retinacular injury. b A coronal MRI (1.5 T) depicting a “partial” tear of the MPFL. Note the injury just medial to the patellar tendon on the distal–medial aspect of the patellar retinaculum. The solid lines represent patellar tendon; the dotted lines represent the retinacular injury. c. Schematic illustration of a partial medial retinacular tear (black tear line) and a complete medial retinacular tear (grey tear line). MPFL medial patellofemoral ligament, MPTL medial patellotibial ligament
Chondral injury location was patella (N = 67, 42.7%), lateral femoral condyle (N = 11, 7%), multiple locations (N = 53, 33.8%) (Fig. 3), and no injury (N = 26, 16.5%). A majority of lesions on the patella were at the inferomedial aspect of the patella (41/67 = 61%). Chondral injury severity was full thickness (N = 81, 51.6%), partial thickness (N = 50, 31.8%), and no injury (N = 26, 16.6%). When a patella and lateral femoral condyle location were both present, there was a full thickness chondral defect at one or both locations 83% of the time. Chondral injury based on sex and skeletal maturity is displayed in Table 2.
Bone bruising injury location was patella (N = 4, 2.5%), lateral femoral condyle (N = 15, 9.6%), combination injury (N = 127, 80.9%), none (N = 5, 3.2%), and other (N = 6, 3.8%). Bone bruises without chondral damage occurred in 14% of patients with bone bruises. No clear relationship was found between or across the location and/or severity of bone bruising, MPFL or chondral injury. There were no statistically significant findings when location of bone bruising was analysed by sex or skeletal maturity.
When using the ‘four-factor’ analysis, there were no significant findings to suggest there is a relationship between anatomic instability risk factors and MPFL injury location or severity. For severity of chondral injury, there were no significant differences in anatomic risk factors between patients with full thickness vs. patients with non-full thickness cartilage lesions. Based on MRI analysis, no concomitant MCL injury was identified.
Discussion
The most important finding in our paper is that underlying anatomic patellar instability risk factors, as defined by MRI, did not predict injury patterns as defined by the location and severity of MPFL injury, chondral damage, and/or bone bruising. Considering the stated hypotheses, there was no evidence that a greater number of risk factors (more dysplastic anatomy) were associated with lower likelihood of chondral damage. Skeletally immature patients have more isolated MPFL patellar-based lesions than skeletally mature patients, although combined injuries of patella plus other ligament location was the most frequent ligament lesion in skeletally immature patients. There was also no evidence that bone bruising is associated with greater cartilage damage as based on MRI. There was no clear relationship between sex and injury findings.
There is a high incidence of both MPFL and chondral injury centred at the inferomedial aspect of the patella. When looking at the location of the MPFL and chondral injury together, the patellar-based MPFL lesions were always inferomedial on the patella. A detailed review of all patellar-based partial medial retinacular tears revealed an interesting finding. All ‘partial’ ruptures of the medial retinaculum were inferomedial patella, i.e., the retinacular/ligamentous injury began inferior in all lesions and extended proximal. The location of the medial retinacular injury at the inferomedial patella anatomically corresponds to the insertion of the medial patellotibial ligament (MPTL), with or without bony avulsion. For complete tears this injury extended proximally into the region typically defined as the MPFL patellar insertion. The medial retinaculum encompasses both the MPFL and the MPTL. Though the MPTL is defined anatomically [21, 26] and through imaging [38], the injury pattern noted from our study has not been recognized in the radiology literature in regard to the injury location on the patella. The potential role of the MPTL in patellar stabilization merits further investigation.
The location of MPFL injury along its horizontal length is variable in the literature [6, 8, 20, 22, 29, 40]. Data from the current study suggest that the location of MPFL injury is most commonly a combination of locations. This has obvious implications for MPFL repair, suggesting that it may be difficult to successfully repair the ligament if it is injured at multiple sites. When considering skeletally immature patients, current literature suggests that MPFL injury is most often patella-based [3, 17, 23, 27, 32]. The present study supports the patellar-based lesion is most common in the skeletally immature patient both in isolation and as a combination location injury.
Chondral injuries are common, particularly off the medial or inferomedial aspect of the patella, which has been documented in multiple studies [16, 32, 37, 41]. This is consistent with the data in the current study suggesting the highest percentage of chondral injury is on the patella. Despite the high rate of chondral injury (84%), few were felt to be clinically significant enough to benefit from surgery (17% of total). Skeletally immature patients were more likely to have chondral injury isolated to the patella, whereas skeletally mature patients were split between isolated patella and combined lesion location.
The severity of the chondral lesion has been infrequently reported. The data from the current study demonstrate that skeletally immature patients were less likely to have severe (full-thickness) chondral lesions than the mature patients, perhaps due to greater plasticity of tissues in skeletally immature patients. Despite the high percentage of chondral damage in PLPD, few cases were judged clinically to need surgery to address the chondral damage (16.5%).
When evaluating anatomic patellar instability risk factors (‘four-factor’ analysis) and severity of injury, our hypothesis was that patients who have an increased number of risk factors present would have less severe chondral injury damage. The data do not support this hypothesis; the number of underlying anatomic patellar instability risk factors in general does not seem to predict injury patterns. This finding is consistent with one other paper looking at a primary LPD population that found that MPFL tear location (along its horizontal length) did not correlate with underlying anatomy [43].
MCL injury as a concomitant injury was not found in this population, which was previously reported to be as high as 50% in a population of 80 transient patellar dislocation [30]. This study differs from ours in that the population was largely male (83%); additionally, the authors did not define the LPD injury as primary or recurrent.
The strengths of this study are the comprehensive nature of injury pattern analysis: MPFL injury location and severity, chondral injury location and severity, and location of bone bruising, with analysis based on sex and bony skeletal maturity.
Limitations of this descriptive study include the limitations of an imaging-based study, as the description was based solely on MRI.
Knowledge of these injury trends will help focus the clinician in injury evaluation when managing primary patellar dislocations. In particular, knowing the injury pattern and location is useful in the clinical consideration of a repair of the MPFL. Chondral damage as assessed by MRI is often present but not always necessary to treat clinically.
Conclusion
Underlying anatomic patellar instability risk factors, as defined by MRI, do not predict injury patterns. MPFL and chondral injury, as well as bone bruising, are common following PLPD. Skeletal immaturity plays a role in the location of the injury pattern with isolated patellar MPFL and chondral injury being more common in the skeletally immature patient. No clear relationship was found between or across the location and/or severity of bone bruising, MPFL or chondral injury. Sex does not appear to be a factor in PLPD injury patterns. The MPTL is torn in patellar-based medial retinacular injuries, based on MRI injury location.
References
Arai Y, Nakagawa S, Higuchi T, Inoue A, Honjo K, Inoue H, Ikoma K, Ueshima K, Ikeda T, Fujiwara H, Kubo T (2015) Comparative analysis of medial patellofemoral ligament length change pattern in patients with patellar dislocation using open-MRI. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3689-2
Arendt EA, England K, Agel J, Tompkins MA (2016) An analysis of knee anatomic imaging factors associated with primary lateral patellar dislocations. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4117-y
Askenberger M, Arendt EA, Ekstrom W, Voss U, Finnbogason T, Janarv P-M (2016) Medial patellofemoral ligament injuries in children with first-time lateral patellar dislocations: a magnetic resonance imaging and arthroscopic study. Am J Sports Med 44(1):152–158
Askenberger M, Janarv P-M, Finnbogason T, Arendt EA (2017) Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations. Am J Sports Med 45(1):50–58
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C (2000) Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 28(4):472–479
Balcarek P, Ammon J, Frosch S, Walde TA, Schuttrumpf JP, Ferlemann KG, Lill H, Sturmer KM, Frosch K-H (2010) Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity-trochlear groove distance. Arthroscopy 26(7):926–935
Balcarek P, Terwey A, Jung K, Walde TA, Frosch S, Schuttrumpf JP, Wachowski MM, Dathe H, Sturmer KM (2013) Influence of tibial slope asymmetry on femoral rotation in patients with lateral patellar instability. Knee Surg Sports Traumatol Arthrosc 21(9):2155–2163
Balcarek P, Walde TA, Frosch S, Schuttrumpf JP, Wachowski MM, Sturmer KM, Frosch K-H (2011) Patellar dislocations in children, adolescents and adults: a comparative MRI study of medial patellofemoral ligament injury patterns and trochlear groove anatomy. Eur J Radiol 79(3):415–420
Boden BP, Pearsall AW, Garrett WE Jr, Feagin JA Jr (1997) Patellofemoral instability: evaluation and management. J Am Acad Orthop Surg 5(1):47–57
Camanho GL, Viegas AdC, Bitar AC, Demange MK, Hernandez AJ (2009) Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy 25(6):620–625
Christiansen SE, Jakobsen BW, Lund B, Lind M (2008) Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy 24(8):881–887
Conchie H, Clark D, Metcalfe A, Eldridge J, Whitehouse M (2016) Adolescent knee pain and patellar dislocations are associated with patellofemoral osteoarthritis in adulthood: a case control study. Knee 23(4):708–711
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2(1):19–26
Diederichs G, Issever AS, Scheffler S (2010) MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics 30(4):961–981
Dietrich TJ, Fucentese SF, Pfirrmann CWA (2016) Imaging of individual anatomical risk factors for patellar instability. Semin Musculoskelet Radiol 20(1):65–73
Elias DA, White LM, Fithian DC (2002) Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology 225(3):736–743
Felus J, Kowalczyk B (2012) Age-related differences in medial patellofemoral ligament injury patterns in traumatic patellar dislocation: case series of 50 surgically treated children and adolescents. Am J Sports Med 40(10):2357–2364
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32(5):1114–1121
Fox AJS, Wanivenhaus F, Rodeo SA (2012) The basic science of the patella: structure, composition, and function. J Knee Surg 25(2):127–141
Guerrero P, Li X, Patel K, Brown M, Busconi B (2009) Medial patellofemoral ligament injury patterns and associated pathology in lateral patella dislocation: an MRI study. Sports Med Arthrosc Rehabil Ther Technol 1(1):17
Kaleka CC, Aihara LJ, Rodrigues A, de Medeiros SF, de Oliveira VM, de Paula Leite Cury R (2017) Cadaveric study of the secondary medial patellar restraints: patellotibial and patellomeniscal ligaments. Knee Surg Sports Traumatol Arthrosc 25(1):144–151
Kang HJ, Wang F, Chen BC, Zhang YZ, Ma L (2013) Non-surgical treatment for acute patellar dislocation with special emphasis on the MPFL injury patterns. Knee Surg Sports Traumatol Arthrosc 21(2):325–331
Kepler CK, Bogner EA, Hammoud S, Malcolmson G, Potter HG, Green DW (2011) Zone of injury of the medial patellofemoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med 39(7):1444–1449
Koh JL, Stewart C (2014) Patellar instability. Clin Sports Med 33(3):461–476
Mundy A, Ravindra A, Yang J, Adler BH, Klingele KE (2016) Standardization of patellofemoral morphology in the pediatric knee. Pediatr Radiol 46(2):255–262
Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G (2006) Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 14(1):7–12
Petri M, von Falck C, Broese M, Liodakis E, Balcarek P, Niemeyer P, Hofmeister M, Krettek C, Voigt C, Haasper C, Zeichen J, Frosch KH, Lill H, Jagodzinski M (2013) Influence of rupture patterns of the medial patellofemoral ligament (MPFL) on the outcome after operative treatment of traumatic patellar dislocation. Knee Surg Sports Traumatol Arthrosc 21(3):683–689
Pfirrmann CW, Zanetti M, Romero J, Hodler J (2000) Femoral trochlear dysplasia: MR findings. Radiology 216(3):858–864
Putney SA, Smith CS, Neal KM (2012) The location of medial patellofemoral ligament injury in adolescents and children. J Pediatr Orthop 32(3):241–244
Quinlan JF, Farrelly C, Kelly G, Eustace S (2010) Co-existent medial collateral ligament injury seen following transient patellar dislocation: observations at magnetic resonance imaging. Br J Sports Med 44(6):411–414
Saggin PRF, Saggin JI, Dejour D (2012) Imaging in patellofemoral instability: an abnormality-based approach. Sports Med Arthrosc 20(3):145–151
Seeley M, Bowman KF, Walsh C, Sabb BJ, Vanderhave KL (2012) Magnetic resonance imaging of acute patellar dislocation in children: Patterns of injury and risk factors for recurrence. J Pediatr Orthop 32(2):145–155
Siebold R, Karidakis G, Fernandez F (2014) Clinical outcome after medial patellofemoral ligament reconstruction and autologous chondrocyte implantation following recurrent patella dislocation. Knee Surg Sports Traumatol Arthrosc 22(10):2477–2483
Sillanpaa PJ, Maenpaa HM (2012) First-time patellar dislocation: surgery or conservative treatment? Sports Med Arthrosc 20(3):128–135
Sillanpaa PJ, Peltola E, Mattila VM, Kiuru M, Visuri T, Pihlajamaki H (2009) Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men: a mean 7-year nonoperative follow-up study. Am J Sports Med 37(8):1513–1521
Sillanpaa PJ, Salonen E, Pihlajamaki H, Maenpaa HM (2014) Medial patellofemoral ligament avulsion injury at the patella: classification and clinical outcome. Knee Surg Sports Traumatol Arthrosc 22(10):2414–2418
Stanitski CL, Paletta GA Jr (1998) Articular cartilage injury with acute patellar dislocation in adolescents. Arthroscopic and radiographic correlation. Am J Sports Med 26(1):52–55
Thawait SK, Soldatos T, Thawait GK, Cosgarea AJ, Carrino JA, Chhabra A (2012) High resolution magnetic resonance imaging of the patellar retinaculum: normal anatomy, common injury patterns, and pathologies. Skeletal Radiol 41(2):137–148
Tsai C-H, Hsu C-J, Hung C-H, Hsu H-C (2012) Primary traumatic patellar dislocation. J Orthop Surg Res 7:21
Weber-Spickschen TS, Spang J, Kohn L, Imhoff AB, Schottle PB (2011) The relationship between trochlear dysplasia and medial patellofemoral ligament rupture location after patellar dislocation: an MRI evaluation. Knee 18(3):185–188
Zaidi A, Babyn P, Astori I, White L, Doria A, Cole W (2006) MRI of traumatic patellar dislocation in children. Pediatr Radiol 36(11):1163–1170
Zhang G-y, Zheng L, Feng Y, Shi H, Liu W, Ji B-j, Sun B-s, Ding H-y (2015) Injury patterns of medial patellofemoral ligament and correlation analysis with articular cartilage lesions of the lateral femoral condyle after acute lateral patellar dislocation in adults: an MRI evaluation. Injury 46(12):2413–2421
Zhang G-Y, Zheng L, Shi H, Ji B-J, Feng Y, Ding H-Y (2017) Injury patterns of medial patellofemoral ligament after acute lateral patellar dislocation in children: correlation analysis with anatomical variants and articular cartilage lesion of the patella. Eur Radiol 27(3):1322–1330
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Funding
There was no funding for this study.
Ethical Approval
Institutional Review Board (IRB) approval was obtained from the IRB (study number 1005E82296) prior to initiation of this study.
Informed consent
Informed consent was not obtained for this study. This research involved the study of existing data.
Rights and permissions
About this article
Cite this article
Tompkins, M.A., Rohr, S.R., Agel, J. et al. Anatomic patellar instability risk factors in primary lateral patellar dislocations do not predict injury patterns: an MRI-based study. Knee Surg Sports Traumatol Arthrosc 26, 677–684 (2018). https://doi.org/10.1007/s00167-017-4464-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4464-3