Abstract
Purpose
To clarify the effect of the radial tear of the lateral meniscus on the in situ meniscus force and the tibiofemoral relationship under axial loads and valgus torques.
Methods
Ten intact porcine knees were settled to a 6-degree of freedom robotic system, while the force and 3-dimensional path of the knees were recorded via Universal Force Sensor (UFS) during 3 cycles of 250-N axial load and 5-Nm valgus torque at 15°, 30°, 45°, and 60° of knee flexion. The same examination was performed on the following 3 meniscal states sequentially; 33, 66, and 100% width of radial tears at the middle segment of the lateral meniscus, while recording the force and path of the knees via UFS. Finally, all paths were reproduced after total lateral meniscectomy and the in situ force of the lateral meniscus were calculated with the principle of superposition.
Results
The radial tear of 100% width significantly decreased the in situ force of the lateral meniscus and caused tibial medial shift and valgus rotation at 30°–60° of knee flexion in both testing protocols. Under a 250-N axial load at 60° of knee flexion, the in situ force decreased to 36 ± 29 N with 100% width of radial tear, which was 122 ± 38 N in the intact state. Additionally, the tibia shifted medially by 2.1 ± 0.9 mm and valgusrotated by 2.5 ± 1.9° with the complete radial tear. However, the radial tear of 33 or 66% width had little effect on either the in situ force or the tibial position.
Conclusion
A radial tear of 100% width involving the rim significantly decreased the in situ force of the lateral meniscus and caused medial shift and valgus rotation of the tibia, whereas a radial tear of up to 66% width produced only little change. The clinical relevance is that loss of meniscal functions due to complete radial tear can lead to abnormal stress concentration in a focal area of cartilage and can increase the risk of osteoarthritis in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radial tear of the lateral meniscus is a critical injury that commonly occurs among young athletes [21] and often leads to cartilage damage or osteoarthritis change when high-activity level is maintained. Thus, it is important to clarify meniscal function with radial tear in the lateral meniscus because some athletes with this injury unwillingly give up their sports activity.
Load distribution is one of the key meniscal functions. Using film sensors, some studies demonstrated that radial tear of 90–100% of the meniscal width in the lateral meniscus significantly increased the contact pressure in a small cartilage area, whereas a tear of up to 75% of the meniscal width did not [3, 17, 19]. Therefore, radial tear involving the rim could significantly deteriorate meniscal function, while those studies indirectly evaluated the meniscal function via the contact pressure/area in the tibiofemoral joint. It is clinically meaningful to evaluate the in situ force of the meniscus in response to external loads, as well as the contact pressure/area, because it directly correlates with the meniscal function of load distribution when axial compressive loads are applied to the knee. The effect of anterior tibial load on the in situ force of the medial meniscus [2] and that of compressive load on the tensile force of the medial meniscus [15] were previously reported in the anterior cruciate ligament-deficient knees. However, to the best of our knowledge, no previous studies have clarified the effect of radial tear on the in situ force of meniscus under external loads.
Besides load distribution, knee-joint stabilization is another meniscal function. Previous studies showed that varus alignment in the lower extremity was aggravated after arthroscopic medial meniscectomy [23], and varus/external rotational angle and tibial lateral translation significantly increased with complete radial tears at the posterior root of medial meniscus under an axial load [1]. These studies demonstrate that loss of meniscal function could lead to abnormal tibial shift/rotation, causing stress concentration in the abnormal contact area and possibly leading to the initiation of osteoarthritis [9, 14, 22]. However, no studies had investigated the effect of radial tears in the lateral meniscus on the tibiofemoral relationship.
The aim of the present study was to clarify the effect of radial tears of the lateral meniscus on the (1) in situ meniscus force and (2) tibiofemoral relationship under external loads. Our hypothesis was that radial tears involving the rim decreases the in situ force of the lateral meniscus and leads to an abnormal tibiofemoral relationship. This is the first study to clarify the effect of radial tears on in situ forces of the meniscus as well as the tibiofemoral relationship under compressive loads in the same specimen.
Materials and methods
Ten intact fresh frozen porcine knees were used in this study. The pigs were approximately 105 kg in weight with a mean age of 6 months. Specimens with any osteoarthritic changes or ligamentous injuries were excluded. The knees were frozen at −30 °C and thawed at room temperature for 1 day.
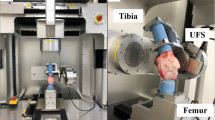
The tibias and femurs were cut 150 mm in length from the joint line. All muscles, including the quadriceps muscle–patella–patellar tendon, were carefully removed from the knee, while the cruciate/collateral ligaments and capsule were left intact. The ends of the femur and tibia were potted in cylindrical molds of acrylic resin (Ostron II; GC Corp, Tokyo, Japan). The fibula was cut 50 mm in length from the proximal tibiofibular joint and fixed to the tibia using acrylic resin to maintain its anatomic position. Subsequently, the femoral and tibial cylinders were fixed to the clamps of the manipulator of a robotic simulator (Fig. 1).
Equipment
The robotic simulator system consisted of a 6-degree of freedom (DOF) manipulator, servo-motor controllers, and a control computer [5, 6]. The femoral clamp was connected to the lower mechanism, while the tibial clamp was fixed to the upper mechanism via a 6-DOF universal force/moment sensor (UFS) (IFS-40E, 15A100-I63-EX; JR3, Inc, Woodland, CA, USA). The six-axis manipulator consisted of three translational actuators (SGMP series, Yaskawa, Fukuoka, Japan) and three rotational actuators (FHA series, Harmonic Drive Systems, Tokyo, Japan). The maximum clamp-to-clamp compliance was 814 N/mm in the proximal–distal direction with the knee extended. The force sensor resolution was 0.01–0.02 N for forces and 0.001 Nm for torques. The test–retest reliability of this robotic system was ±0.006 mm in translation and ±0.03° in rotation for reproducing the paths. Force control fluctuations were under 5 N in force and 0.2 Nm in moment. Thus, this robotic system could apply force/moment to the knee, while controlling the three-dimensional positional displacement and force/moment in natural joint motion without impeding in any directions. The knee joint coordinate system was defined with respect to the non-orthogonal mechanism proposed by Grood and Suntay [8]. To control displacement and force/moment on the knees, a LabView program (LabView version 8.6.1, National Instruments Corp., Austin, TX, USA) was run on a personal computer. Data acquisition was performed at a rate of 17–20 Hz [7].
Test protocols
The knee flexion angle was defined as 15° of flexion with 1 Nm of extension moment because of the intrinsic lag of porcine knees. After a knee was subjected to three cycles of passive extension-flexion between 15° and 120° of knee flexion for preconditioning, the simulator applied (1) an axial load of up to 250 N at a rate of 0.08 mm/s and (2) a valgus moment of up to 5 Nm at a rate of 0.1°/s at 15°, 30°, 45°, and 60° of knee flexion for three cycles. The same test protocols were performed every time after the serial radial sections were created in the middle segment of the lateral meniscus as follows: a radial tear involving (1) one-third width (33%), (2) two-third width (66%), and (3) the whole width (100%) (Table 1) (Fig. 2). Before the creation of radial sections, the knee joint was deeply flexed so that the middle segment of the lateral meniscus could be directly visualized with no damage to the cartilages or soft tissues; three equal parts (33 and 66%) of the meniscal width were then marked using a caliper. All the three cycles of the three-dimensional path of the knee motion and the forces of three directions (fx, fy, fz) to the knee were recorded via UFS. After the test protocols were performed in each meniscal state, the lateral meniscus was totally removed. Then, the simulator reproduced all the identical paths previously acquired under the four meniscal states, including the intact state and the ones with radial tears, while the forces (fx′, fy′, fz′) were also recorded. Based on the principle of superposition [6], the in situ force of the lateral meniscus (F) was calculated and used for evaluations at the third cycle under 50-, 150-, and 250-N axial load and 5-Nm valgus torque:
Accordingly, the in situ force of the meniscus was defined as the resultant force that the meniscus carries in response to a load applied to the knee joint [2] and could be directly correlated with the meniscal function of load distribution when axial compressive loads were applied to the knee.
In addition, the three-dimensional tibial position relative to the femur under 50-, 150-, and 250-N axial load and 5-Nm valgus torque was also evaluated at the third cycle in each meniscal state.
Study approval
The study protocol received the approval of the institutional review board of Yukioka Hospital for using cadaveric porcine specimens (ID: 24-4).
Statistical analysis
All statistical tests were performed using JMP software (version 11.0.0; SAS Institute Inc., Cary, NC, USA). Regarding sample size calculation, it was determined that seven knee specimens would be required for the detection of a 54-N change with a SD of ±46 N of the in situ force of the lateral meniscus with 80% power at the 5% level of significance. Thus, the sample size of 10 knee specimens in this study was acceptable for power analysis. A two-factor repeated-measures analysis of variance was used for the factors of flexion angles and meniscal states (radial tear of 33, 66, and 100% width). Post hoc tests for multiple comparisons were performed using the Tukey’s honestly significant difference test, and P < 0.05 was considered statistically significant.
Results
In situ force of lateral meniscus
The in situ force of the lateral meniscus with a radial tear of 100% width was significantly smaller than that in the other three meniscal states at 30°–60° of knee flexion under 150 and 250 N of axial load (Fig. 3). Similarly, under 5-Nm valgus torque, the in situ force of the lateral meniscus with complete radial tear was significantly lower at 30°–60° of knee flexion (Fig. 4), whereas there were no significant differences among the intact and other two meniscal states. There were no interactions between flexion angles and meniscal states in either axial loads or valgus torque.
Tibiofemoral relationship
The tibia shifted medially and rotated valgus with a radial tear of 100% width in both test protocols, and these medial shift and valgus rotation were significantly greater than those with radial tears of 33 and 66% widths at all flexion angles under 50, 150, and 250 N of axial load (Table 2). Similar changes in the tibiofemoral relationship also occurred under a 5-Nm valgus torque (Fig. 5).
Change of the tibial position due to the radial tears of the middle segment in the lateral meniscus under a 5-Nm valgus torque: a medial–lateral shift, b valgus–varus rotation, c anterior–posterior shift d internal–external rotation. 33%/66%/100% RT: lateral meniscus with a radial tear of 33%/66%/100% width in the middle segment. Asterisk Significant difference (P < 0.05)
Discussion
The principal finding of this study was that a radial tear of 100% width involving the rim significantly decreased the in situ force of lateral meniscus and caused medial shift and valgus rotation of the tibia under tibiofemoral compressive loads, whereas a radial tear of up to 66% width did not produce any significant changes.
Meniscus has important roles in knee joint, such as lubrication, stabilization, and load distribution. Once the meniscus is injured, the other knee structures, including the articular cartilage, may be affected because of impairment of these functions. According to the previous human cadaveric reports, a radial tear of 90–100% width in the lateral meniscus significantly increased the contact pressure between the femur and tibia with the decrease of contact area using a film sensor, whereas a radial tear of 60–75% width did not change the contact pressure or area [3, 17, 19].
Measurement of the in situ force of the meniscus is also significant because this force is directly correlated to the meniscal function of load distribution. The present study is the first to investigate the in situ force of the lateral meniscus with radial tears under tibiofemoral compressive loads. The results indicated that the in situ force of the lateral meniscus exhibited a slight change with a radial tear of up to 66% width, but significantly decreased with the radial tear of 100% width at 30°–60° of knee flexion. Thus, it can be concluded that the outer third area plays an important role in load distribution. In a previous study, the radial tear of 100% width completely de-functioned the medial meniscus because little hoop strain of circumferential fiber was recorded under compressive loads [11]. Thus, it can be inferred that meniscus with the complete radial tear functions as just a spacer, intervening in the tibiofemoral compartment, because the in situ force of the lateral meniscus did not completely disappear with a radial tear of 100% width.
A few studies have examined the effect of isolated radial meniscal tears on the tibiofemoral relationship under compressive loads. When the hoop is disrupted with a complete radial tear, the meniscus cannot resist the outward component of the compressive loads and consequently extrudes from the tibial plateau [13, 16, 20]. In a previous study, the external rotational angle and lateral translation of tibia increased under a 1000-N axial load in case of a complete radial tear at the posterior root of medial meniscus [1]. In the present study, a radial tear of 100% width in the lateral meniscus caused valgus rotation and medial shift of the tibia, even under a small axial load of 50 N. Since meniscus functions as a buttress effect against the femoral condyle [1], the tibia shifted medially relative to femur when the outer fibers of the meniscus were destroyed with a complete radial tear. Furthermore, the extrusion of meniscus could be the cause of tibial valgus rotation, because the radial tear site of meniscus might open under compressive loads, consequently decreasing the meniscal thickness. Therefore, the clinical relevance of our study is that a complete radial tear of the meniscus can lead to abnormal stress concentration in an abnormal cartilage area and can increase the risk of osteoarthritis in the future [4, 14, 22].
This study has some limitations. First, porcine cadaveric models were used in this study, while it might have been more clinically applicable to use a human model. However, as most of the human cadaveric knees are acquired from elders and frequently exhibit degenerative changes in their menisci or cartilages, young porcine knees were used in this study to reduce the influence of these qualitative variations. Moreover, porcine and human knees exhibit anatomical similarities [10, 12, 18]. Second, the magnitude of the axial load applied in this study might be small. Nevertheless, a 250-N axial load is equivalent to the load of knee joint when a 100-kg pig stands on its four legs. In addition, the in situ force of the lateral meniscus with a complete radial tear significantly decreased, even under a 150-N axial load (Fig. 3). Therefore, the force/torque applied in this study would be large enough to yield clinically significant findings. Third, there was no evaluation of the relation between the in situ meniscus force and the contact pressure/area in the same specimen. However, our results were quite similar to those of previous studies, showing that a radial tear involving the rim of the lateral meniscus had a detrimental effect on the meniscal function. Moreover, measurement of the in situ meniscus force could directly evaluate the meniscal function of load distribution in response to axial compressive loads, contrary to the previous studies indirectly evaluating the meniscal function via the contact pressure or area. Therefore, the evaluation of the in situ meniscus force using a robotic simulator as well as the contact pressure/area using a film sensor, are clinically important. Fourth, we did not clarify the threshold of radial tear between 66 and 100% width affecting the meniscal function. Clinically, some fibers in the rim remain in many cases of radial meniscal tears involving the rim. However, the results might vary when some fibers in the rim remain in order to create the radial tear of such as 90% width. Thus, in this study, only a radial tear of 100% width was adopted as a large radial tear to avoid variability.
Conclusion
A radial tear of 100% width involving the rim significantly decreased the in situ force of the lateral meniscus and caused medial shift and valgus rotation of the tibia, whereas a radial tear of up to 66% width produced only little change.
References
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am 90(9):1922–1931
Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL (2000) Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res 18(1):109–115
Bedi A, Kelly N, Baad M, Fox AJ, Ma Y, Warren RF, Maher SA (2012) Dynamic contact mechanics of radial tears of the lateral meniscus: implications for treatment. Arthroscopy 28(3):372–381
Defrate LE, Papannagari R, Gill TJ, Moses JM, Pathare NP, Li G (2006) The 6 degrees of freedom kinematics of the knee after anterior cruciate ligament deficiency: an in vivo imaging analysis. Am J Sports Med 34(8):1240–1246
Fujie H, Livesay GA, Fujita M, Woo SL-Y (1996) Forces and moments in 6-DOF at the human joint: mathematical description for control. J Biomech 29:1577–1585
Fujie H, Sekito T, Orita A (2004) A novel robotic system for joint biomechanical tests: application to the human knee joint. J Biomech Eng 126:54–61
Fujie H, Otsubo H, Fukano S, Suzuki T, Suzuki D, Mae T, Shino K (2011) Mechanical functions of the three bundles consisting of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 19(Suppl 1):S47–S53
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105(2):136–144
Hosseini A, Van de Velde SK, Gill TJ, Li G (2012) Tibiofemoral cartilage contact biomechanics in patients after reconstruction of a ruptured anterior cruciate ligament. J Orthop Res 30(11):1781–1788
Jaspers P, Lange A, Huiskes R, van Rens T (1980) The mechanical function of the meniscus experiments on cadaveric pig knee-joints. Acta Orthop Belg 46:663–668
Jones RS, Keene GC, Learmonth DJ, Bickerstaff D, Nawana NS, Costi JJ, Pearcy MJ (1996) Direct measurement of hoop strain in the intact and torn human medial meniscus. Clin Biomech 34:295–300
Joshi MD, Suh JK, Marui T, Woo SL (1995) Interspecies variation of compressive biomechanical properties of the meniscus. J Biomed Mater Res 29(7):823–828
Lerer DB, Umans HR, Hu MX, Jones MH (2004) The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skelet Radiol 33(10):569–574
Li G, Park SE, DeFrate LE, Schutzer ME, Ji L, Gill TJ, Rubash HE (2005) The cartilage thickness distribution in the tibiofemoral joint and its correlation with cartilage-to-cartilage contact. Clin Biomech (Bristol, Avon) 20(7):736–744
Markolf KL, Jackson SR, McAllister DR (2012) Force measurements in the medial meniscus posterior horn attachment: effects of anterior cruciate ligament removal. Am J Sports Med 40(2):332–338
Messner K, Gao J (1998) The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat 193(Pt 2):161–178
Ode GE, Van Thiel GS, McArthur SA, Dishkin-Paset J, Leurgans SE, Shewman EF, Wang VM, Cole BJ (2012) Effects of serial sectioning and repair of radial tears in the lateral meniscus. Am J Sports Med 40(8):1863–1870
Proffen BL, McElfresh M, Fleming BC, Murray MM (2012) A comparative anatomical study of the human knee and six animal species. Knee 19(4):493–499
Schillhammer CK, Werner FW, Scuderi MG, Cannizzaro JP (2012) Repair of lateral meniscus posterior horn detachment lesions: a biomechanical evaluation. Am J Sports Med 40(11):2604–2609
Setton LA, Guilak F, Hsu EW, Vail TP (1999) Biomechanical factors in tissue engineered meniscal repair. Clin Orthop Relat Res 367(Suppl):S254–S272
Terzidis IP, Christodoulou A, Ploumis A, Givissis P, Natsis K, Koimtzis M (2006) Meniscal tear characteristics in young athletes with a stable knee: arthroscopic evaluation. Am J Sports Med 34(7):1170–1175
Van de Velde SK, Bingham JT, Hosseini A, Kozanek M, DeFrate LE, Gill TJ, Li G (2009) Increased tibiofemoral cartilage contact deformation in patients with anterior cruciate ligament deficiency. Arthritis Rheum 60(12):3693–3702
Yoon KH, Lee SH, Bae DK, Park SY, Oh H (2013) Does varus alignment increase after medial meniscectomy? Knee Surg Sports Traumatol Arthrosc 21(9):2131–2136
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This work was supported by a grant from Japan Society for the Promotion of Science, JSPS KAKENHI Grant Number JP26462293.
Ethical approval
This article does not contain any studies with animals performed by any of the authors because all the knee specimen were obtained from the edible pigs of the local butcher.
Rights and permissions
About this article
Cite this article
Tachibana, Y., Mae, T., Fujie, H. et al. Effect of radial meniscal tear on in situ forces of meniscus and tibiofemoral relationship. Knee Surg Sports Traumatol Arthrosc 25, 355–361 (2017). https://doi.org/10.1007/s00167-016-4395-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4395-4