Abstract
Purpose
Medial patellofemoral ligament (MPFL) reconstruction offers good clinical results with a very low rate of instability recurrence. However, its in vivo effect on patellar tracking is not clearly known. The aim of this study is to investigate the effects of MPFL reconstruction on patellar tracking using dynamic 320-detector-row CT.
Methods
Ten patients with patellofemoral instability referred to isolated MPFL reconstruction surgery were selected and subjected to dynamic CT before and ≥6 months after surgery. Patellar tilt angles and shift distance were analysed using computer software specifically designed for this purpose. Kujala and Tegner scores were applied, and the radiation of the CTs was recorded. Two protocols for imaging acquisition were compared: a tube potential of 80 kV and 50 mA versus a tube potential of 120 kV and 100 mA, both with a slice thickness of 0.5 mm and an acquisition duration of 10 s.
Results
There were no changes in patellar tracking after MPFL reconstruction. There was no instability relapse. Clinical scores improved from a mean of 51.9 (±15.6)–74.2 (±20.9) on the Kujala scale (p = 0.011) and from a median of 2 (range 0–4) to 4 (range 1–6) on the Tegner scale (p = 0.017). The imaging protocols produced a dose-length product (DLP) of 254 versus 1617 mGycm and a radiation effective estimated dose of 0.2 versus 1.3 mSv, respectively. Both protocols allowed the analysis of the studied parameters without loss of precision.
Conclusions
Reconstruction of the MPFL produced no improvement in patellar tilt or shift in the population studied. The low-radiation protocol was equally effective in measuring changes in patellar tracking and is recommended. Although the procedure successfully stabilized the patella, knee surgeons should not expect patellar shift and tilt correction when performing isolated patellofemoral ligament reconstruction in patients with recurrent patellar instability.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The medial patellofemoral ligament (MPFL) is the main patellar stabilizer between 0° and 60° of knee flexion [31, 33, 48]. Normal patellar tracking is dependent on bone and soft tissue balance, especially on trochlear anatomy, which is the most important predictor of lateral maltracking [7, 46]. Reconstruction of the medial patellofemoral ligament (MPFL) offers good clinical results [6, 10, 16, 19, 30, 32] with a very low rate of instability recurrence. However, its real in vivo effect on patellar tracking is still not fully known. The anatomical complexity of the patellofemoral joint makes it extremely difficult to isolate the result of a single procedure, considering that trochlear dysplasia, patellar height, and increased Q angle are fundamental to defining patellar tracking and that most patellar instability patients have combined abnormalities of varying degrees.
Most studies that analysed the effect of MPFL reconstruction on the movement of the patella relative to the trochlea were performed on cadavers with normal anatomy and without muscle action [2, 34]. Even in these studies, there is evidence that patellar kinematics are not optimal after MPFL reconstruction with tubular grafts in comparison with the native ligament [33]. The few studies that describe in vivo analyses were conducted without muscle contraction [24] or combined with other techniques such as tibial tuberosity realignment [15]. Furthermore, dynamic biomechanical evaluation is difficult because most imaging is static even with muscle contraction [5, 22, 37].
There is, therefore, no widespread and accepted method that can be used to evaluate the effect of surgical intervention on patellar tracking. Although it is not yet widely used for this purpose, coronary angiography multiple-detector-row tomography [13, 38] allows continuous dynamic analysis of the patellofemoral joint [15].
With the hypothesis that isolated MPFL reconstruction in vivo can improve patellar tracking in patients with recurrent patellar instability and considering that this answer has clinical relevance because most related knowledge is based on cadaveric studies, this work aimed to evaluate the effect of this procedure on patellar kinematics utilizing a dynamic computed tomography protocol for the patellofemoral joint.
Materials and methods
Ten patients with a diagnosis of recurrent patellar instability with at least two dislocations and a history of at least 6 months were included following the subsequent criteria:
-
1.
10–35 years of age;
-
2.
Non-pregnant and not lactating;
-
3.
Presence of laxity of the medial ligamentous stabilizers of the patella;
-
4.
Lack of indication for distal realignment, patellar height correction, trochleoplasty, or corrective osteotomies of the mechanical axis;
-
5.
Lack of prior knee surgeries; and.
-
6.
Lack of patellofemoral arthritis.
The objective was to include only patients with indication for isolated MPFL reconstruction. The presence of laxity of the medial stabilizers was confirmed by a positive apprehension test and the lateralization of the patella relative to the trochlea of more than half of its width [43]. It was especially important to rule out the need for associated surgeries. The indication for distal realignment of the tibial tuberosity (TT) was a tibial tuberosity–trochlear groove distance (TTTG) ≥20 mm [12]. Trochleoplasty was considered whenever lateral radiography showed a Dejour type B or D trochlea [11, 44] with ventral prominence greater than 6 mm [14, 28] and trochlear groove angle greater than 150° [29]. Patellar height correction was indicated when the Caton–Deschamps index exceeded 1.3 [9]. Lateral retinacular release was based on intraoperative impossibility of medializing the patella more than 5 mm from its centred position and the inability of raising its lateral edge [43].
Inclusion was sequentially determined from the hospital surgical waiting list, with nine females and one male by chance. The ages of the patients had a mean of 21.1 and median of 19 years (range 14–34). There were 6 left knees and 4 right knees. Half of the patients had generalized ligamentous laxity according to the Beighton score [3]. All the patients had positive apprehension tests, 7 had positive “J” sign, and all had at least 3 dislocation episodes. The anatomical characteristics of the patients are shown in Table 1 and indicate that most patients had altered patellar tilt and tracking.
The study consisted of dynamic pre-operative CT, surgery, and a second CT 6–12 months later.
MPFL reconstruction was performed according to the method described by Camanho et al. [8] using as graft the medial part of the patellar tendon and securing it to the femur with an anchor, using the parameters described by Schöttle et al. [41]. The fixation of the graft was made by removing its slack without tension with the knee between 30° and 45° of flexion and the patella centred in the trochlea.
Kujala’s [25] and Tegner’s [45] scales were pre-operatively applied and at the time of post-operative CT. The mean follow-up was 10.2 months, with a median of 9 months (range 7–14). Instability recurrence was considered a failure.
The apparatus used was an Aquilion ONE Toshiba Medical Systems CT scanner with 320-detector-row, 0.5-mm-thick collimation, 350 ms X-ray tube rotation and 16 cm z-axis coverage. No previously established image acquisition protocol existed for performing continuous dynamic CT. To move a knee through its range of motion, patients were placed in the supine position with the knee initially flexed at 90° and the back of the thigh supported to form a triangle of 31 × 31 × 36 cm with the knee, leg, and foot free to move against gravity. Patients took 10 s to actively move the knee from 90° of flexion to full extension, allowing the capture of images in continuous motion.
Tomographic parameters were based on the values commonly used in standard knee CT. Due to concerns about radiation in a continuous examination, an alternative protocol was created. The two acquisition protocols were allocated by drawing sealed envelopes. Protocol 1 (higher radiation dose and higher-resolution images) involved in 10 s of acquisition time, 0.5 mm slice thickness, 120 kV tube potential, and 100 mA tube current per slice. The lower radiation protocol 2 differed only in employing 80 kV tube potential and 50 mA tube current per slice. The radiation analysis was performed comparing the effective radiation dose (mSv), which was calculated using a correction factor specific to the anatomical region irradiated (knee, 0.0008 mSv/mGycm). These acquisition protocols generated approximately 20 volumes of sequential images.
Working with 3-dimensional images at different flexion angles required a system for monitoring patellar tracking. A software program was designed to allow the evaluator to manually set three planes on the femur, one plane on the patella, and one point at the patellar centre and to measure the angles and distances between them without the need for 3D reconstruction. The software allowed measurement of the volume flexion angle using a digital goniometer. The standardized planes and points were as follows (Fig. 1):
-
Pxz: the plane tangential to the posterior condyles of the femur, defined on the axial cut in which the intercondylar notch has a Roman arch appearance and identical to the one used for the TTTG measurement [12];
-
Pzy: the plane perpendicular to Pxz, crossing the deepest point of the trochlea (trochlear plane) and identical to the one used for the TTTG measurement [12];
-
Pxy: the axial plane of the femur perpendicular to the Pxz and Pzy planes, tangential to the most distal point of the trochlea (distal trochlea limit);
-
Ppl: defined by the transverse axis of the patella as performed in the patellar tilt measurement [20].
-
pl: the midpoint of the patella, defined as the intersection of the Ppl and its perpendicular passing through the patellar apex. This point is situated at the centre of the patella in both axial and sagittal cuts.
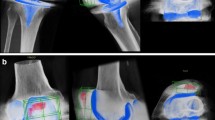
The measurements taken between the planes and the pl point were as follows (Fig. 2):
Angles and distances measured. The positions of the planes in the image have been chosen to illustrate the measured angles and do not correspond to those actually used for the measurements (depicted in Fig 1). The alpha angle described in the text is the angle exceeding 90° of the depicted alpha and represents patellar tilt
-
Alpha angle: angle exceeding 90° from alpha is depicted in Fig. 2 between Ppl and Pzy (this alpha angle represents patellar tilt);
-
Beta angle: between Ppl and Pxz;
-
Gamma angle: between Ppl and Pxy;
-
dx distance: shortest distance between point pl (patella centre) and plane of the trochlea Pzy (this distance represents patellar shift or the degree of lateralization of the patella from the trochlear plane).
The institutional review board (IRB) of the Clinical Hospital of the School of Medicine at the University of São Paulo (Hospital das CLínicas da Universidade de São Paulo) approved the study under the ID number 0357/11.
Statistical analysis
The normality of the data was tested using the Kolmogorov–Smirnov test. The analysis was performed using the paired Student’s t test for normally distributed data or the Wilcoxon test for non-parametric distribution. P < 0.05 was considered statistically significant.
Because different patients actively and freely moved the knee in varying patterns, each volume captured a different flexion angle that varied according to the initial captured knee position, the final extension obtained, and the speed of movement. Because the image volumes generated for each patient had different flexion angles, it was necessary to summarize these measurements into paired intervals. Thus, a mean value of each measure (alpha, beta, and gamma angles and dx distance) was calculated at 10° flexion intervals for each patient.
Although the anatomical referencing used is routine for knee surgeons, the authors decided to analyse the consistency of the data. To that end, the intraclass correlation coefficient (ICC) was used before and after surgery with a 95 % confidence interval by comparing two sets of measurements blindly performed at a 15 day interval. Pre- and post-operatively, respectively, the ICCs were 0.978 and 0.992 for flexion angle, 0.936 and 0.97 for alpha angle, 0.967 and 0.986 for beta angle, 0.982 and 0.996 for gamma angle, and 0.955 and 0.974 for dx distance measurement, indicating excellent consistency.
The sample size was obtained by similarity with previous cadaveric and in vivo studies investigating patellar tracking analysis; these studies typically use fewer than 10 knees to reach statistical significance [15, 33, 36, 48].
Results
One set of images could not be retrieved due to a hardware malfunction, despite having the radiation calculation available. Another patient, who missed the second CT and clinical scoring, did not attend the follow-up after pre-CT and surgery. Thus, the measurements presented in the tables, and graphics refer to 8 complete sets of images. The clinical results refer to nine patients, and the radiation analysis refers to 19 CTs.
The first 12 CTs were analysed. Imaging protocol 1 had a final effective radiation dose mean of 1.306 mSv, which is approximately 6.5 times greater than the protocol 2 mean of 0.203 mSv. Protocol 2 enabled adequate identification of all reference points. We therefore decided to use protocol 2 in the eight remaining examinations.
The values for the alpha, beta, and gamma angles and the dx distance, as well as the results of statistical tests comparing the pre- and post-operative periods, are summarized in Tables 2 and 3.
There were no differences in the angles or the dx distances between the pre- and post-operative periods with the exception of the dx distance between 79° and 70° and that between 39° and 30°.
Figures 3 and 4 describe the angles and dx distance in relation to the flexion angle by comparing pre- and post-operative measurements.
No lateral retinacular releases were performed because in all cases, the patella could be medialized more than 5 mm from its centred position and its lateral edge could be raised until medially tilted. No patient presented with instability recurrence in the follow-up period. Clinical scores improved from a mean of 51.9 (±15.6) –74.2 (±20.9) on the Kujala scale (p = 0.011) and from a median of 2 (range 0–4) to 4 (range 1–6) on the Tegner scale (p = 0.017).
Discussion
The most important finding of the present study was that MPFL reconstruction, although successful for patellar stabilization, showed no improvement in patellar tilt or shift in the population studied.
Only patients with isolated indication of MPFL reconstruction were included. The parameters used to contraindicate associated corrections were based on the clinical experience of the authors reinforced by non-consensual literature. It can be argued that there was diversity in the anatomical profiles of the patients (Table 1), but this is a characteristic of recurrent patellar instability patients. Most patients had increased patellar tilt and altered tracking caused by a combination of several mild anatomical abnormalities without indication for individual surgical correction by the chosen criteria. Hence, the studied population is typically referred for isolated MPFL reconstruction, and an improvement in tracking could be expected after surgery.
Some studies in cadavers [31, 39] showed that patellar behaviour is restored with MPFL reconstruction when a lateralization force is applied to the patella. Zaffagnini et al. [48] showed that without lateral load, MPFL resection did not alter patellar tilt and shift, reinforcing the idea that the ligament probably has only a passive function in restraining lateralization. However, it cannot be assumed from these cadaver models with normal anatomy that the patellar tracking during active movement is modified by in vivo surgery in patients with abnormal anatomy, nor can possible loosening of the graft that may occur over time be ignored. Few studies have evaluated the effect of this surgery in vivo. Kita et al. [24] investigated the persistence of patellar centralization achieved with MPFL reconstruction after at least 6 months; in agreement with the findings of the present study, in 16 out 25 knees the patella shifted laterally upon knee extension. Of note, the study had no muscle contraction, which could result in underestimation of lateralization.
Orthopaedics dynamic studies in vivo have always been a challenge. Because most of the imaging is static, it is often difficult to draw conclusions regarding how a joint behaves during gait and normal or pathological muscle contraction. Skin motion capture sensors [26], biplane radiography [1, 4, 21, 27], MRI, and 3D computer reconstruction models with muscle contraction [7, 17, 18, 35, 42, 47] have all been used to study patellar tracking, but these methods are methodologically complex and are not commercially available. Several studies have reported the dynamic use of CT in the analysis of the PF joint, but the method comprises sequential static slices with or without quadriceps contraction [5, 22, 37].
A truly continuous dynamic CT analysis is a very recent achievement. In 2014, Elias et al. [15] published a study comparing the pre- and post-operative patellar tracking of six patients with patellar instability undergoing TT medial transfer, associated with MPFL reconstruction in five cases. The study used an imaging method similar to that used in the current study, but patellar tracking analysis used complex and less available computer modelling. The authors found a statistically significant improvement of 7° in patellar tilt and of 7 mm in patellar lateralization at the 5° flexion angle, probably because of TT realignment.
Regarding the margin of error of the measurements, the minimum sensitivity of a linear measurement in the software was limited by slice thickness (0.5 mm). The software had a maximum approximation error of 2 pixels (0.78 mm). Therefore, with a maximum error of up to 1.3 mm and the excellent intraclass correlation found, the method can be considered quite accurate and reproducible.
The results of this work show that no patellar tracking parameters changed due to MPFL reconstruction. Even so, none of the patients had instability recurrence in the follow-up. Viewing the plots, it is clear that below 30° of flexion, there was an acceleration of patellar shift (3 to over 16 mm) and lateral tilt (15° to more than 32°) both pre- and post-operatively (Figs. 3, 4). The only significant differences found (mean dx distance between 79°–70° and 39o–30° of flexion) had a magnitude lacking clinical significance and were in the range of the error of the method (<1.3 mm).
With regard to the clinical results, the population had an overall score improvement inferior to that usually observed in the literature [23, 40], probably because of the chronic presentation of instability in the sample, which led to long-term withdrawal from sports activities and poor muscular performance that could not be completely reverted during the follow-up. Patient JCS had worsening of the Kujala score due to worsening anterior knee pain not related to surgery issues; she had previous patellar cartilage degeneration not addressed, without indication for tibial tuberosity transfer.
One limitation of the method is that movement is performed in a non-standing open kinematic chain, against gravity. Nevertheless, most studies citing imaging under load use muscular contraction in a closed kinematic chain with the patient lying down [17].
Another initial potential limitation of the method was radiation exposure. This was solved using protocol 2. Mammography can generate 0.4 mSv, double the effective radiation of the presented protocol. Therefore, this method is not limited by radiation.
It is essential to emphasize that the alpha, beta, and gamma angles and the dx distance allow patellar tracking analysis but are not meant to be compared to traditional measures used in conventional radiography or CT. There is difficulty in making the data comprehensible to the reader because of its complexity and unfamiliarity; this is another limitation of the study.
This study is one of the first studies to consistently assess in vivo active patellar tracking after isolated MPFL reconstruction in a population with recurrent patellar instability. The results, as a whole, reinforce the idea that MPFL reconstruction should not be considered a proximal realignment but instead a stabilizing surgery and are of clinical relevance to the surgeon planning this procedure in the presence of altered lateral tracking. This study alone cannot suggest how to correct the tracking in patients with borderline deformities that are usually referred to isolated MPFL reconstruction, but surgeons should probably be more inclined to perform associated procedures such as trochleoplasty and patellar height correction in this clinical setting.
Finally, this form of in vivo evaluation of patellar tracking may be reproduced in a consistent manner and with low radiation exposure in any centre with a 320-detector-row CT scanner, opening new possibilities for investigating the kinematic results of patellofemoral interventions.
Conclusions
Although successfully stabilizing the patella and improving clinical scores, MPFL reconstruction resulted in no improvement in patellar tilt or shift in the population studied. A low-radiation protocol for patellofemoral dynamic CT was described for measuring changes in patellar tracking.
References
Anderst W, Zauel R, Bishop J, Demps E, Tashman S (2009) Validation of three-dimensional model-based tibio-femoral tracking during running. Med Eng Phys 31:10–16
Beck P, Brown NA, Greis PE, Burks RT (2007) Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med 35:1557–1563
Beighton P, Solomon L, Soskolne CL (1973) Articular mobility in an African population. Ann Rheum Dis 32:413–418
Bey MJ, Kline SK, Tashman S, Zauel R (2008) Accuracy of biplane X-ray imaging combined with model-based tracking for measuring in vivo patellofemoral joint motion. J Orthop Surg Res 3:38
Biedert RM, Gruhl C (1997) Axial computed tomography of the patellofemoral joint with and without quadriceps contraction. Arch Orthop Trauma Surg 116:77–82
Bitar AC, D'Elia CO, Demange MK, Viegas AC, Camanho GL (2015) Randomized prospective study on traumatic patellar dislocation: conservative treatment versus reconstruction of the medial patellofemoral ligament using the patellar tendon, with a minimum of two years of follow-up. Rev Bras Ortop 46:675–683
Biyani R, Elias JJ, Saranathan A, Feng H, Guseila LM, Morscher MA, Jones KC (2014) Anatomical factors influencing patellar tracking in the unstable patellofemoral joint. Knee Surg Sports Traumatol Arthrosc 22:2334–2341
Camanho GL, Bitar AC, Hernandez AJ, Olivi R (2007) Medial patellofemoral ligament reconstruction: a novel technique using the patellar ligament. Arthroscopy 23:108e1–1084
Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H (1982) Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 68:317–325
Deie M, Ochi M, Sumen Y, Adachi N, Kobayashi K, Yasumoto M (2005) A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports Traumatol Arthrosc 13:522–528
Dejour D, Reynaud P, Lecoultre B (1998) Douleurs et instabilite rotulienne Essai de classification. Med Hyg 56:1466–1471
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Dewey M, Zimmermann E, Deissenrieder F, Laule M, Dübel HP, Schlattmann P, Knebel F, Rutsch W, Hamm B (2009) Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 120:867–875
Donell ST, Joseph G, Hing CB, Marshall TJ (2006) Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. Knee 13:266–273
Elias JJ, Carrino JA, Saranathan A, Guseila LM, Tanaka MJ, Cosgarea AJ (2014) Variations in kinematics and function following patellar stabilization including tibial tuberosity realignment. Knee Surg Sports Traumatol Arthrosc 22:2350–2356
Feller JA, Richmond AK, Wasiak J (2014) Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc 22:2470–2476
Fellows RA, Hill NA, Gill HS, MacIntyre NJ, Harrison MM, Ellis RE, Wilson DR (2005) Magnetic resonance imaging for in vivo assessment of three-dimensional patellar tracking. J Biomech 38:1643–1652
Fellows RA, Hill NA, Macintyre NJ, Harrison MM, Ellis RE, Wilson DR (2005) Repeatability of a novel technique for in vivo measurement of three-dimensional patellar tracking using magnetic resonance imaging. J Magn Reson Imaging 22:145–153
Fernandez E, Sala D, Castejon M (2005) Reconstruction of the medial patellofemoral ligament for patellar instability using a semitendinosus autograft. Acta Orthop Belg 71:303–308
Galland O, Walch G, Dejour H, Carret JP (1990) An anatomical and radiological study of the femoropatellar articulation. Surg Radiol Anat 12:119–125
Giphart JE, Zirker CA, Myers CA, Pennington WW, LaPrade RF (2012) Accuracy of a contour-based biplane fluoroscopy technique for tracking knee joint kinematics of different speeds. J Biomech 45:2935–2938
Jan MH, Lin DH, Lin CH, Lin YF, Cheng CK (2009) The effects of quadriceps contraction on different patellofemoral alignment subtypes: an axial computed tomography study. J Orthop Sports Phys Ther 39:264–269
Kang HJ, Cao JH, Pan S, Wang XJ, da Yu H, Zheng ZM (2014) The horizontal Y-shaped graft with respective graft tension angles in anatomical two-bundle medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 22:2445–2451
Kita K, Horibe S, Toritsuka Y, Nakamura N, Tanaka Y, Yonetani Y, Mae T, Nakata K, Yoshikawa H, Shino K (2012) Effects of medial patellofemoral ligament reconstruction on patellar tracking. Knee Surg Sports Traumatol Arthrosc 20:829–837
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Laprade J, Lee R (2005) Real-time measurement of patellofemoral kinematics in asymptomatic subjects. Knee 12:63–72
Li G, Van de Velde SK, Bingham JT (2008) Validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion. J Biomech 41:1616–1622
MacKay JW, Godley KC, Toms AP, Donell ST (2014) Trochlear boss height measurement: a comparison of radiographs and MRI. Knee 21:1052–1057
Merchant AC, Mercer RL, Jacobsen RH, Cool CR (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 56:1391–1396
Mikashima Y, Kimura M, Kobayashi Y, Miyawaki M, Tomatsu T (2006) Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. Acta Orthop Belg 72:65–71
Nomura E, Horiuchi Y, Kihara M (2000) Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee 7:121–127
Nomura E, Inoue M (2006) Hybrid medial patellofemoral ligament reconstruction using the semitendinous tendon for recurrent patellar dislocation: minimum 3 years’ follow-up. Arthroscopy 22:787–793
Ntagiopoulos PG, Sharma B, Bignozzi S, Lopomo N, Colle F, Zaffagnini S, Dejour D (2013) Are the tubular grafts in the femoral tunnel in an anatomical or isometric position in the reconstruction of medial patellofemoral ligament? Int Orthop 37:1933–1941
Ostermeier S, Stukenborg-Colsman C, Hurschler C, Wirth CJ (2006) In vitro investigation of the effect of medial patellofemoral ligament reconstruction and medial tibial tuberosity transfer on lateral patellar stability. Arthroscopy 22:308–319
Park HJ, Ahn JH, Kim SS, Lee SY, Choi YJ, Chung EC, Rho MH, Kook SH (2013) A new assessment of patellar instability using coronal magnetic resonance images of the patella superimposed on the femur and its clinical utility. J Comput Assist Tomogr 37:470–474
Philippot R, Boyer B, Testa R, Farizon F, Moyen B (2012) Study of patellar kinematics after reconstruction of the medial patellofemoral ligament. Clin Biomech 27:22–26
Pinar H, Akseki D, Genc I, Karaoglan O (1994) Kinematic and dynamic axial computerized tomography of the normal patellofemoral joint. Knee Surg Sports Traumatol Arthrosc 2:27–30
Rybicki FJ, Otero HJ, Steigner ML, Vorobiof G, Nallamshetty L, Mitsouras D, Ersoy H, Mather RT, Judy PF, Cai T, Coyner K, Schultz K, Whitmore AG, Di Carli MF (2008) Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging 24:535–546
Sandmeier RH, Burks RT, Bachus KN, Billings A (2000) The effect of reconstruction of the medial patellofemoral ligament on patellar tracking. Am J Sports Med 28:345–349
Schneider DK, Grawe B, Magnussen RA, Ceasar A, Parikh SN, Wall EJ, Colosimo AJ, Kaeding CC, Myer GD (2016) Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and meta-analysis. Am J Sports Med. doi:10.1177/0363546515624673
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35:801–804
Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE (2010) Q-angle and J-sign: indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res 468:266–275
Smith TO, Clark A, Neda S, Arendt EA, Post WR, Grelsamer RP, Dejour D, Almqvist KF, Donell ST (2012) The intra- and inter-observer reliability of the physical examination methods used to assess patients with patellofemoral joint instability. Knee 19:404–410
Tecklenburg K, Dejour D, Hoser C, Fink C (2006) Bony and cartilaginous anatomy of the patellofemoral joint. Knee Surg Sports Traumatol Arthrosc 14:235–240
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Van Haver A, De Roo K, De Beule M, Labey L, De Baets P, Dejour D, Claessens T, Verdonk P (2015) The effect of trochlear dysplasia on patellofemoral biomechanicas: a cadaveric study with simulated trochlear deformities. Am J Sports Med 43:1354–1361
Yamada Y, Toritsuka Y, Horibe S, Sugamoto K, Yoshikawa H, Shino K (2007) In vivo movement analysis of the patella using a three-dimensional computer model. J Bone Joint Surg Br 89:752–760
Zaffagnini S, Colle F, Lopomo N, Sharma B, Bignozzi S, Dejour D, Marcacci M (2013) The influence of medial patellofemoral ligament on patellofemoral joint kinematics and patellar stability. Knee Surg Sports Traumatol Arthrosc 21:2164–2171
Acknowledgment
The São Paulo Research Foundation (Fundação de Amparo à Pesquisa do Estado de São Paulo—Fapesp) provided financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gobbi, R.G., Demange, M.K., de Ávila, L.F.R. et al. Patellar tracking after isolated medial patellofemoral ligament reconstruction: dynamic evaluation using computed tomography. Knee Surg Sports Traumatol Arthrosc 25, 3197–3205 (2017). https://doi.org/10.1007/s00167-016-4284-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4284-x