Abstract
Purpose
The purpose of the present study was to determine whether the axes aligned with the sulcus between the tibial spines and the middle of the posterior cruciate ligament at the knee and with the tibialis anterior tendon at the ankle provide a neutral rotational and coronal alignment of the tibial component in total knee arthroplasty (TKA).
Methods
In a cohort of 45 TKA patients, CT scans were taken to quantify coronal and rotational positioning of the components. All patients received a posterior stabilised total knee replacement with a fixed insert (PFC Sigma; DePuy Orthopaedics, Inc; Warsaw, IN, USA). The tibial guide was aligned with the sulcus between the tibial spines and the middle of the posterior cruciate ligament at the knee and with the tibialis anterior tendon at the ankle.
Results
The average post-operative coronal mechanical alignment was 1° varus (range 4.5° varus–1.5° valgus; SD ±1.51). The average post-operative rotational deviation from the transepicondylar axes (TEA) was 0.78° of internal rotation (1.50° of internal rotation − 3.5° of external rotation) for the tibial component. The whole-extremity mechanical axis deviation was outside the tolerance range of 3° in 4 patients (8.9 %). Deviation of the tibial component rotational position relative to the TEA was 3° or less in 94.5 % of the patients.
Conclusions
When the tibial component is aligned using the axis drawn from the centre of the PCL to the sulcus between the tibial spines on the proximal tibia and to the tibialis anterior tendon at the ankle, good alignment will be achieved in both the coronal and axial planes.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A significant improvement in function and pain relief following total knee arthroplasty (TKA) in the vast majority of patients is well documented in the literature. Optimal implant positioning and precise reconstruction of the leg mechanical axis are necessary for good results [10, 24]. Malalignment is the main reason for early failures related to instability and patellofemoral complications and for longer-term failures related to polyethylene wear and inadequate fixation [10, 26]. The consequences of malalignment greater than 3° in the coronal plane are well understood, with numerous reports demonstrating a relationship between varus limb alignment and medial compartment overload, radiolucent lines and implant failure due to medial bone collapse [5, 16, 20]. Although a small degree of combined internal rotation (1°–4°) is associated with lateral tracking and inclination of the patella in the axial plane of the femoral and tibial components, a large degree of internal rotation (7°–17°) is associated with patellar dislocation and loosening of the patellar prosthesis [6].
Optimal alignment and appropriate implant sizing and positioning can be achieved using traditional jigs and alignment guides or through the use of computer navigation. In the coronal plane, most surgeons attempt to create distal femoral valgus of 4°–7° with neutral alignment of the proximal tibia [14]. As the femoral transepicondylar axis (TEA) has been shown to be close to the knee flexion–extension axis [8], it is generally desirable to locate the component parallel to this axis in the axial plane. When determining component rotation, the measured resection technique is used on the femoral side. Typically, the femoral posterior condyles [19], Whiteside’s line [32] and TEA are used [7]. There is no consensus on defined reference points with which to determine the rotational position of the tibial component compared with the femur [1, 3, 4, 19, 22, 23, 30, 34]. The tibial posterior condylar line [23], the tibial transcondylar line [34], the medial third of the tibial tubercle [19], Akagi’s line [2], the ankle transmalleolar axis [3], the axis of the anterior tibial crest [12] and the second metatarsal [3] are known examples of tibial markers.
The hypothesis of this study is that in primary TKA, when the rotational position of the tibial component is defined according to the anteroposterior axis of the tibia with the axis drawn from the middle of the posterior cruciate ligament seen at the posterior notch to the tibial sulcus, the alignment can run parallel to the TEA. Appropriate alignment of the tibial component in the coronal plane can be achieved when determined according to the line joining the middle of the tibialis anterior tendon at the level of the ankle to the anterior extension of the tibial anteroposterior axis. To the best of our knowledge, there are no published studies on the analysis by CT of the component coronal and rotational position following placement of the tibial component using these anatomical landmarks. This study analysed the coronal and axial positions of tibial component by CT placed according to centre of the posterior cruciate ligament, the sulcus between tubercle spines and tibialis anterior tendon.
Materials and methods
In this prospective clinical cohort study, 95 consecutive patients with primary osteoarthritis who underwent primary TKA by the same surgeon using the same technique were evaluated between September 2007 and April 2009. The inclusion criterion was the presence of primary varus osteoarthritis of the knee. Patients who had undergone previous surgery on the joint were excluded. Nineteen patients with a flexion contracture greater than 10° were not included in the study because this condition would have resulted in an altered reciprocal rotational position between the femur and the tibia. Another five patients were excluded because the femur medial epicondylar sulcus could not be defined on the knee CT axial section. A random-number generator was used to invite patients to participate in the study until the target number of patients defined by the power analysis was reached. The study comprised 45 knees from 45 patients (34 female, 11 male) with a mean age of 65.8 (±6.3) years. Of these patients, three who were undergoing bilateral TKA but had previously undergone unilateral knee surgery were included in the study. The lateral femorotibial angle as determined by the preoperative standing radiographs was 189.1° (±4.1). The coronal and axial positions of the femoral and tibial components were determined by CT images of the knees on which TKA was to be performed. The follow-up period averaged 25.5 months (range 20–32 months). Informed consent was obtained from all patients participating in the study, and the study was approved by the local ethics committee.
Radiological examination
A Siemens Somatom Spirit CT scanner (Siemens A.G. Medical Solutions, Forchheim, Germany) was used for all scans. The patient was placed in the supine position on the scanning table with the affected leg in full extension. We acquired a post-operative, anteroposterior scanogram with a field of view extending from the hip to the ankle. A scout view was obtained. To obtain scans perpendicular to the long axis of the leg, the scanner’s gantry was tilted based on the lateral scout view. CT images 2 mm in thickness and 1.5 mm in Recon increment were taken of the area extending from the femoral distal metaphysis to the tibial tubercle. The image reconstruction was performed using both bone and soft-tissue filters. Field parameters were not changed during reconstruction to allow image superimposition. For this step, the surgeon simulated a weight-bearing condition with full extension of the patient’s knee. CT data were analysed using Syngo viewing software (Siemens A.G. Medical Solutions, Forchheim, Germany).
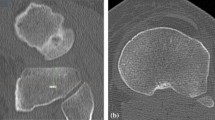
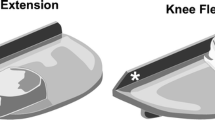
Surgical technique
A posterior stabilised total knee replacement with a fixed insert (P.F.C. Sigma; DePuy Orthopaedics, Inc; Warsaw, IN, USA) was implanted with cement in all patients. Femoral intramedullary and tibial extramedullary alignment guides were used for implantation. The first step of the implantation process was preparation of the tibia [14]. The tibial guide was aligned with the sulcus between the tibial spines and the middle of the posterior cruciate ligament at the knee and with the tibialis anterior tendon at the ankle, which created neutral coronal alignment (Fig. 1a, b). The tibial cut was made so that 8–10 mm of bone was removed from the lateral tibial plateau. The tibia was sized based on the AP dimension of the lateral tibial plateau, by selecting the size that best covered the lateral plateau without overhang. The tibial component was centred on the lateral plateau and externally rotated until the middle of the component was aligned with the AP between the tibial spines and the middle of the posterior cruciate ligament. On the femoral side, the rotational alignment was approximated using 3° of external rotation from the posterior condylar axis.
The reference points used for tibial guide placement. a The preferred reference points for tibial component placement were the sulcus between the tibial spines (star) and the middle of the posterior cruciate ligament (triangle) at the knee and the tibialis anterior tendon (arrow) at the ankle. b After placement of the tibial guide according to the reference points
Clinical evaluation
At the preoperative and final examinations, the range of motion was measured, and the Knee Society score was calculated.
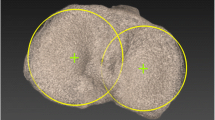
Evaluation of alignment and rotation
The femoral mechanical axis was defined as the connecting line between the centre of the femoral head and the centre of the knee. The tibial mechanical axis was the line connecting the centre of the ankle and the centre of the knee (Fig. 2). The rotational deviation of the femoral component from the referenced axis was determined by the angle between the line connecting the posterior femoral component line and the surgical epicondylar axis (Fig. 3). The tibial rotational error was defined as the angle between the angle bisecting the line of the posterior tibial component line and the transposed epicondylar axis (Fig. 4). On the basis of the spatial relationship between the femoral and tibial components and the femoral and tibial mechanical axis, the following angles were determined: the varus or valgus position of the femoral component relative to the femoral mechanical axis, the varus or valgus position of the tibial component relative to the tibial mechanical axis, the varus or valgus position of the entire limb as the sum of the tibial and femoral mechanical axes, the rotational deviation of the femoral component from the epicondylar axis and the rotational deviation of the tibial component from the epicondylar axis.
Anteroposterior scanogram with a field of view from the hip to the ankle. The mechanical axis of the femur was a line joining the mid-point of the femur at the joint line and the centre of the femoral head (line a). The mechanical axis of the tibia was a line joining the mid-point of the tibia at the joint line and the centre of the talus. The long leg view shows the limb has a 1° varus position of the entire limb as the sum of the tibial and femoral mechanical axes
The CT scan measurement technique for the femoral rotation angle is shown. A CT scan shows the medial and lateral epicondyles on the distal femur. The PCL line connects the posterior surfaces of the prosthetic posterior condyles, depicting the position of the component. The horizontal line in the middle of the figure connects the medial and lateral epicondyles, defining the transepicondylar axis (TEA). The PCL line is recopied closer to the TEA (PCL′) to facilitate measurement of the angle between the component and the TEA, in this patient 3° of internal rotation
The CT scan measurement technique for the tibial rotation angle is shown. The PL line connects the posterior surface of the prosthetic posterior condyles, depicting the position of the component. The TEA is transposed to the tibial scan (TEA′) to facilitate measurement of the angle between the component and the TEA, in this patient 2 of internal rotation
All measurements were repeated by two independent observers. The mean values of the two observers’ measurements were used for analysis. The first observer repeated all the radiological measurements after 1 week for test–retest reliability measurement.
Statistical analysis
On the basis of the power analysis conducted before the study, which was derived from conservative estimates from previous studies [2, 3, 10, 20, 29, 30], we assumed that our technique would have a standard deviation of 7° with the assumption that a total of 45 measurements would be required for our technique to achieve an a priori statistical power of 0.80 to detect a 3° difference from 0°. The intraclass correlation coefficient was calculated to evaluate measurement consistency. A test–retest was performed for intra-observer reliability with the first observer taking the first measurement again 1 week later in all cases. The mean value of repeated measurements was calculated. A Wilcoxon signed-rank test was used to compare preoperative and post-operative measurements of knee scores and functional scores. The median (min:max) was used as a descriptive value. Correlation analysis was performed using the Pearson correlation coefficient. p < 0.05 was accepted as statistically significant.
Results
Relative to the femoral mechanical axis, the average femoral component coronal position was 0.38° (±1.2) varus. Relative to the tibial mechanical axis, the tibial component coronal position averaged 0.38° varus (±1.3). The coronal position of the whole extremity was determined as the mean 1° varus (±1.5) (Fig. 5). The mean rotational deviation of the femoral component from the epicondylar axis was 0.7° of internal rotation (±0.7) (Fig. 6), and the mean rotational deviation of the tibial component from the epicondylar axis was 0.9° of internal rotation (±1.1) (Fig. 7). In all patients, the coronal alignment of the femoral component ranged between 3° of internal rotation and 3° of external rotation.
There was a deviation in the coronal plane of the tibial component position outside the tolerance range of 3° in 4 patients (8.9 %). In 91.1 % of the patients, whole-extremity post-operative mechanical axes of between 3° varus and 1° valgus were achieved. Post-operative full mechanical axis deviation of more than 3° was determined in 4 patients (8.9 %). The rotational position deviation of the femoral component relative to the TEA was more than 3° in 2 patients (4.4 %). The rotational position deviation of the tibial component relative to the TEA was more than 3° in 2.5 patients (5.5 %). At the end of the follow-up period, the mean knee scores had risen from preoperative 40.1 (±10.1) to post-operative 87 (±10.5) (p < 0.01). The mean functional knee scores rose from preoperative 48 (±7.9) to post-operative 78 (±11.9) (p < 0.01).
Although there was a negative correlation between the preoperative lateral femorotibial angle and post-operative knee score (r = −0.462, p = 0.001) and post-operative functional knee score (r = −0.459, p = 0.002), there were no negative correlations among any of the other parameters. A positive correlation between the tibial component rotational position and the post-operative mechanical axis was observed (r = 0.320, p = 0.032).
Whereas the interobserver correlation coefficient was high for the post-operative mechanical axis, the femoral component coronal alignment and the tibial component coronal alignment, low values were found for femoral component rotation and tibial component rotation. Nonetheless, the interobserver errors in the measurement of rotational deformity with respect to rotational alignment of the femoral and tibial components were small irrespective of the reference lines (between 4° of internal rotation and 4° of external rotation). The intra-observer correlation coefficient was high for all measurements (Table 1).
Discussion
The most important finding of the present study was that when the tibial guide is aligned with the sulcus between the tibial spines, the middle of the posterior cruciate ligament and tibialis anterior tendon, it may be possible to create neutral coronal and rotational alignment of the tibial component in TKA. The classic application on the femoral side can achieve alignment within a safe margin when taking an intramedullary guide in the coronal plane and posterior condyles as references in the axial plane. Although a preoperative large varus deformity has been shown to have a negative effect on early post-operative knee scores, no relationship has been observed between component position and early post-operative knee scores.
As the number of TKA operations increases, it becomes more important to have reliable techniques to achieve the correct rotational positioning of the components. Each of the methods used to achieve correct alignment has its own advantages and disadvantages, and some of these methods have been shown to have a low rate of interindividual reproducibility [17, 23, 29]. The traditional methods used on the tibial side were ‘classic,’ involving the medial one-third of the tibial tubercle [11] or self-alignment of a conforming mobile tibial insert in extension [21]. Comparative studies [11] have demonstrated the difficulties encountered in achieving the desired rotation relative to the TEA, typically yielding outliers with abnormal external or internal rotation [11, 18, 23, 31]. Ikeuchi et al. [18] reported a greater likelihood of tibial component internal rotation with the self-aligning method. In a study by Uehara et al. [31] on TKA for varus osteoarthritis, preoperative CTs were taken. In the 12 % of cases where the medial third of the tibial tuberosity was taken as reference, a rotational mismatch of more than 10° relative to the TEA was found. Sun et al. [28] showed that the tibial tubercle was not a reliable rotational landmark for the tibial tray in osteoarthritic knees with varus or valgus deformity. In a cadaver study, Rossi et al. [25] compared the flexion–extension technique with techniques where the tibial tray is placed fully in the posterolateral and anteromedial corners of the tibia. The authors emphasised that the flexion–extension and posterolateral corner locked techniques are both precise and reproducible methods with which to assess tibial component rotation during TKA. However, the authors stated that although the flexion–extension technique was dependent on correct positioning of the femoral component and soft-tissue balancing, the posterolateral corner locked method was easier if a complete visualisation of the posterolateral corner of the cut tibial plateau was achieved. In recent years, preoperative CT scanning methods have come into use to appropriately align component rotations [2, 33]. Akagi et al. [2] defined a new anteroposterior axis in the proximal tibia, which is the line connecting the mid-posterior cruciate ligament attachment to the medial border of the tibial plateau. This axis is perpendicular to the femoral TEA. Therefore, the axis reference of Akagi et al. [2] on the tibia should also consider the femoral TEA. Cobb et al. [9] reported that an anatomical axis created perpendicular to the line joining medial and lateral tibial centres is more reliable than either the posterior surfaces of tibial condyles or any axis involving the tibial tubercle. However, it is unclear whether routine preoperative CT scanning is a useful tool with which to improve positioning.
Most investigators have demonstrated that total knee replacements implanted with computer-assisted navigation have more accurate component alignment especially on the coronal and sagittal planes, on the basis of plain radiographs, compared with those implanted conventionally (13, 15). However, short-term clinical studies have not shown improved clinical outcomes attributable to the use of navigation. Matziolis et al. [21] showed that computer-assisted implantation of total knee replacements improved the frontal and sagittal alignment of the femoral component but not of the tibial component. Moreover, the rotational alignment of the component was not improved through navigation by solely referencing the epicondylar axis for the femur and the tuberosity for the tibia. The landmarks (tibial tuberosity and centre of the tibia) selected by Matziolis et al. [21] to determine tibial component rotation showed a high rate of variance. Siston et al. [27] demonstrated in a cadaver study that a navigation system that relies on the digitisation of landmarks to establish a rotational alignment axis does not provide a more reliable means of rotational alignment than does the use of traditional TKA instrumentation.
By considering the external rotation in the ankle, the anteroposterior axis of the proximal tibia, which is the axis least affected by the deformity, and the centre of the tibialis anterior tendon were selected for use as anatomic reference points for component placement. The result of this coronal alignment of the components, as in previously applied classical and computerised methods, was that more than 90 % of the components were inside the tolerance range of 3° of deviation. However, the major finding of this study is that relative to the TEA, tibial component rotational alignment was achieved within a 3° deviation in 94.5 % of the patients. With the method used in this study to achieve correct alignment, despite the high level of interindividual reproducibility in defining the post-operative mechanical axis, the femoral component axis and the tibial component axis in the coronal plane, the values for femoral component rotation and tibial component rotation were found to be low. However, for rotational alignment of the femoral and tibial components, the interobserver errors in measurement of rotational deformity were small (4° of internal rotation − 4° of external rotation) irrespective of the reference lines. Additionally, when the 2 observers were evaluated separately, more than 90 % of the component rotational alignment was seen to be between 3° of internal rotation and 3° of external rotation.
One of the limitations of the present study is the small number of cases. As the operations were performed by a single surgeon, interobserver reliability could not be evaluated. Another limitation of the study is the lack of comparison of the technique used with any other conventional or computerised technique. Furthermore, the follow-up period was not sufficient to determine whether there was any difference in Knee Society scores over the long term.
In TKA surgery, the use of referred anteroposterior axis of the proximal tibia is a safer method of avoiding excessive internal or external rotation of tibial component. In addition, when the referred anteroposterior axis is combined with the tibialis anterior tendon at the level of the ankle joint, coronal alignment of tibial component may be provided in a safe range without using any computerised method.
Conclusions
It can be concluded that in conventional TKA, the successful use of jigs and alignment guides requires attention to specific anatomic landmarks. With the classic intramedullary guide for the coronal position of the femoral component together with rotational positioning according to the posterior femoral condyles, good alignment of the tibial component can be achieved when defined according to the axis drawn from the centre of the PCL on the tibial proximal joint surface to the tibial sulcus and the axis drawn to the centre of the tibialis anterior tendon distally.
References
Aglietti P, Sensi L, Cuomo P, Ciardullo A (2008) Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res 466:2751–2755
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C (2005) Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res 436:172–176
Bae DK, Song SJ (2011) Computer assisted navigation in knee arthroplasty. Clin Orthop Surg 3(4):259–267
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 356:111–118
Cobb JP, Dixon H, Dandachli W, Iranpour F (2008) The anatomical tibial axis: reliable rotational orientation in knee replacement. J Bone Joint Surg Br 90:1032–1038
Czurda T, Fennema P, Baumgartner M, Ritschl P (2010) The association between component malalignment and post-operative pain following navigation-assisted total knee arthroplasty: results of a cohort/nested case-control study. Knee Surg Sports Traumatol Arthrosc 18:863–869
Eckhoff DG, Metzger RG, Vandewalle MV (1995) Malrotation associated with implant alignment technique in total knee arthroplasty. Clin Orthop Relat Res 321:28–31
Fukagawa S, Matsuda S, Mitsuyasu H, Miura H, Okazaki K, Tashiro Y, Iwamoto Y (2011) Anterior border of the tibia as a landmark for extramedullary alignment guide in total knee arthroplasty for varus knees. J Orthop Res 29:919–924
Haaker RG, Stockheim M, Kamp M, Proff G, Breitenfelder J, Ottersbach A (2005) Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res 433:152–159
Hepinstall MS, Ranawat AS (2008) Knee reconstruction. Landmarks for optimizing component position in total knee arthroplasty. Current Orthopaedic Practice 19:147–154
Hetaimish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK (2012) Meta-analysis of navigation vs conventional total knee arthroplasty. J Arthroplasty. doi:10.1016/j.arth.2011.12.028
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg Br 73:709–714
Jerosch J, Peuker E, Philipps B, Filler T (2002) Interindividual reproducibility in perioperative rotational alignment of femoral components in knee prosthetic surgery using the transepicondylar axis. Knee Surg Sports Traumatol Arthrosc 10:194–197
Ikeuchi M, Yamanaka N, Okanoue Y, Ueta E, Tani T (2007) Determining the rotational alignment of the tibial component at total knee replacement: a comparison of two techniques. J Bone Joint Surg Br 89:45–49
Insall JN (1993) Surgical techniques and instrumentation in total knee arthroplasty. In: Insall JN, Windsor RE, Scott WN, Kelly M, Aglietti P (eds) Surgery of the knee, 2nd edn. Churchill-Livingstone, New York, pp 739–804
Löer I, Plitz W (2003) Tibial malalignment of mobile-bearing prostheses–a simulator study. Orthopade 32:296–304
Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C (2007) A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am 89:236–243
Mizu-uchi H, Matsuda S, Miura H, Higaki H, Okazaki K, Iwamoto Y (2006) The effect of ankle rotation on cutting of the tibia in total knee arthroplasty. J Bone Joint Surg Am 88:2632–2636
Moreland JR (1988) Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res 226:49–64
Rodriguez JA, Bhende H, Ranawat CS (2001) Total condylar knee replacement: a 20-year followup study. Clin Orthop Relat Res 388:10–17
Rossi R, Bruzzone M, Bonasia DE, Marmotti A, Castoldi F (2010) Evaluation of tibial rotational alignment in total knee arthroplasty: a cadaver study. Knee Surg Sports Traumatol Arthrosc 18:889–893
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM (2002) Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Siston RA, Goodman SB, Patel JJ, Delp SL, Giori NJ (2006) The high variability of tibial rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 452:65–69
Sun T, Lu H, Hong N, Wu J, Feng C (2009) Bony landmarks and rotational alignment in total knee arthroplasty for Chinese osteoarthritic knees with varus or valgus deformities. J Arthroplasty 24:427–431
Suter T, Zanetti M, Schmid M, Romero J (2006) Reproducibility of measurement of femoral component rotation after total knee arthroplasty using computer tomography. J Arthroplasty 21:744–748
Şahin N, Atıcı T, Öztürk A, Özkaya G, Özkan Y, Avcu B (2012) Accuracy of anatomical references used for rotational alignment of tibial component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:565–570
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y (2002) Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 402:196–201
Whiteside LA, Arima J (1995) The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res 321:168–172
Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y (2001) Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty 16:493–497
Yoshioka Y, Siu DW, Scudamore RA, Cooke TD (1989) Tibial anatomy and functional axes. J Orthop Res 7(1):132–137
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Şahin, N., Atıcı, T., Kurtoğlu, Ü. et al. Centre of the posterior cruciate ligament and the sulcus between tubercle spines are reliable landmarks for tibial component placement. Knee Surg Sports Traumatol Arthrosc 21, 2384–2391 (2013). https://doi.org/10.1007/s00167-012-2120-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2120-5