Abstract
Purpose
The patellofemoral (PF) joint may be adversely affected by medial open-wedge high tibial osteotomy (OWHTO). This study aimed to evaluate the PF compartmental changes using combined single-photon emission computed tomography (SPECT) and conventional computed tomography (CT) after OWHTO to provide clinical guidance regarding the PF joint pressure and force.
Methods
Patients with medial osteoarthritis and varus malalignment > 5° were treated using OWHTO. Patients with a minimum 2-year follow-up were included in the study. The patellar positions were evaluated based on the radiographic parameters. The changes in chondral lesions during second-look arthroscopic examination were evaluated, and the PF joint arthritis grade was recorded on patellar Merchant radiographs using Kellgren–Lawrence classification. The PF compartmental changes according to SPECT/CT analysis after OWHTO were evaluated in all patients. The scintigraphic uptake was graded on four scales. Patients were divided into improved and unimproved groups according to the PF compartmental grade using the SPECT/CT uptake grading system.
Results
At a mean follow-up period of 47.0 months (range 25–74 months), the mean mechanical femorotibial angle changed significantly from varus 6.3° (range 5–12°) to valgus 2.6° (range 0–8°); p < 0.001) postoperatively. The radiological parameters presenting patellar positions, including the tibial slope, patellar convergence angle, and lateral tilt angle, did not change significantly between the preoperative values and the 2-year follow-up values. The mean patellar height significantly decreased (0.07 ± 0.14, p = 0.001 according to the Blackburn–Peel index and 0.32 ± 0.23, p < 0.001 using the modified Insall–Salvati ratio). The average tibial tubercle to trochlear groove (TT–TG) distance significantly decreased from 14.1 to 12.2 mm (p < 0.001). The Q angle also significantly decreased from 9.8o to 7.7o (p = 0.008). Chondral lesions of the patella and trochlear groove revealed significant deterioration; at 2 years after OWHTO, the arthritic grades of the PF joints worsened significantly, as determined by radiography (p = 0.007). Scintigraphic uptake in the PF joint was significantly lower (from 2 to 1) at 2 years postoperatively compared to that immediately after the index operation (p < 0.001). Only 4 of 56 (7.1%) patients showed increased uptake. Comparison between the improved and unimproved groups according to scintigraphic uptake changes revealed that the changes in the cartilage status on the patellar undersurface and TT–TG distance were the most significant predictive factors of increased scintigraphic uptake in the PF joint after OWHTO.
Conclusion
Alignment correction by OWHTO result in PF compartment offloading and should be considered when identifying the surgical indications for OWHTO.
Level of evidence
Therapeutic, Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Open-wedge high tibial osteotomy (OWHTO) decreases the moment arm of the ground reaction force and further offloads the medial compartment of the knee, resulting in decreased cartilage degeneration in the medial compartment with proven clinical improvement in the pain symptoms [28]. However, several studies have reported the acceleration of degenerative change resulting from increased contact pressure at the patellofemoral (PF) joint [35] owing to the increased Q angle, altered PF joint tracking [9], and unintended changes in the patellar height after OWHTO [10, 20].
As the PF joint function is maintained by a complex interaction between the soft tissues and bony structures, the PF joint pressure and force cannot be evaluated only by calculation of the Q angle and altered patellar height. There is little reported evidence of an association between patient complaint and deterioration affecting PF joints [20]. Goshima et al. reported that the changes in PF alignment and arthritic progression did not affect the clinical outcomes of OWHTO at mid-term follow-up [10]. The principal effect of OWHTO is alleviation of medial knee pain. Therefore, the clinical assessment of anterior knee pain and functional assessment may provide secondary information and may be affected by clinical improvement in the medial knee pain. Especially, owing to the poor correlation between radiographic abnormalities and anterior knee pain [19], objective detection tools are required to evaluate the effect of OWHTO on the PF joint.
The combined single-photon emission computed tomography and conventional computed tomography (SPECT/CT) is a highly sensitive tool for detecting bone metabolism [2, 29]. Hirschmann et al. [12, 35, 37] reported the efficacy of SPECT/CT for determining the source of the patients’ symptoms with respect to the PF joint. Thus, SPECT/CT findings can provide more objective OWHTO outcomes with respect to the PF joint pressure and force, which are important for elucidating the possible long-term sequelae associated with the procedure [28].
The scintigraphic uptake in the PF compartment detected on SPECT/CT may change with alterations in the PF contact force according to the changes in the PF alignment after OWHTO and that the change in the scintigraphic uptake in the PF compartment may be correlated with the postoperative cartilage deterioration or arthritic progression. Therefore, this study aimed to evaluate the change in the scintigraphic uptake in the PF joint using SPECT/CT after OWHTO, and to identify the variables associated with these changes.
We hypothesized that the altered patellar position, such as denoted by decreased tibial tuberosity–trochlear groove (TT–TG) distance [11], would change the soft-tissue tension and muscle activity applied to the patella, and affect on the PF joint.
Materials and methods
Participants
This retrospective study included 53 patients who underwent OWHTO between January 2013 and May 2017. The indications for OWHTO were, as follows: (1) medial tibiofemoral osteoarthritis (OA) with varus malalignment > 5° (measured on preoperative double-limb standing radiographs); (2) near-normal range of motion (flexion > 90° and flexion contracture < 5°). The additional inclusion criteria were, as follows: (1) ≥ 2-year follow-up; (2) simultaneous hardware removal and second-look arthroscopy; and (3) diagnosis of International Cartilage Repair Society (ICRS) grade ≤ 3 PF chondral lesions. Nine patients aged > 69 years with a medical history that included previous surgery with excessive arthroscopic debridement and/or any additional injury or disorder, such as rupture of the cruciate ligament, were excluded from the study. OWHTO was performed on 53 patients (56 knees). The mean follow-up period was 47.0 ± 13.5 months (range 25–74 months). The mean patient age at the time of the surgery was 56.2 ± 6.0 years (range 41–66 years). Of the 53 patients, 13 were male. The mean body mass index was 26.3 ± 3.6 kg/m2 (range 19.1–35.4 kg/m2).
Surgical techniques and postoperative rehabilitation
Arthroscopic partial meniscectomy or suturing was performed when a medial meniscus injury was found. All knees were subjected to OWHTO using a lateral cortical hinge by a single experienced surgeon. Thin osteotomes were then used to complete the osteotomy just short of the lateral cortex, and both the lateral cortex and lateral capsular hinge were maintained intact. Subsequently, osteotomy was performed using the prescribed method, exercising care to complete osteotomy of the posterior cortex. The anterior gap at the osteotomy site was approximately two-thirds that of the posterior gap. The correction angle was planned preoperatively using the Miniaci method to achieve a target alignment passing through the Fujisawa point [8]. The osteotomy was stabilized using a fixed-angle plate with interlocking screws (TomoFixTM104; Synthes, Bettlach, Switzerland) or an Ohtofix HTO plate (Ohtomedical Co. Ltd., Goyang, Republic of Korea).
The postoperative rehabilitation protocol for the OWHTO group included isometric-quadriceps, active-ankle, and straight-leg-raising exercises commencing on the day after the surgery. Patients were restricted from toe-touch weight-bearing for the first 2 weeks postoperatively, followed by partial weight-bearing for the next 4 weeks. Full weight-bearing was permitted at 8–12 weeks, following radiographic evaluation for bone consolidation at the osteotomy site. A cast or brace was not used postoperatively.
Clinical and radiographic assessment
The clinical outcomes were evaluated and compared using the American Knee Society score (KSS) and function score (KSFS) [31] and Kujala score [21] preoperatively and at the postoperative 2-year follow-up. The radiographic evaluations entailed assessment of full-length standing hip-to-ankle, anteroposterior knee, and lateral and patellar merchant radiographs. The mechanical femorotibial angle (MFTA) and mechanical medial proximal tibial angle (mMPTA) were measured using full-length standing hip-to-ankle radiographs obtained preoperatively and postoperatively (at the 2-year follow-up). The MFTA was defined as the angle between the mechanical axes of the femur and tibia, and the mMPTA was defined as the medial angle between a line drawn parallel to the proximal tibial condyles and the mechanical axis of the tibia. The tibial slope was defined as the angle between the line perpendicular to the mid-diaphysis of the tibia and the line depicting the posterior inclination of the tibial plateau on lateral view radiographs in full extension. The radiographic parameters presenting patellar positions, such as patella congruence angle (CA), lateral PF tilt angle (LTA), and TT–TG distance [32], were evaluated. The TT–TG distances on the CT images were measured between the most cephalad point of the tibial tubercle and the deepest point of the trochlear groove, with the trochlear line drawn perpendicular to the posterior condylar line and passing through the deepest point of the trochlear groove. The Blackburn–Peel index (BPI) and modified Insall–Salvati (mIS) ratio were measured using a standing lateral view of the knee at 30° flexion [30]. The Q angle was measured using scanograms of both legs in the stance phase. The Q angle was manually measured as the angle between the line connecting the anterior superior iliac spine with the center of the patella and the line connecting the center of the patella and the tibial tubercle.
A total of 53 patients (56 knees) who underwent an additional operation at 2 years postoperatively for hardware removal agreed to undergo a second-look arthroscopic evaluation. The chondral lesion changes were evaluated during the second-look arthroscopic examination. The degree of cartilage degeneration of the PF and tibiofemoral joints was assessed and semi-quantitatively analyzed according to the ICRS grading system [26]. OA grade of the PF joint on patellar Merchant radiographs was recorded using the Kellgren–Lawrence (K–L) classification [17].
The scintigraphic uptake, observed on SPECT/CT after OWHTO, denoted the PF compartmental changes and was classified as four grades in all patients. The SPECT/CT scans were performed using a Symbia T16 hybrid system (Siemens, Erlangen, Germany) equipped with a pair of low-energy high-resolution collimators and a dual-head gamma camera with an integrated 16 × 0.75-mm slice thickness CT. Two hours after the injection of 700 MBq technetium-99 m hydroxydiphosphonate (HDP) (CIS Bio International, Sur Yvette, France), SPECT was performed with a frame matrix size of 128 × 128; angle step, 32°; and time per frame, 25 s. The reconstructed data were displayed in the transaxial, coronal, and sagittal planes [12].
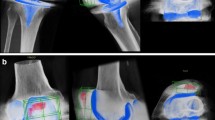
Scintigraphic uptake was graded, as follows: grade 0, no uptake (equivalent to normal cancellous bone); grade 1, higher uptake than that by normal cancellous bone but lower than that by the articular surface; grade 2, same uptake as that by the articular surface; and grade 3, higher uptake than that by the articular surface [33]. Patients were divided into the improved and unimproved groups according to the PF compartmental grade using the SPECT/CT uptake grading system. The improved group included patients showing a decrease in scintigraphic uptake, while the unimproved group included those showing increased or unchanged scintigraphic uptake (Fig. 1).
a A 58-year-old man underwent open-wedge high tibial osteotomy (OWHTO). A 7° varus malalignment of the knee (a) is corrected to 3° valgus (b) of the mechanical axis. Patellar merchant radiographs obtained at the postoperative 2-year follow-up, showing that the arthritis grade of the patellofemoral (PF) joint did not change or mildly improve (e: preoperative, f: postoperative); the scintigraphic uptake is markedly decreased during combined single-photon emission computed tomography and conventional computed tomography (SPECT/CT). b A 61-year-old woman underwent OWHTO. A 6° varus malalignment of the knee (a) is corrected to a 2° valgus (b) of the mechanical axis. Patellar merchant radiographs obtained at the postoperative 2-year follow-up, showing that the arthritis grade of the PF joint is deteriorated (e: preoperative, f: postoperative) and the scintigraphic uptake increased during SPECT/CT
The study protocol was approved by the Institutional Review Board (GCIRB2019-224) from our institution (Gachon University Gil Hospital, Incheon, South Korea) before the commencement of the study. All patients provided informed consent prior to participation in this study.
Statistical analysis
SPSS version 22.0 (SPSS Corp, Chicago, IL, USA) was used for statistical analyses. P values < 0.05 were considered significant. The Shapiro–Wilk test was used to evaluate the normality of distribution. The Wilcoxon signed-rank test was used to compare differences in the preoperative and 2-year postoperative follow-up values. In our study, 32 and 24 knees were allocated to the improved and unimproved groups, respectively. To compare the demographic data and preoperative and postoperative outcomes between the improved and unimproved groups, the Student’s t test or Mann–Whitney U test was used for the continuous variables and the Chi-square test or Fisher’s exact test was used for the categorical variables. Binary logistic regression analysis was used to investigate the factors associated with PF compartmental changes noted on SPECT/CT. The following independent variables were analyzed: patient age, sex, body mass index, preoperative and postoperative MFTA, changes in the tibial slope and mMPTA, ICRS change on the patellar undersurface or trochlear groove, K–L grade change in the PF joint, radiographic parameters of the patellar position (CA, LTA, BPI, mIS ratio, and TT–TG distance), and Q angle. The adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. A ten-point difference in the Kujala score was considered a clinically important difference [7]. We calculated that > 90% power was required to detect a difference of at least 10 points with a standard deviation of 15 points in the Kujala score (α = 0.05) [7]. The sample size was determined with G-power 3.1 for the Wilcoxon signed-rank test with an effect size of 0.5, α error of 0.05, and power of 0.95. The measurement methods were developed and agreed upon by two orthopedic surgeons (independent observers). However, these surgeons were blinded to each other’s measurements and their own previous measurements. They measured the parameters twice, with a 6-week interval between measurements. The inter- and intra-class correlation coefficients were examined to assess the reliability of the measurements and ranged from 0.90 to 0.95 and from 0.89 to 0.99, respectively, indicating a significantly high agreement between the two observers on the radiographic and arthroscopic measurements (an appendix is available as a supplemental file, Table s1). The SPECT/CT measurements were also interpreted twice by two independent observers. The inter-observer reliability quantified using intra-class correlation coefficients (ICCs) was > 0.82 in all cases.
Results
The clinical outcomes, including the Kujala score, KSS, and KSFS, significantly improved at 2-year follow-up compared with the preoperative measurements (all subscales; p < 0.001). The mean preoperative MFTA was 6.3° varus corrected to mean 2.6° valgus postoperatively. The radiological parameters presenting patellar positions, including the tibial slope, patellar convergence angle, and lateral tilt angle, did not show significant changes between the preoperative values and values recorded at the 2-year follow-up. However, the patellar height significantly decreased (mean difference in the BPI, 0.07 ± 0.14, p = 0.001; mean difference in the mIS ratio: 0.32 ± 0.23, p < 0.001). The average TT–TG distance significantly decreased from 14.1 to 12.2 mm postoperatively (p < 0.001). The Q angle also significantly decreased from 9.8° to 7.7° (p = 0.008; Table 1).
A semi-quantitative evaluation using the ICRS grade scoring system [26] revealed mildly significant deterioration in the chondral lesions on the patellar undersurface and trochlear groove. Second-look arthroscopy was performed concomitantly with plate removal at a mean duration of 25.0 ± 4.8 months after the index operation. Radiographically, the K–L grades of the PF joints worsened slightly and significantly at 2 years after OWHTO (p = 0.007). The scintigraphic uptake in the patella or femoral trochlea was significantly lower at 2 years postoperatively compared to that after the index operation (from 2 to 1; p < 0.001). Among the 53 knees, 32 (57.1%) showed decreased scintigraphic uptake, 19 (33.9%) showed no change, and 4 (7.1%) showed increased uptake.
Table 2 compares the improved and unimproved groups classified according to changes in the scintigraphic uptake. The improved group showed less progression of the chondral lesions on the patellar undersurface. A decrease in the scintigraphic uptake was observed in patients with a larger Q angle and greater TT–TG distance, which significantly correlated with a greater decrease in the TT–TG distance. The other independent variables, including patient demographic characteristics and radiographic parameters of the patellar position, showed no significant intergroup differences. The same results were noted in the binary logistic regression analysis (Table 3). The changes in the ICRS grade of the patellar undersurface and in the TT–TG distance were the most significant predictive factors for increased scintigraphic uptake in the PF joint after OWHTO (R 2n = 0.34 and 0.71, respectively).
Discussion
The principal findings of this study are as follows: (1) only 7.1% of the patients who underwent OWHTO showed increased scintigraphic uptake and almost all patients showed decreased or unchanged uptake in the PF compartment on SPECT/CT performed at 2 years postoperatively; (2) the radiologic evaluations of the patellar position after OWHTO revealed decreased TT–TG distance and Q angle, and descent of the patella was observed, but the patellar tilt angle was not changed; (3) the change in scintigraphic uptake was significantly correlated with the changes in the TT–TG distance and cartilage status on the patellar undersurface.
Several studies have reported that chondral lesions identified using imaging modalities or during arthroscopy do not correlate well with the presence or severity of PF pain in patients [34, 37]. To improve patient outcomes, the effect of an OWHTO on the PF joint must be well understood with established correlations between increased contact pressure and progression of cartilage deterioration [15]. However, conventional radiographs are limited in their ability to identify PF disorders indicated by the poor correlation between radiographic abnormalities and PF pain [19]. Such limitations would be overcome with the development of hybrid SPECT/CT systems that can provide clear anatomical detailed evaluation through high-resolution CT imaging with bone physiological activity detected in an SPECT study.
SPECT/CT is a hybrid imaging modality that combines three-dimensional bone scintigraphy and conventional CT into a single imaging procedure [12, 29]. The intensity and distribution of the SPECT/CT tracer uptake correlate with the mechanical overload of the knee joint [29]. Increased shear stress in the patellar cartilage can increase the metabolic activity of the subchondral bone, ultimately triggering anterior knee pain [12]. Furthermore, higher SPECT/CT tracer uptake of a specific compartment by an altered loading pattern is significantly correlated with a higher risk of OA progression [29]. Hence, when the signal strength is measured using SPECT/CT after HTO, possible long-term sequelae on the PF joint can be identified even with a short follow-up, allowing for the early diagnosis of complications and providing guidance for further treatment in patients with postoperative pain [12].
Several studies have reported variable results regarding postoperative changes of the patellar position according to radiographic parameters, including the patellar height, lateral tilt and shift, and tibial posterior slope. Regarding patellar height, patella infera may lead to increased retropatellar pressure and contact forces with a resultant risk of knee pain and reduced range of motion [18]. However, it is still controversial whether PF contact stress changes with altered patella height [36]. With regard to OWHTO, Chae et al. [1] reported that the mean BPI decreased from 0.71 to 0.61 (p < 0.001) after OWHTO. Jingbo et al. [16] reported that patellar height was not altered when the knee axis correction was < 15°. In the present study, there was significant patellar descent postoperatively. However, it did not adversely affect the postoperative outcomes by SPECT/CT analysis. Regarding the patellar tilt and tibial slope angle, no significant postoperative changes were found in this study. However, the previous studies have reported changes in the patellar tilt and the tibial slope angle after OWHTO [4, 23]. In addition, several techniques have been used to avoid the change in tibial slope [3, 4]. Regarding TT–TG distance, the present results showed a significant decrease after OWHTO. This can be explained by the tendency of the internal rotation of the distal tibia after OWHTO results in decreased TT–TG distance. The change in TT–TG distance and ratio profiles affect the soft-tissue tension of the medial hamstrings/soft-tissue structures [11], muscle actions applied to the patella, and kinematics of the PF joint.
There are a few theoretical rationales to explain the decrease in scintigraphic uptake of the PF compartment by SPECT/CT after OWHTO. First, contrary to the anticipation of an increase in the Q angle after OWHTO, a decreasing effect of the Q angle from 10° to 7° was observed. Q angle is determined by several composites of pelvic position, hip rotation, tibial rotation, patella position, and foot position. We posit that the decreased Q angle may have been a result of the decreased TT–TG distance due to internal rotation of the distal tibia and reduction of the lateral subluxation of the tibia in varus malaligned arthritic knees.
These changes in the patellar position and alignment should be considered for understanding changes in the PF joint contact pressure with the muscle forces applied to the patella. Stronger quadriceps muscles help to improve joint stability, absorb shock, and attenuate ground reaction forces during gait [27], which may, subsequently, improve knee pain and function [38]. However, this mechanism may be less effective in cases of malaligned knees, possibly due to damaged mechanoreceptors from stretched joint capsules or ligaments producing abnormal afferent signals that decrease quadriceps contraction [14]. Stronger quadriceps can also increase PF joint compression, which accentuates knee malalignment. Varus malalignment has been associated with the presence of medial PF joint OA [5]. Therefore, alignment correction may improve quadriceps efficiency and protect against medial PF joint cartilage deterioration.
Second, the change in PF joint contact pressure should be investigated alongside the muscle forces applied to the patella, particularly the vastus medius obliquus (VMO). A slight increase in the compression as the VMO force is increased which contributes to a more consistent medial pressure increase compared to the lateral pressure decrease [6]. The VMO pulls at a more horizontal angle of 50–55° to the long axis of the femur than the other Q muscles (the vastus lateralis pulls at 12–15° and the vastus medialis longus pulls at 15–18°) [6]. Therefore, a change in the direction of the VMO in patients who undergo OWHTO changes the forces applied to the patella, albeit slight, and the quadriceps efficiency, including the VMO, increases as the medial PF contact pressure markedly decreases. Furthermore, the lessened iliotibial band tension by validation contributes to the relief of symptomatic anterior knee pain [13]. Third, decreases in varus after OWHTO decrease the peak knee adduction moment and peak internal rotation moment [24]. This effect is beneficial for PF decompression with knee flexion during weight-bearing and significant quadriceps tension.
Nevertheless, significant cartilage deterioration and arthritic progression were identified in the present study. The temporary increase in PF contact forces was supposedly induced by postoperative short-term quadriceps atrophy. Several studies have reported cartilage status deterioration after OWHTO with most cases classified with deterioration grade I to II. Our study also showed differences in the cartilage status and arthritic grade at 2-year follow-up after OWHTO, including 0.1–0.5 according to ICRS grade and 0.1 for the K–L grade.
The present study has several limitations. First, there is a fundamental limitation due to its retrospective design with a relatively small sample size. Second, it had a relatively short-term follow-up period which does not allow for determination of the procedure’s long-term sequelae of the PF joint. However, a 2-year follow-up period is sufficient to determine the effect of an HTO on PF pressure and forces by SPECT/CT that are associated with long-term sequelae. Third, SPECT images are often ill-defined and lack precise anatomical detail for quantitative measurement. Consequently, a quantitative comparison of the position, size, and intensity of SPECT uptake regions among patients is difficult. Although SPECT/CT has been accepted as an effective diagnostic tool in the orthopedic field, its use has several limitations. For example, its clinical adoption has been limited due to shortcomings in the available analytical tools. However, the use of a scanning protocol to perform and analyze SPECT/CT outcomes allows for meaningful clinical observation and provides useful information to further guide surgical management [25]. Fourth, when patellar tilt is increased after OWHTO, the lateral PF contact pressure can be increased from altered quadriceps loading [6, 22]. Overloading lateral cartilage can lead to chondrosis on the lateral facet of the patella [37], but the proposed SPECT/CT protocol could not distinguish the anatomical detail of the PF joint. Fifth, this study did not show a significant correlation between PF compartment scintigraphic uptake and clinical outcomes. A more detailed clinical exam related to the PF compartment is required to further investigate this topic. Six, heterogeneity of treatment and study cohort, using two fixed-angle plates with interlocking screws, can be a limitation. However, both products have been clinically verified in several international published papers.
Several studies have reported that there is no significant correlation between changes in the PF alignment and clinical outcomes after OWHTO. However, the reason for this has been not clarified [10]. This study revealed that alignment correction using OWHTO yields decreased TT–TG distance, possibly resulting in internal rotation of the distal tibia and Q angle. Thus, the altered muscle actions applied to the patella will decrease the PF joint contact pressure and anterior knee pain. In contrast to the previous studies on the adverse effects on the PF joint after OWHTO, in the present study, improvement in the PF joint was noted using the SPECT/CT analysis. Therefore, the previous reports on the adverse effects of OWHTO on the PF joint must be reconsidered.
Conclusion
Alignment correction by OWHTO results in PF compartment offloading and should be considered when identifying the surgical indications for OWHTO.
References
Chae DJ, Shetty GM, Lee DB, Choi HW, Han SB, Nha KW (2008) Tibial slope and patellar height after opening wedge high tibia osteotomy using autologous tricortical iliac bone graft. Knee 15:128–133
Dordevic M, Hirschmann MT, Rechsteiner J, Falkowski A, Testa E, Hirschmann A (2016) Do chondral lesions of the knee correlate with bone tracer uptake by using SPECT/CT? Radiology 278:223–231
Ducat A, Sariali E, Lebel B, Mertl P, Hernigou P, Flecher X et al (2012) Posterior tibial slope changes after opening- and closing-wedge high tibial osteotomy: a comparative prospective multicenter study. Orthop Traumatol Surg Res 98:68–74
El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S (2010) Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med 38:323–329
Elahi S, Cahue S, Felson DT, Engelman L, Sharma L (2000) The association between varus-valgus alignment and patellofemoral osteoarthritis. Arthritis Rheum 43:1874–1880
Elias JJ, Kilambi S, Goerke DR, Cosgarea AJ (2009) Improving vastus medialis obliquus function reduces pressure applied to lateral patellofemoral cartilage. J Orthop Res 27:578–583
Felli L, Formica M, Lovisolo S, Capello AG, Alessio-Mazzola M (2018) Clinical Outcome of Arthroscopic Lateral Retinacular Release for Symptomatic Bipartite Patella in Athletes. Arthroscopy 34:1550–1558
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 10:585–608
Gaasbeek R, Welsing R, Barink M, Verdonschot N, van Kampen A (2007) The influence of open and closed high tibial osteotomy on dynamic patellar tracking: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 15:978–984
Goshima K, Sawaguchi T, Shigemoto K, Iwai S, Nakanishi A, Ueoka K (2017) Patellofemoral osteoarthritis progression and alignment changes after open-wedge high tibial osteotomy do not affect clinical outcomes at mid-term follow-up. Arthroscopy 33:1832–1839
Hinterwimmer S, Feucht MJ, Paul J, Kirchhoff C, Sauerschnig M, Imhoff AB et al (2016) Analysis of the effects of high tibial osteotomy on tibial rotation. Int Orthop 40:1849–1854
Hirschmann MT, Iranpour F, Davda K, Rasch H, Hugli R, Friederich NF (2010) Combined single-photon emission computerized tomography and conventional computerized tomography (SPECT/CT): clinical value for the knee surgeons? Knee Surg Sports Traumatol Arthrosc 18:341–345
Hudson Z, Darthuy E (2009) Iliotibial band tightness and patellofemoral pain syndrome: a case-control study. Man Ther 14:147–151
Hurley MV, Scott DL, Rees J, Newham DJ (1997) Sensorimotor changes and functional performance in patients with knee osteoarthritis. Ann Rheum Dis 56:641–648
Javidan P, Adamson GJ, Miller JR, Durand P Jr, Dawson PA, Pink MM et al (2013) The effect of medial opening wedge proximal tibial osteotomy on patellofemoral contact. Am J Sports Med 41:80–86
Jingbo C, Mingli F, Guanglei C, Zheng L, Shuai A, Jiang H (2019) Patellar height is not altered when the knee axis correction is less than 15 degrees and has good short-term clinical outcome. J Knee Surg. https://doi.org/10.1055/s-0039-1681051
Kan H, Arai Y, Kobayashi M, Nakagawa S, Inoue H, Hino M et al (2017) Radiographic measurement of joint space width using the fixed flexion view in 1,102 knees of japanese patients with osteoarthritis in comparison with the standing extended view. Knee Surg Relat Res 29:63–68
Kaper BP, Bourne RB, Rorabeck CH, Macdonald SJ (2001) Patellar infera after high tibial osteotomy. J Arthroplasty 16:168–173
Kijowski R, Blankenbaker D, Stanton P, Fine J, De Smet A (2006) Correlation between radiographic findings of osteoarthritis and arthroscopic findings of articular cartilage degeneration within the patellofemoral joint. Skeletal Radiol 35:895–902
Kim KI, Kim DK, Song SJ, Lee SH, Bae DK (2017) Medial open-wedge high tibial osteotomy may adversely affect the patellofemoral joint. Arthroscopy 33:811–816
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Lee TQ, Sandusky MD, Adeli A, McMahon PJ (2002) Effects of simulated vastus medialis strength variation on patellofemoral joint biomechanics in human cadaver knees. J Rehabil Res Dev 39:429–438
Lee YS, Lee SB, Oh WS, Kwon YE, Lee BK (2016) Changes in patellofemoral alignment do not cause clinical impact after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 24:129–133
Leitch KM, Birmingham TB, Dunning CE, Giffin JR (2015) Medial opening wedge high tibial osteotomy alters knee moments in multiple planes during walking and stair ascent. Gait Posture 42:165–171
Lorberboym M, Ami DB, Zin D, Nikolov G, Adar E (2003) Incremental diagnostic value of 99mTc methylene diphosphonate bone SPECT in patients with patellofemoral pain disorders. Nucl Med Commun 24:403–410
Mainil-Varlet P, Aigner T, Brittberg M, Bullough P, Hollander A, Hunziker E et al (2003) Histological assessment of cartilage repair: a report by the Histology Endpoint Committee of the International Cartilage Repair Society (ICRS). J Bone Joint Surg Am 85:45–57
Mikesky AE, Meyer A, Thompson KL (2000) Relationship between quadriceps strength and rate of loading during gait in women. J Orthop Res 18:171–175
Mucha A, Dordevic M, Hirschmann A, Rasch H, Amsler F, Arnold MP et al (2015) Effect of high tibial osteotomy on joint loading in symptomatic patients with varus aligned knees: a study using SPECT/CT. Knee Surg Sports Traumatol Arthrosc 23:2315–2323
Mucha A, Dordevic M, Testa EA, Rasch H, Hirschmann MT (2013) Assessment of the loading history of patients after high tibial osteotomy using SPECT/CT–a new diagnostic tool and algorithm. J Orthop Surg Res 8:46
Murayama K, Nakayama H, Murakami T, Yoshiya S, Otsuki S, Tachibana T (2018) The effect of concomitant arthroscopic lateral retinacular release on postoperative patellar position and orientation in open wedge high tibial osteotomy. Knee Surg Relat Res 30:241–246
Nha KW, Shin YS, Kwon HM, Sim JA, Na YG (2019) Navigated versus conventional technique in high tibial osteotomy: a meta-analysis focusing on weight bearing effect. Knee Surg Relat Res. https://doi.org/10.5792/ksrr.17.090
Prakash J, Seon JK, Woo SH, Jin C, Song EK (2016) Comparison of radiological parameters between normal and patellar dislocation groups in korean population: a rotational profile CT-based study. Knee Surg Relat Res 28:302–311
du Ro H, Lee HY, Chang CB, Kang SB (2015) Value of SPECT-CT imaging for middle-aged patients with chronic anterior knee pain. BMC Musculoskelet Disord 16:169
Samim M, Smitaman E, Lawrence D, Moukaddam H (2014) MRI of anterior knee pain. Skeletal Radiol 43:875–893
Schön SN, Afifi FK, Rasch H, Amsler F, Friederich NF, Arnold MP et al (2014) Assessment of in vivo loading history of the patellofemoral joint: a study combining patellar position, tilt, alignment and bone SPECT/CT. Knee Surg Sports Traumatol Arthrosc 22:3039–3046
Singerman R, Davy DT, Goldberg VM (1994) Effects of patella alta and patella infera on patellofemoral contact forces. J Biomech 27:1059–1065
Slevin O, Schmid FA, Schiapparelli F, Rasch H, Hirschmann MT (2018) Increased in vivo patellofemoral loading after total knee arthroplasty in resurfaced patellae. Knee Surg Sports Traumatol Arthrosc 26:1805–1810
van Baar ME, Assendelft WJ, Dekker J, Oostendorp RA, Bijlsma JW (1999) Effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic review of randomized clinical trials. Arthritis Rheum 42:1361–1369
Acknowledgments
The authors would like to thank Oh YJ for his illustration.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
No informed consent was necessary for the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sim, J.A., Na, Y.G., Lee, B.K. et al. Alignment changes after open-wedge high tibial osteotomy result in offloading in the patellofemoral joint: a SPECT/CT analysis. Knee Surg Sports Traumatol Arthrosc 30, 437–446 (2022). https://doi.org/10.1007/s00167-020-06115-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06115-0