Abstract
Purpose
Retinacular restraints have a critical role in patellar tracking, limiting the movement of the patella in the trochlear groove. The medial patellofemoral ligament (MPFL) is probably the main stabilizer against lateral displacement; few studies are focused on MPFL role on patellofemoral kinematics and patellar stability. The main goal of this in vitro study was to analyse the influence of the MPFL on the kinematics of the patellofemoral joint and patellar stability.
Methods
Using a non-image-based navigation system, kinematics and anatomical data of six fresh-frozen specimens were collected. A passive flexion–extension from 0° to 90° and static acquisitions at 0°, 30°, 60° and 90°, with and without 25 N of lateral load, were performed with intact and resected MPFL with a 60 N axial force applied to the isolated quadriceps tendon. Patellar tilt and shift were analysed.
Results
The MPFL intact state showed a shift in medial direction during the first degrees of knee flexion—that disappeared in MPFL resected condition—followed by a lateral shift, similar to that of MPFL resected condition. Tilt analysis showed that patella rotated laterally until 85° of knee flexion for intact MPFL condition and until 70° for resected MPFL condition and after rotated medially. Static tests showed that patellar stability was significantly affected by MPFL resected condition in particular at 30° and 60°.
Conclusions
The MPFL has an aponeurotic nature. It works as a restraint during motion, with an active role under high stress on lateral side, but with a small contribution during neutral knee flexion. Its biomechanical behaviour under loading conditions should be kept into account when performing surgical reconstruction of this ligamentous structure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellar stability is an important element for a correct kinematic behaviour of the patellofemoral (PF) joint and thus for the whole knee function. It depends on several factors such as joint geometry, muscles strength and soft tissues actions [9, 12, 15, 35]. All these aspects converge in a complex mechanism, whose perfect equilibrium is fundamental to allow the correct function of this joint.
Although deeper analyses are required, one possible factor associated with the patellar instability is related to patellofemoral maltracking [2, 8, 17, 37]; this issue consists in an incorrect track of the patella into the trochlear groove that can cause many joint disorders, thus leading to pain and mobility alterations [12, 15, 16].
Retinacular restraints have been demonstrated to have a critical role in patellar tracking, limiting the movement of the patella in the trochlear groove [4, 9]. Among these ligamentous structures, the medial patellofemoral ligament (MPFL)—which originates in the region of the femoral medial epicondyle and attaches to the proximal part of the medial border of the patella—has been reported to be probably the main stabilizer against lateral displacement. Pathologies like lateral patellar dislocation have in fact been found to be strongly related to damage to the MPFL [1, 25, 30]. For these reasons, in the last years, several surgical techniques addressing MPFL reconstruction have been gaining popularity [11, 33]; they are also preferred with respect to conservative methods because they seem to be able to prevent further patellar dislocation [23].
A better comprehension of the contribution of the patellar stabilizing mechanisms, such as ligamentous passive restraints, on the kinematics and stability of the patellofemoral joint, will be therefore extremely useful, concerning both the biomechanical and clinical aspects.
However, at present, there are several works on patellar kinematics [2, 5, 8, 24, 30, 37], but few studies are focused on MPFL role on patellofemoral kinematics and patellar stability [25, 28, 31].
The main goal of this in vitro study was to analyse the influence of the MPFL on the kinematics of the patellofemoral joint; the analysis was performed using a non-image-based navigation system on a cadaveric biomechanical set-up. We specifically hypothesized that the MPFL mainly acts as a passive restraint to abnormal lateral loads, thus influencing patellofemoral stability under loadings. The study was specifically conducted considering intact and resected MPFL conditions, under different loads, thus to better understand the role and the contribution of this ligament also on patellar stability.
Only after a deep biomechanical understanding of the influence of the MPFL, it would be possible to know—from the clinical point of view—which is the most appropriate approach to restore a correct patellofemoral kinematics and stability and to prevent alterations, joint compression and long-term chondral degeneration after reconstruction.
Materials and methods
Six fresh-frozen specimens (two males and four females, three right-sided and three left-sided) with a mean age 50 ± 7 years were obtained for the experimental set-up. Each specimen consisted of the whole lower limb disarticulated at the hip joint, including the musculotendinous and capsular structures. None of the specimens presented evidence of pathology or previous intervention. All specimens were thawed 24 h prior to testing. Before the tests, skin and subcutaneous tissues were dissected 30 cm proximal and distal to the knee, leaving an intact extensor apparatus. The femoral diaphysis was fixed on a rigid support by means of a mechanical clamp, preventing any movement of the femur bone and eliminates femoral anteversion.
The femoral and patellar insertions of the MPFL were defined isolating it from the medial meniscotibial ligament and vastus medialis obliquus (VMO).
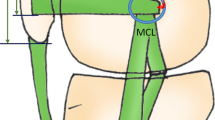
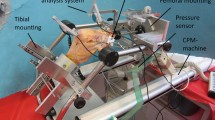
The tibia was free to rotate during passive motion, allowing a range from full extension to 90° of knee flexion (Fig. 1a). During all the tests, a 60 N axial force was applied to the isolated quadriceps tendon via a forceps loaded with weights through a pulley.
Navigation set-up
A commercial navigation system (Klee, BLU-IGS, Orthokey LLC, Lewes, DE, USA) was used to record the tibiofemoral and patellofemoral kinematics; two standard trackers were specifically pinned onto the femur and the tibia, while an additional lighter tracker was screwed into the patella (Fig. 1a), thus avoiding to interfere with patellar tracking. The accuracy, reliability and repeatability of the system for joint kinematic analysis were reported in previous studies [21, 22, 32].
Several landmarks were digitized in order to define the correct anatomical references for the femur, tibia and patella (Fig. 2). On the femur, we specifically identified the centre of the femoral head—estimated by pivoting, the most distal point of the femur (i.e. the femoral notch), the most posterior points of the medial and lateral condyles. Femoral mechanical axis was defined as proximal–distal axis; as reported in literature for the analysis of patella kinematics [2, 5, 25], the line tangent to posterior condyles was used as the mediolateral axis. Medial and lateral malleolus, tibial spine and tibial tuberosity were specifically acquired on the tibia. Mechanical axis of the tibia, defined as the line connecting the mid-point between malleoli and the tibial spine, was the proximodistal axis, whereas the line connecting tibial spine and tibial tuberosity were defined as anteroposterior axis. The proximodistal axis for the patella was defined as the line passing through the upper pole and the lower pole, whereas the mediolateral axis as the line passing through the medial pole and the lateral pole; the origin of the coordinate system was set as the mid-point between the medial and lateral poles.
Acquisition protocol
In order to analyse the kinematics of the patellofemoral joint, a passive flexion–extension from 0° to 90° was performed three times for each specimen, with the intact and the resected MPFL. The tester was aware to maintain the foot in a neutral position during this passive movement.
Furthermore, in order to analyse the influence of the MPFL on the patellar stability, for each specimen a static acquisition was performed without load and with a lateral force of 25 N applied with a dynamometer along medial–lateral axis of patella (Fig. 1b); this test was performed both with the intact and with the resected MPFL, at 0°, 30°, 60° and 90° of flexion. The point of application of the lateral force was marked at the beginning of the experiment in order to have the same point of application.
Data analysis
Patellar tilt and medial–lateral shift of the patella were analysed to understand the MPFL contribution on patellar kinematics. Tilt was evaluated through the tibiofemoral flexion range and was defined as the rotation of the patella along its proximal–distal axis, with respect to the femoral medial–lateral axis. Medial–lateral shift was defined with respect to the tibiofemoral flexion, as the position of the origin of patellar reference system, with respect to femoral reference system calculated on femoral medial–lateral axis (line tangent to posterior condyles). Patellar lateral shift was also used to analyse the stability of the patella under a static load at different knee flexion angle, thus to understand the influence of MPFL on as restraint of patellar lateral displacement. All the evaluations were performed with proprietary routines developed in Matlab (Mathworks, Natick, MA, USA).
Statistical analysis
Starting from the data reported by previous study [21, 27], a priori power analysis for nonparametric Wilcoxon signed-rank test (α = 0.05, power = 0.95, mean difference of 2.0 ± 1.0 mm of displacement and 2.0 ± 1.0° of rotation) indicated a minimum sample size of 6 specimens.
For statistical comparison of kinematic behaviour, continuous data obtained from passive movements were re-sampled each 5° of knee flexion, extrapolating the values from 0° to 90° of knee flexion. Patellar shift and tilt values were then averaged on the three repetitions, at every re-sampled angle, for both MPFL conditions (i.e. intact and resected) for each specimen. The mean values obtained for each specimen were then averaged for the whole set of limbs, thus obtaining one mean curve for the intact condition and one for the resected one.
Differences between intact and resected condition in patellar shift and tilt at every re-sampled angle were tested with Wilcoxon signed-rank test (with Monte Carlo correction for small sample). For statistical comparison of the stability behaviour, the values of shift obtained at 0°, 30°, 60° and 90° of knee flexion were then averaged to compare MPFL intact and resected conditions by means of Wilcoxon signed-rank test (with Monte Carlo correction for small sample). Statistical significance was set at 95 % (p = 0.05). All the statistical tests were performed with SPSS 17 software (SPSS Inc. IBM Corp, USA).
Results
The analysis of neutral position of the patella during PROM, that is the patellar mediolateral position with no stress, normalized to the intact position, showed the following results: the MPFL intact state showed an initial shift of the patella in medial direction between 20° and 25° of flexion and a subsequent lateral shift (Fig. 3). This patellar behaviour, the initial medial shift, disappeared in MPFL resected condition, and the patella showed a slightly lateral shift during all PROM in a similar way of intact state (Fig. 3).
There was high variability in patellar shift until 60° of knee flexion and a reduction in variability between 60° and 90°, both in intact and in resected MPFL state. There was not statistical difference between MPFL intact and resected condition (p > 0.05) for all degrees of PROM.
Tilt analysis in intact MPFL condition showed that patella rotated laterally for all PROM until 85° and after rotated medially (Fig. 4). Resected MPFL condition showed the same behaviour of MPFL intact curve but patella reduced medially after 70° (Fig. 4). Both conditions showed high variability and no statistically significant difference (p > 0.05).
Static tests conducted at different degrees of knee flexion, 0°, 30°, 60° and 90°, under a laterally directed load of 25 N, showed that patellar stability was significantly affected by MPFL resected condition. Medial–lateral laxity was present along all degrees of flexion but is more evident at 30° and 60° (Fig. 5). Lateral load did not affect patellar stability in intact MPFL state (Fig. 5). The inter-specimen variability was high in MPFL cutted condition, especially at 30° and 60°.
Statistical analysis of medial–lateral shift under load showed a significant difference between MPFL resected and intact state both at 30° (p = 0.0274) and at 60° (p = 0.0004) of knee flexion.
Discussion
The most important finding of the present study was the analysis of the kinematic behaviour of the patellofemoral joint and, specifically, of the contribution of the MPFL, that resulted a main restraint against patellar lateral displacement.
The kinematics and the stability of the patellofemoral joint were analysed by means of a navigation system, in a cadaveric set-up, considering both the intact and the MPFL ligament resected knees.
In this study, the medial patellar shift was detectable in MPFL intact state between 20° and 25° of flexion, when the patella engaged the trochlea; subsequently, the patella translated laterally up to 90° of knee flexion. These findings on normal kinematics are comparable to earlier reports [2, 5, 12, 24, 37]. In particular, Amis et al. [2] showed a similar behaviour in normal healthy knees during flexion movement. Starting from full extension, the patella showed a medial translation up to 20° of knee flexion, when the patella engaged the trochlea, followed by a progressive lateral translation up to 90° of knee flexion. The authors described this result as the normal path of the patella when due to its engagement with the trochlear groove and referred to soft tissues—and in particular to the MPFL—the role of contributing as restraint to lateral translation. Brunet et al. [12] showed the same patellar path with an initial medial translation up to 20° of knee flexion, followed by a lateral shift as the flexion angle increased. Also, Nha et al. [24] showed the same behaviour of patellar shift during passive range of motion in an in vivo study. Other authors reported similar results [5, 37], that is, a medial translation in the early degrees of knee flexion, followed by a constant shift value during the remaining arc of flexion.
There is less agreement in literature for what concerns patellar kinematics in the MPFL deficient state [7, 21, 28, 29, 34]. Different studies chose different experimental set-up and this adds further variability to the results.
Some works studied the role of MPFL in patellofemoral joint kinematics focusing their analysis on the ligament strength, analysing its corresponding lengthening using both anatomical and kinematic measurements [1, 13, 14, 35]. Others authors studied the kinematics of MPFL deficient patella only under loading conditions [18, 25].
Few works analysed the role of MPFL, as we did, comparing MPFL intact and resected patella kinematics without using lateral load [27, 31, 34]; according to our results, they suggested that there is no influence of the medial restraints on the patellar tracking in unloaded conditions; in particular, the shift and the tilt presented similar kinematic behaviour with no statistically significant differences.
On the contrary, Ostermeier et al. [28] reported a statistically significant lateral shift of 4.0 mm (SD 2.5 mm) at 9.1° of knee flexion in an unloaded MPFL deficient patellofemoral joint [28]. The contradiction in the statistical results of Ostermeier et al. could be due to some important differences in the experimental set-up: first, the kinematic analysis was based on extension movements—that is, from full flexion to full extension; as reported by Amis et al. [2], this approach could introduce differences in the patellar kinematics with respect to other reported literature. Furthermore, they chose the transepicondylar axis as medial–lateral axis for the femoral reference; as highlighted by previous studies [20, 28], this choice could introduce additional variability in the decomposition of the patellofemoral kinematics. Finally, further incongruence could be due to the detachment of the VMO insertion into the MPFL during dissection.
Data on patellar tilt are more variable and, in contrast to literature, the current study did not note any medial tilt in early flexion when the MPFL was intact [2, 5, 12, 24, 37]. A reduction in lateral tilt was noted after 85° of flexion in both MPFL intact and MPFL deficient knee. Ostermeier et al. reported a similar medial tilt at 102° of flexion [6, 7, 26, 32]. The persistent variability in patellar tilt even after 60° of knee flexion, in contrast to patellar shift, was probably related to the bony anatomical structure.
Intra-group kinematic variability was also higher in the MPFL deficient state as in most studies [7, 21, 28, 29, 34], mainly due to trochlear shape, position of the tibial tubercle and patellar height. In our study, we tried to control these factors via exclusion criteria and the use of the navigation system. Therefore, the variability we obtained, could represent differences related to MPFL insertion, site of MPFL resection and effect of VMO, as reported also in literature [1, 3, 10].
For what concerns patellofemoral stability under loading condition, this study highlighted a more evident difference between MPFL intact and deficient joint. The load applied at 30° and 60° of flexion radically changed the path of patella causing its dislocation. These results showed that the contribution of MPFL in normal healthy knee—without pathological conditions—was closely related to the intervention of external lateral loads that could compromise the stability of the joint [27, 31, 34]. When a laterally directed load was applied in the MPFL deficient state, the peak in lateral patellar shift occurred between 30° and 50° of knee flexion. The effect of the laterally directed load blunted after 60° of knee flexion. The findings were consistent with literature [19, 25]. They probably reflected the peak strain on the MPFL in early flexion [19, 25] and the role of trochlear restraint after 60° of knee flexion [19, 36].
This study has some limitations. The primary is the use of an in vitro model: cadaveric set-up allows only to perform passive movements; thus, in general, it could not exactly replicate the in vivo kinematic behaviour of the joint; in particular, it was not possible to simulate the effect of other active patellar stabilizing mechanisms, such as muscles surrounding the knee, except for the quadriceps contribution. On the other side, this set-up allowed to exactly control the only passive contribution of the MPFL to the patellofemoral kinematics and patellar stability.
The second limitation is that only few specimens were available for tests; therefore, it is possible that the differences in the anatomy and geometry of the recruited specimens may have a role in the variability of results.
The variability of the data could also due to the application of the loading condition, above all for what concerns the load applied on the quadriceps (i.e. through the use of a pulley directly applied on the muscular fibres). Moreover, although the application point of the lateral load was marked, we were not able to exactly control the direction of the applied force. The values of the used forces are, however, in accordance with the ranges we found in literature [2, 25].
From the clinical point of view, this work provided useful information about the biomechanical role of MPFL in the patellofemoral kinematics and stability; this information will be fundamental in suggesting the appropriate surgical approach to restore a correct joint kinematic behaviour, allowing to prevent alterations of the joint stability under loading condition.
Further studies will also keep in consideration joint compression and long-term chondral degeneration after MPFL surgical reconstruction.
Conclusion
This study has underlined that the MPFL has an aponeurotic nature that works as a restraint during motion, with an active role under high stress on lateral side, but low role during neutral knee flexion.
Further studies should focus on in vivo pathological situations to better understand the influence of the bony anatomical abnormalities (patella alta and trochlear dysplasia) on this structure and its kinematic modifications on a dysplastic patellofemoral joint.
References
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10:215–220
Amis AA, Senavongse W, Bull AMJ (2006) Patellofemoral kinematics during knee flexion-extension: an in vitro study. J Orthop Res 24:2201–2211
Amis AA (2007) Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc 15:48–56
Arendt EA (2009) MPFL reconstruction for PF instability. The soft (tissue) approach. Orthop Traumatol Surg Res 95:S97–100
Asano T, Akagi M, Koike K, Nakamura T (2003) In vivo three-dimensional patellar tracking on the femur. Clin Orthop Relat Res 413:222–232
Baldwin JL (2009) The anatomy of the medial patellofemoral ligament. Am J Sports Med 37:2355–2361
Bedi H, Marzo J (2010) The biomechanics of medial patellofemoral ligament repair followed by lateral retinacular release. Am J Sports Med 38:1462–1467
Belvedere C, Catani F, Ensini A, Moctezuma de la Barrera JL, Leardini A (2007) Patellar tracking during total knee arthroplasty: an in vitro feasibility study. Knee Surg Sports Traumatol Arthrosc 15:985–993
Bicos J, Fulkerson JP, Amis A (2007) Current concepts review: the medial patellofemoral ligament. Am J Sports Med 35:484–492
Biedert RM, Netzer P, Gal I, Sigg A, Tscholl PM (2011) The lateral condyle index: a new index for assessing the length of the lateral articular trochlea as predisposing factor for patellar instability. Int Orthop 35:1327–1331
Bitar AC, Demange MK, D’Elia CO, Camanho GL (2012) Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med 40:114–122
Brunet ME, Brinker MR, Cook SD, Christakis P, Fong B, Patron L, O’Connor DP (2003) Patellar tracking during simulated quadriceps contraction. Clin Orthop Relat Res 414:266–275
Conlan T, Garth WPJ, Lemons JE (1993) Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 75:682–693
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM (2007) Surgical biomechanics of the patellofemoral joint. Arthroscopy 23:542–553
Fitzpatrick CK, Baldwin MA, Laz PJ, FitzPatrick DP, Lerner AL, Rullkoetter PJ (2011) Development of a statistical shape model of the patellofemoral joint for investigating relationships between shape and function. J Biomech 44:2446–2452
Fulkerson JP, Shea KP (1990) Disorders of patellofemoral alignment. J Bone Joint Surg Am 72:1424–1429
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
Higuchi T, Arai Y, Takamiya H, Miyamoto T, Tokunaga D, Kubo T (2010) An analysis of the medial patellofemoral ligament length change pattern using open-MRI. Knee Surg Sports Traumatol Arthrosc 18:1470–1475
Jenny J, Boeri C (2004) Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop Scand 75:74–77
Martelli S, Zaffagnini S, Bignozzi S, Bontempi M, Marcacci M (2006) Validation of a new protocol for computer-assisted evaluation of kinematics of double-bundle ACL reconstruction. Clin Biomech (Bristol, Avon) 21:279–287
Martelli S, Lopomo N, Bignozzi S, Zaffagnini S, Visani A (2007) Validation of a new protocol for navigated intraoperative assessment of knee kinematics. Comput Biol Med 37:872–878
Mountney J, Senavongse W, Amis AA, Thomas NP (2005) Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br 87:36–40
Nha KW, Papannagari R, Gill TJ, Van de Velde SK, Freiberg AA, Rubash HE, Li G (2008) In vivo patellar tracking: clinical motions and patellofemoral indices. J Orthop Res 26:1067–1074
Nomura E, Horiuchi Y, Kihara M (2000) Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee 7:121–127
Nomura E, Inoue M, Osada N (2005) Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc 13:510–515
Ostermeier S, Stukenborg-Colsman C, Hurschler C, Wirth C (2006) In vitro investigation of the effect of medial patellofemoral ligament reconstruction and medial tibial tuberosity transfer on lateral patellar stability. Arthroscopy 22:308–319
Ostermeier S, Holst M, Bohnsack M, Hurschler C, Stukenborg-Colsman C, Wirth C (2007) In vitro measurement of patellar kinematics following reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 15:276–285
Parker DA, Alexander JW, Conditt MA, Uzodinma ON, Bryan WJ (2008) Comparison of isometric and anatomic reconstruction of the medial patellofemoral ligament: a cadaveric study. Orthopedics 31:339–343
Philippot R, Chouteau J, Wegrzyn J, Testa R, Fessy MH, Moyen B (2009) Medial patellofemoral ligament anatomy: implications for its surgical reconstruction. Knee Surg Sports Traumatol Arthrosc 17:475–479
Philippot R, Boyer B, Testa R, Farizon F, Moyen B (2012) The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc 20:331–336
Philippot R, Boyer B, Testa R, Farizon F, Moyen B (2012) Study of patellar kinematics after reconstruction of the medial patellofemoral ligament. Clin Biomech (Bristol, Avon) 27:22–26
Sallay PI, Poggi J, Speer KP, Garrett WE (1996) Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med 24:52–60
Sandmeier RH, Burks RT, Bachus KN, Billings A (2000) The effect of reconstruction of the medial patellofemoral ligament on patellar tracking. Am J Sports Med 28:345–349
Senavongse W, Amis AA (2005) The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability: a biomechanical study in vitro. J Bone Joint Surg Br 87:577–582
Thaunat M, Erasmus PJ (2007) The favourable anisometry: an original concept for medial patellofemoral ligament reconstruction. Knee 14:424–428
Yamada Y, Toritsuka Y, Horibe S, Sugamoto K, Yoshikawa H, Shino K (2007) In vivo movement analysis of the patella using a three-dimensional computer model. J Bone Joint Surg Br 89:752–760
Acknowledgments
The authors would like to acknowledge DETERCA, Bordeaux II University (33076—Bordeaux), in particular Pr. Jean Charles Le Huec, and S.B.M Science for biomaterials for their support to conduct the study. SBM Science and biomaterials (Lourdes, France) funded the travel expenses, the specimen retrieval and data elaboration costs for the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zaffagnini, S., Colle, F., Lopomo, N. et al. The influence of medial patellofemoral ligament on patellofemoral joint kinematics and patellar stability. Knee Surg Sports Traumatol Arthrosc 21, 2164–2171 (2013). https://doi.org/10.1007/s00167-012-2307-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2307-9