Abstract
Purpose
The objective of this study was to quantify the amount of ensuing internal rotation of the tibial component when positioned along the medial border of the tibial tubercle, thus establishing a reproducible intraoperative reference for tibial component rotational alignment during total knee arthroplasty (TKA).
Methods
The angle formed from the tibial geometric centre to the intersection of both lines from the middle of the tibial tuberosity and its medial border was measured in 50 patients. The geometric centre was determined on an axial CT slice at 10 mm below the lateral tibial plateau and transposed to a slice at the level of the most prominent part of the tibial tuberosity. Similar measurements were taken in 25 patients after TKA, in order to simulate the intraoperative appearance of the tibia after making its proximal resection.
Results
This angle was found to be similar (n.s.) in normal and post-TKA tibiae [median 20.4° (range 15°–24°) vs. 20.7° (range 16°–25°), respectively]. In 89.3 % of the patients, the angle ranged from 17° to 24°. No statistical difference (p n.s.) was found between women and men in both normal [median −20.7° (range 16°–25°) vs. 19.9° (range 15°–24°)] and post-TKA tibiae [median 21.4° (range 19°–24°) vs. 20° (range 16°–25°)].
Conclusion
This study found that in 90 % of the patients, the medial border of the tibial tuberosity is internally rotated 17°–24° in relation to the line connecting the middle of the tuberosity to the tibial geometric centre. Since this anatomical landmark may be more easily identifiable intraoperatively than the commonly used “medial 1/3”, it can provide a better quantitative reference point and help surgeons achieve a more accurate tibial implant rotational position.
Level of evidence
Cohort and case control studies, Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Long-term clinical success of total knee arthroplasty (TKA) has been reported in the literature with expected ten-year survivorship surpassing 95 % [13]. Unfortunately, a small percentage of patients might still experience clinical failure due to continued knee pain and impaired physical function [13, 29]. Component malrotation refers to alignment of the femoral component in relation to the femoral epicondylar axis, and to the alignment of the tibial base plate relative to the tibial tuberosity. TKA component malrotation has been previously recognized as a possible cause of early onset knee pain, subsequent patient dissatisfaction, and treatment failure following TKA [6, 10, 12, 15, 17, 22].
Tibial base plate alignment is a key component for successful outcomes after TKA, as consequences of malrotation may include patella maltracking [1, 4, 30, 39], flexion and mid-flexion instability [4], synovial and soft tissue impingement, accelerated wear of ultra-high molecular weight polyethylene [23, 30, 42], knee stiffness [35], and abnormal gait patterns [41]. Contrary to the femoral component, which can be verified by various anatomical landmarks such as: the surgical transepicondylar axis or the anterior-posterior line (Whiteside line), the tibial rotational alignment is difficult to readily determine intraoperatively [5, 25, 26, 28, 44].
Current published data support that the tibial component in TKA should be placed in internal rotation not exceeding 18°, in relation to the line connecting the geometrical centre of the proximal tibia and the middle of the tibial tuberosity [6]. Both of these landmarks are difficult to identify intraoperatively. Furthermore, an angle of 18°, from the above line, is practically impossible to assess intraoperatively. Thus, several anatomical references have been suggested to assist in establishing the tibial base plate rotation such as the medial 1/3 of the tibial tuberosity [18], a perpendicular line from the posterior tibial condylar line [27], the mid-sulcus of the tibial spine [9, 33], the transcondylar line of the tibia [11, 45], intermalleolar axis of the ankle, and the axis of the second metatarsal bone [21].
The primary objective of this study was to quantify the amount of the ensuing internal rotation of the tibial component when positioned along the most medial border of the tibial tuberosity. The secondary objective of this study was to examine whether there were any differences in this measurement between genders, since several studies indicated that there were significant differences between males and females in relation to the shape distribution of the proximal tibial plateau morphology [24, 43].
In contrast to the previous described landmarks that are either inaccurate or not easily assessed intraoperatively at the time of tibial component insertion, the medial border of the tibial tuberosity can be readily identified through out surgery.
The hypothesis was that this anatomical landmark can be used as an auxiliary tool for intraoperative tibial component rotational alignment during TKA for both men and women.
Materials and methods
The control cohort included 25 consecutive knee computer tomography (CT) studies of asymptomatic patients 2 years following an uneventful TKA. None of these patients had any complaints of patellofemoral pain, instability, or swelling. The average arc of motion in this cohort was 113°. The cohort included 9 males and 16 females, with an average age of 70 years (range 49–83 years) with preoperative varus malalignment due to primary osteoarthritis. All TKAs were performed by the same surgeon (DB) using the measured resection technique, resecting 10 mm from the tibia below the lateral joint line. All implants were posterior sacrificing fixed bearing with a patellar resurfacing, cemented TKA design (Zimmer, Nexgen, Warsaw, Indiana, USA).
The study group consisted of 50 consecutive non-operated native knee computer tomography (CT) studies from our database. The CT studies were performed as part of an investigation of suspected femoral pathologies such as distal femoral bone cysts, osteochondral defects, ligamentous injuries, and femoral fractures. There were 21 males and 29 females with an average age of 55.3 years (range 19–86 years). Our musculoskeletal radiologist confirmed that all patients in the control group had a normal tibial anatomy, which enabled adequate measurement of the tibial anatomical landmarks.
The asymptomatic post-TKA cohort (control group) was used in order to validate the reliability of the medial border of the tibial tuberosity as a reliable landmark in arthritic patients, who may theoretically present with different tibial anatomy than present in normal individuals.
Radiographic analysis
In order to accurately quantify the ensuing internal rotation of the tibial component, if we aligned the base plate according to the medial border of the tibial tuberosity, we examined the angle created between the lines drawn from the medial border of the tibial tuberosity to the geometric tibial centre, and from the middle of the tibial tuberosity to the geometric tibial centre.
This angle was determined as the tibial component internal rotation angle (TCIRA).
The hypothesis was that the TCIRA will be less than 18°.
In the non-operated group, the measurements were taken at a level of 10 mm below the lateral joint line, mimicking a TKA proximal tibia measured resection technique as described in the CT image analysis section.
In the operated group, the measurements were taken just below the tibial base plate.
These radiographic measurements were taken using an eFilm (Merge Healthcare Headquarters, Chicago, Illinois, USA) program, which is routinely used at our institution.
CT image analysis
-
1.
An axial section parallel to the lateral tibial plateau and placed 10 mm distal to it was created, using an multi-planar reformatting (MPR) reformat. This radiographic modality of the eFilm workstation (Merge Healthcare Headquarters, Chicago, Illinois, USA) allows for accurately passing a plane through a radiographic data set. Thus, it is possible to view and accurately manipulate the image along a different axis than that of the original images (Fig. 1a, b).
Fig. 1 Computed tomography images of the measurement technique used. a A sagittal view showing the position 10 mm distal to the lateral tibial plateau where the axial CT section was taken for measurement. b The axial section acquired from the sagittal measurement that was used for measurements of the MPR reformat for accurate alignment was used for analysis
-
2.
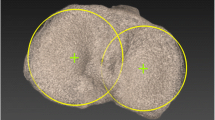
The geometric centre of the tibial plateau at that level which reflects the level of tibial resection during TKA was found using the rectangle (“Rhombus”) method (Fig. 2):
-
On the axial section of the tibial plateau 10 mm below the lateral joint surface, a line connecting the posterior tibial condyles was drawn (line AB).
-
The line was right-clicked, copied, and dragged into its most anterior tibial point (line CD).
-
Perpendicular lines to the line AB (a line connecting the posterior tibial condyles) were drawn tangent to the most lateral and medial tibial boarders (lines AD, and BC).
-
The four vertexes of the rectangle were connected with two diagonals, and their intersection was determined as the geometric centre (point E).
-
A right click was set on both diagonals, and “copy to all images” was performed allowing fixing the geometric centre to all images.
-
-
3.
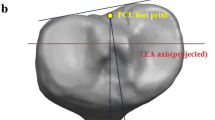
Determining the angle between the line from the tibial geometric centre and the tip of tibial tuberosity and the line from the tibial geometric centre and the medial border of the tibial tuberosity (Fig. 3):
-
The fixed geometric centre was moved further distally to the level of the most prominent point of the tibial tuberosity distal to the insertion of the patellar tendon (point A).
-
A line (line AB) connecting the tibial geometric centre (point A) with the most prominent point of the tip of the tuberosity (point B) was drawn.
-
A line was drawn between the tibial geometric centre (point A) and the medial border of the tibial tuberosity, right at the point where the tibial cortex starts to become denser (point A).
-
The angle (angle BAC) between these two lines was measured and recorded. This angle was determined as the tibial component internal rotation angle (TCIRA).
-
All measurements were taken independently by an orthopaedic surgeon (YK) and a musculoskeletal radiologist (US). These measurements were taken after performing five pilot angle measurements (not included in the study) together using the above-mentioned technique in order to minimize inter-observer errors. The average TCIRA between the measurement of the orthopaedic surgeon and radiologist was recorded for each patient. The TCIRA actually represented the amount of internal rotation of the medial border of the tibial tuberosity compared to its tip. The average between the measured TCIRAs of the orthopaedic surgeon and radiologist was recorded only if the difference was 2° or less. In these 69 (92 %) knees, where the measured TCIRAs were within a 2° difference between observers, we recorded these measurements as an agreed measurement for the interobserver analysis. However, in 6 out of the 75 cases (8 %) where the discrepancy in the TCIRAs was 3° or more, we recorded these measurements as non-agreed measurements for the interobserver analysis. In the non-agreed cases, a subsequent consensus measurement was reached and recorded after reevaluating the measurements by both observers together.
The study was approved by our institutional review board (IRB) University of Toronto, Toronto, Canada, ID approval number—REB 11-0209-C.
Statistical analysis
A chi test was used between the internal rotation of the medial border of the tibial tuberosity angles of the control group and study cohort. In addition, we compared the internal rotation angle between the men and women within the subgroups. A set point of p = 0.05 was determined as statistically significant.
In order to analyse the interobserver correlation, the Cohen Kappa interobserver coefficient was used, based on the measurements mentioned previously in the materials and methods section. Interobserver correlation coefficient values were defined as follow: below 0.40 as poor, between 0.40 and 0.59 as fair, between 0.60 and 0.74 as good, and over 0.74 as excellent [34].
Post hoc power analysis was performed on the control and study group’s data. The power analysis indicated that 25 patients in each group will results in a power of 80 %.
Results
The TCIRA was found to be similar [non-significant (n.s.)] in the non-operated (study) and operated (control, post-TKA) tibias, with a median angle of 20.4° (range 15°–24°) versus a median angle of 20.7° (range 16°–25°), respectively. In 89.3 % of the patients, the TCIRA ranged from 17° to 24°.
No statistical difference (n.s.) was found between women and men in both the non-operated control group with a median of 20.7° (range 16°–25°) versus a median of 19.9° (range 15°–24°), respectively, and the post-TKA cohort tibias with a median of 21.4° (range 19°–24°) versus a median of 20° (range 16°–25°), respectively.
There was an agreement between the radiologist and orthopaedic surgeon within the 2° margin in 69 (92 %) of the 75 knees. The Cohen Kappa coefficient was 0.8 which we considered as excellent. Consequently, the Cohen Kappa interobserver coefficient was 0.8, which is considered as excellent [34].
Discussion
The most important finding of the present study was the ability to use the medial border of the tibial tuberosity as an intraoperative land mark during TKA surgery, surgeons with an auxiliary tool that enabling further fine-tuning for accurate tibial component rotational alignment.
Several anatomical references have been used in the past to determine tibial base plate rotational position such as: the medial 1/3 of the tibial tuberosity [18], the posterior condylar line of the tibia [27], the mid-sulcus of the tibial spine [9, 33], the transcondylar line of the tibia [11, 45], the intermalleolar axis of the ankle, and the axis of the second metatarsal bone [21]. However, a previous publication reported that the medial 1/3 of the tibial tuberosity might be too externally rotated in aligning the tibial component in TKA [9, 37]. Moreover, the posterior condylar line of the tibia, the mid-sulcus of the tibial spine, and the transcondylar line of the tibia would be susceptible to osteophyte formation and bone loss of the tibial articular surface in patients with OA, thus making it harder to accurately identify these anatomical landmarks intraoperatively [27]. In addition, the intermalleolar axis of the ankle and the axis of the second metatarsal bone would be susceptible to deformities and positioning of the ankle and foot. In contrast, the AP axis shown by Akagi et al. [2, 3] would not be influenced by articular deformity and would be perpendicular to the surgical epicondylar axis in both healthy knees and osteoarthritic knees [20]. Yet, when reaching the stage of tibial plateau preparation, during TKA, the Akagi landmark is already absent, and if not reliably marked previously before the proximal tibial resection is completed it cannot be used.
Consequently, tibial component rotational alignment may not be as readily determined intraoperatively as the femoral component rotation due to the lack of existing landmarks at the actual time of tibial component preparation. Subsequently, excessive internal tibial rotation may occur and lead to patella maltracking [1, 4, 7, 30, 39], flexion and mid-flexion instability [4], synovial and soft tissue impingement, accelerated wear of ultra-high molecular weight polyethylene [23, 30, 42], knee stiffness [35], and abnormal gait patterns [41]. The reason for this detrimental effect may be related to the increased biomechanical forces induced by anteroposterior translations [36]. These increased forces can be somewhat moderated by using a rotating platform tibial base plate that can decrease the patellofemoral shear forces induced by femoral component internal rotation in flexion [8, 40].
Berger et al. found that the tibial component in TKA should be placed in internal rotation not exceeding 18°, in relation to the line connecting the geometrical centre of the proximal tibia and the middle of the tibial tuberosity [6]. However, both of these landmarks are difficult to identify intraoperatively. Furthermore, an angle of 18° is practically impossible to assess intraoperatively by eyeballing.
Based on this study, in 90 % of the patients, alignment of the tibial component to the medial border of the tibial tuberosity will place the tibial base plate in 17°–24° of internal rotation in relation to the line connecting the geometrical centre of the proximal tibia and the middle of the tibial tuberosity. Consequently, the surgeon will need only to “fine-tune” the tibial component rotation with ancillary measures to overcome the possible resulting internal rotation of 6°.
The data in this study indicate that this principle can be applied similarly both in men and in women. The lack of difference between the genders regarding the proximal tibial morphology corresponds to the findings of Hartel et al. [14] that found similar findings in a study analysing 237 proximal tibia MRI exams rather than the studies performed in oriental population [24, 43].
After aseptic loosening and infection, the third most common cause for TKA revision surgery is knee pain (10 %), while the fourth cause is patellofemoral pain (10 %). Data from the Australian Joint Registry suggest that a significant group of patients as much as 20 % of all revision TKA cases underwent revision TKA for non-defined post-operative knee pain. TKA component malrotation has previously been recognized as an early onset cause for pain after primary TKA [6, 10, 12, 15, 17, 22] and may be the reason for a substantial part of those 20 % revision TKAs performed for non-defined post-operative knee pain as component malrotation is not easily demonstrated by plain radiographs [6, 19, 22, 38].
Component malrotation in TKA refers to the femoral component position relative to the femoral epicondylar axis, while tibial rotation refers to the position of the tibial base plate relative to the tibial tuberosity. Subtle internal rotation of the femoral and tibial components can only be accurately measured using a CT scan [6, 19, 22, 38] and may be difficult to determine intraoperatively without a computer-assisted surgical navigation system or patient-specific instrumentation, which have their own shortcomings such as cost and surgical operating room time [31, 32].
The finding in this study shows that the medial border of the tibial tuberosity as an intraoperative land mark will result in a TCIRA of 17°–24° of internal rotation in 90 % of the patients. These data can provide surgeons with an auxiliary tool that allows supplementary fine-tuning for accurate tibial component rotational alignment. Howell et al. [16] performed a virtual magnetic resonance image of tibial anatomy. They found that the medial third of the tibial tuberosity was too externally rotated for referencing tibial component rotational alignment. Instead, they recommend to use the medial border of the tibial tuberosity which is 0–6 mm from the AP axis, which actually corresponds with our findings.
There are several limitations to this study. First, we evaluated a limited number of varus knees and as such our data may not include the entire spectrum of patients. However, the standard deviations of the measurements were all small enough to use the internal rotation angle as the anterior reference point in aligning the tibial component. Second, the non-operative cohort lacks post-operative CT rotation measurements of the tibial component and does not have the entire clinical post-operative data in these patients. Yet, this limitation is balanced by the control group (the operated patients) which shows that when the tibial component was aligned along the medial border of the tibial tuberosity the clinical outcome was favourable. The third limitation regarding the data of the control (operated) group is that the data are essentially limited to clinical data and do not include gait analysis parameters. The fourth limitation which could further enhance the validity of our findings is the retrospective nature of this study. A better study design would include a preoperative and post-operative CT in patients undergoing TKA in order to better validate our findings.
Conclusion
The current study provides knee surgeons with a cost-effective quantitative reference point to assist them with proper rotation of the tibial base plate intraoperatively. The reported reference point of the TCIRA together with routine intraoperative ancillary measurements may help arthroplasty surgeons to better assess the rotation of the tibial component and achieve proper positioning of the tibial base plate. This may allow a lower rate of tibial component outliers and possibly decrease the rate of patellar maltracking and revision TKA [5].
References
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 366:155–163
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C (2005) Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res 436:172–176
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Cinotti G, Sessa P, Rocca AD, Ripani FR, Giannicola G (2013) Effects of tibial torsion on distal alignment of extramedullary instrumentation in total knee arthroplasty. Acta Orthop 84(3):275–279
Colwell CW Jr, Chen PC, D’Lima D (2011) Extensor malalignment arising from femoral component malrotation in knee arthroplasty: effect of rotating-bearing. Clin Biomech (Bristol, Avon) 26:52–57
Dalury DF (2001) Observations of the proximal tibia in total knee arthroplasty. Clin Orthop Relat Res 389:150–155
Drexler M, Dwyer T, Chakravertty R, Farno A, Backstein D (2013) Assuring the happy total knee replacement patient. Bone Joint J 95-B:120–123
Eckhoff DG, Johnston RJ, Stamm ER, Kilcoyne RF, Wiedel JD (1994) Version of the osteoarthritic knee. J Arthroplasty 9:73–79
Eckhoff DG, Metzger RG, Vandewalle MV (1995) Malrotation associated with implant alignment technique in total knee arthroplasty. Clin Orthop Relat Res 321:28–31
Graves S, Davidson D, de Steiger R (2011) Australian Orthopaedic Association National Joint Replacement Registry Annual Report for 2011
Hartel MJ, Loosli Y, Gralla J, Kohl S, Hoppe S, Roder C, Eggli S (2009) The mean anatomical shape of the tibial plateau at the knee arthroplasty resection level: an investigation using MRI. Knee 16:452–457
Hofmann S, Romero J, Roth-Schiffl E, Albrecht T (2003) Rotational malalignment of the components may cause chronic pain or early failure in total knee arthroplasty. Orthopade 32:469–476
Howell SM, Chen J, Hull ML (2013) Variability of the location of the tibial tubercle affects the rotational alignment of the tibial component in kinematically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2288–2295
Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD (2007) Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res 458:131–136
Insall JN (1993) Surgical techniques and instrumentation in total knee arthroplasty. In: Insall JN, Windsor RE, Scott WN, Kelly M, Aglietti P (eds) Surgery of the knee, 2nd edn. Churchill livingstone, New York, pp 739–804
Jazrawi LM, Birdzell L, Kummer FJ, Di Cesare PE (2000) The accuracy of computed tomography for determining femoral and tibial total knee arthroplasty component rotation. J Arthroplasty 15:761–766
Kawahara S, Matsuda S, Okazaki K, Tashiro Y, Mitsuyasu H, Nakahara H, Iwamoto Y (2012) Relationship between the tibial anteroposterior axis and the surgical epicondylar axis in varus and valgus knees. Knee Surg Sports Traumatol Arthrosc 20:2077–2081
Kawahara S, Okazaki K, Matsuda S, Mitsuyasu H, Nakahara H, Okamoto S, Iwamoto Y (2014) Medial sixth of the patellar tendon at the tibial attachment is useful for the anterior reference in rotational alignment of the tibial component. Knee Surg Sports Traumatol Arthrosc 22:1070–1075
Lakstein D, Zarrabian M, Kosashvili Y, Safir O, Gross AE, Backstein D (2010) Revision total knee arthroplasty for component malrotation is highly beneficial: a case control study. J Arthroplasty 25:1047–1052
Lewis P, Rorabeck CH, Bourne RB, Devane P (1994) Posteromedial tibial polyethylene failure in total knee replacements. Clin Orthop Relat Res 299:11–17
Li P, Tsai TY, Li JS, Zhang Y, Kwon YM, Rubash HE, Li G (2014) Morphological measurement of the knee: race and sex effects. Acta Orthop Belg 80:260–268
Mantas JP, Bloebaum RD, Skedros JG, Hofmann AA (1992) Implications of reference axes used for rotational alignment of the femoral component in primary and revision knee arthroplasty. J Arthroplasty 7:531–535
Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE (2001) Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res 392:38–45
Moreland JR (1988) Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res 226:49–64
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 69:745–749
Mortazavi SM, Molligan J, Austin MS, Purtill JJ, Hozack WJ, Parvizi J (2011) Failure following revision total knee arthroplasty: infection is the major cause. Int Orthop 35:1157–1164
Nagamine R, Whiteside LA, White SE, McCarthy DS (1994) Patellar tracking after total knee arthroplasty. The effect of tibial tray malrotation and articular surface configuration. Clin Orthop Relat Res 304:262–271
Ollivier M, Tribot-Laspiere Q, Amzallag J, Boisrenoult P, Pujol N, Beaufils P (2015) Abnormal rate of intraoperative and postoperative implant positioning outliers using “MRI-based patient-specific” compared to “computer assisted” instrumentation in total knee replacement. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3645-1
Roberts TD, Clatworthy MG, Frampton CM, Young SW (2015) Does computer assisted navigation improve functional outcomes and implant survivability after total knee arthroplasty? J Arthroplasty 30:59–63
Sahin N, Atici T, Kurtoglu U, Turgut A, Ozkaya G, Ozkan Y (2013) Centre of the posterior cruciate ligament and the sulcus between tubercle spines are reliable landmarks for tibial component placement. Knee Surg Sports Traumatol Arthrosc 21:2384–2391
Streiner DL, Norman GR (1995) Health measurement scales: a practical guide to their development and use. Oxford University Press, New York
Su EP, Su SL, Della Valle AG (2010) Stiffness after TKR: how to avoid repeat surgery. Orthopedics 33:658-20100722-48
Thompson JA, Hast MW, Granger JF, Piazza SJ, Siston RA (2011) Biomechanical effects of total knee arthroplasty component malrotation: a computational simulation. J Orthop Res 29:969–975
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y (2002) Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 402:196–201
van der Linden-van der Zwaag HM, Bos J, van der Heide HJ, Nelissen RG (2011) A computed tomography based study on rotational alignment accuracy of the femoral component in total knee arthroplasty using computer-assisted orthopaedic surgery. Int Orthop 35:845–850
van Gennip S, Schimmel JJ, van Hellemondt GG, Defoort KC, Wymenga AB (2014) Medial patellofemoral ligament reconstruction for patellar maltracking following total knee arthroplasty is effective. Knee Surg Sports Traumatol Arthrosc 22(10):2569–2573
Vanbiervliet J, Bellemans J, Verlinden C, Luyckx JP, Labey L, Innocenti B, Vandenneucker H (2011) The influence of malrotation and femoral component material on patellofemoral wear during gait. J Bone Joint Surg Br 93:1348–1354
Verlinden C, Uvin P, Labey L, Luyckx JP, Bellemans J, Vandenneucker H (2010) The influence of malrotation of the femoral component in total knee replacement on the mechanics of patellofemoral contact during gait: an in vitro biomechanical study. J Bone Joint Surg Br 92:737–742
Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG (1994) Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res 299:31–43
Yang B, Song CH, Yu JK, Yang YQ, Gong X, Chen LX, Wang YJ, Wang J (2014) Intraoperative anthropometric measurements of tibial morphology: comparisons with the dimensions of current tibial implants. Knee Surg Sports Traumatol Arthrosc 22:2924–2930
Yoshioka Y, Siu D, Cooke TD (1987) The anatomy and functional axes of the femur. J Bone Joint Surg Am 69:873–880
Yoshioka Y, Siu DW, Scudamore RA, Cooke TD (1989) Tibial anatomy and functional axes. J Orthop Res 7:132–137
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Drexler, M., Backstein, D., Studler, U. et al. The medial border of the tibial tuberosity as an auxiliary tool for tibial component rotational alignment during total knee arthroplasty (TKA). Knee Surg Sports Traumatol Arthrosc 25, 1736–1742 (2017). https://doi.org/10.1007/s00167-016-4072-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4072-7